Abstract
Study design:
Cross-sectional study.
Objectives:
Determine clinical factors associated with plasma C-reactive protein (CRP) in persons with chronic spinal cord injury (SCI).
Setting:
Veterans Affairs Medical Center in Boston, MA, USA.
Methods:
Participants provided a blood sample, completed a respiratory health questionnaire and underwent dual X-ray absorptiometry (DXA) to assess total and regional body fat. Linear regression models were used to assess cross-sectional associations with plasma CRP.
Results:
In multivariable models, factors associated with a higher CRP included a greater BMI, urinary catheter use, a respiratory illness in the past week and non-white race. Mean CRP also increased with decreasing mobility (motorized wheelchair >hand-propelled wheelchair >walk with an assistive device >walk independently). Results were similar when adjusting for percentage android, gynoid, trunk or total fat mass in place of BMI. Level and completeness of SCI was not associated with CRP in multivariable models.
Conclusions:
Clinical characteristics common in chronic SCI are associated with plasma CRP. These factors are more important than the level and completeness of SCI and some are potentially modifiable.
Similar content being viewed by others
Introduction
Chronic spinal cord injury (SCI) is characterized by clinical factors that promote systemic inflammation, including reduced mobility,1, 2, 3, 4, 5 accumulation of central fat6, 7, 8 and recurrent infections.9, 10 The linkage between systemic inflammation as assessed by C-reactive protein (CRP) and the development of atherosclerosis and coronary heart disease is well established.11 As individuals with SCI age, they are at increased risk for developing cardiovascular disease,12 which has become a major cause of mortality in the population with SCI.13, 14, 15, 16, 17, 18
Although elevated CRP levels have previously been described in chronic SCI,19, 20, 21, 22 to date, there has been a limited description of clinical factors that contribute. Slowly healing pressure ulcers in 34 men with SCI,9 urinary tract infections in 37 men,10 tetraplegia compared to paraplegia in 69 men and women23 and greater fat mass and body mass index (BMI) in 77 men and women have been associated with elevated CRP levels.24 In a previous report in 63 individuals, we found that mobility mode, a greater BMI, heart disease and a pressure ulcer reported in the past year were each associated with higher circulating CRP.25 A limitation of these previous reports, however, is a reduced ability to assess multiple covariates due to small sample sizes. The objective of this report is to assess the robustness of our previous findings in a new chronic SCI cohort with more than five times as many participants, as well as to assess the impact of additional factors, including fat mass assessed by dual x-ray absorptiometry (DXA) on levels of CRP.
Materials and methods
Subjects
Between August 2009 and April 2015 we recruited 360 individuals into a study of respiratory health among individuals with chronic SCI. Participants were recruited from patients receiving care at VA Boston, from the greater Boston area through advertisement, and by direct mail to persons who had received care at Spaulding Rehabilitation Hospital, Boston University Medical Center, were members of the National Spinal Cord Injury Association, or were subscribers to New Mobility Magazine. Individuals were eligible if they were 22 years of age or older, were 1 or more years post injury, had no other neuromuscular disease, did not have a tracheostomy and were able to breathe without chronic ventilatory support. Participants were eligible regardless of etiology of SCI, and testing was scheduled when subjects were free of acute illness. The Institutional Review Board at VA Boston Healthcare System approved the protocol, and informed consent was obtained. We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Neurological exam, stature and weight
SCI level and severity was assessed by exam and medical record review.26 Motor incomplete SCI included AIS C (most key muscles below the neurological level grade <3/5) or AIS D (most muscles below the neurological level grade⩾3/5). For analysis, participants were further grouped into cervical motor complete (AIS A or B) and cervical AIS C, high thoracic (T1–T6) complete (AIS A or B) and AIS C, others with T7 or below motor complete (AIS A or B) or AIS C, and all others (AIS D’s). Height was obtained by measuring the body length from top of the head to the heel of the subject in a supine position. Supine length was measured in 307 (91%) and obtained by self-report in 31 (9%) persons when contractures precluded accurate measurement (see statistical analysis). If required, wheelchairs were weighed with and without the participant, and wheelchair weight subtracted. In 5 persons, self-report of weight was used. BMI (kg m−2) was calculated from height and weight.
DXA for percentage body fat
A 5th generation GE Healthcare iDXA scanner was used to assess percentage total body, percentage trunk, percentage android and percentage gynoid fat using GE Lunar software analyzed by a certified clinical densitometrist (AAL). Daily quality assurance was performed utilizing a phantom. The trunk region was defined by cuts passing through the shoulders and extended inferiorly as close to the body as possible through the femoral necks. The lower boundary of the android region was a horizontal cut at the level of the iliac crests and the upper boundary extended upward to 20% of the distance between the pelvis and shoulders. For the gynoid region, the upper boundary was the iliac crests and the lower boundary included the pelvis and extended downward 1.5 times the height of the android region.
Health questionnaire
A questionnaire based on American Thoracic Society Division of Lung Diseases ATS DLD-7827 was used to obtain a history of cigarette smoking, comorbid medical diseases and statin use. Hypertension, diabetes and asthma were defined based on report of a diagnosis by a doctor, and chronic obstructive pulmonary disease (COPD) was defined as either doctor-diagnosed emphysema or chronic bronchitis. Heart disease was defined as treatment for ‘heart trouble’ reported in the 10 years prior to study entry. Participants were asked to report whether a chest illness kept them off work, indoors at home or in bed in the previous one and three years, whether they had had a respiratory illness in the past week, whether they currently had a urinary tract infection (UTI) or a skin ulcer, or whether they had experienced either in the past 1 and 3 years, how they usually passed urine, and whether they received regular dental care. Usual mobility mode (>50% of the time) was ascertained in four categories: motorized wheelchair use, hand-propelled wheelchair use, walk with aid such as crutch or cane, or walk without assistance.
Biochemical analyses
Plasma samples were drawn into an EDTA tube and immediately delivered to a core blood research laboratory. The samples were centrifuged for 15 min at 2600 r.p.m. (1459 g) at 4 °C and stored at −80 °C until batch analysis. High-sensitivity CRP concentrations using an immunoturbidimetric assay were determined at the Clinical and Epidemiologic Research Laboratory, Department of Laboratory Medicine at Children’s Hospital in Boston. This assay has a sensitivity of 0.03 mg l−1. The day-to-day variability of the assay at concentrations of 0.91, 3.07 and 13.38 mg l−1 are 2.81, 1.61 and 1.1%, respectively.
Statistical analysis
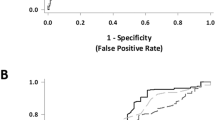
We excluded persons without a detectable SCI level (n=3), history of stroke (n=2), incomplete data collection (n=6), inability to obtain blood (n=6), incomplete data on body composition (n=4) or without CRP results (n=1), leaving a sample size of 338 participants. There were 26 subjects who participated in our previous study (2004–2005)25 who were retested. Natural log-transformation of CRP was used to meet modeling assumptions. General linear models (PROC GLM, SAS version 9.4) were used to assess determinants of natural log CRP. A Tukey adjustment was used for multiple comparisons. Trends across percentage-fat and BMI quartiles were assessed using the median values, and trends for mobility and SCI categories were assessed by assigning ordinal numbers. Variables significant in univariable models at the 0.10 level or less were included in multivariate models. We a priori assessed characteristics associated with infection (i.e., ulcer history) and considered effects of comorbid diseases as potential confounders.
Results
Participant characteristics
Participant characteristics are presented in Table 1 overall and by primary mobility mode. The mean ±standard deviation age and injury duration were 54.1±14.4 years and 17.3±13.3 years, respectively (Table 1). The majority of participants were male (82%) and white (86%). When screened by a questionnaire at the time of testing, a mild cold or other respiratory illness was reported by 26 persons (7.7%) in the past week. A history of skin ulcers, urinary tract infections and catheter use was more common among motorized and hand-propelled wheelchair users. There were 83 people (25%) with CRP levels <1 mg l−1 (defined as low cardiovascular risk),11 105 (31%) with CRP levels of 1–3 mg l−1 and 150 (44%) people with CRP levels of >3 mg l−1. There were 54 (16%) people with very high CRP levels (>10 mg l−1). The distribution of natural log CRP was normally distributed (Shapiro–Wilks test W=0.996, P=0.640), and there was no evidence of outliers.
Univariable associations
In univariable models, age, sex, injury duration, smoking status and pack years of smoking, sex, statin use, dental care and comorbidities were not associated with CRP (Table 2). Both mobility mode and level and completeness of SCI were statistically significantly associated with CRP, with the highest CRP levels observed among motorized wheelchair users and among cervical motor complete and AIS C SCI with a significant linear trend across mobility and SCI level and completeness categories (Table 2). Persons who reported a current skin ulcer or a UTI or reported either in the past one and three years had higher CRP levels compared to persons without these conditions. Persons who used a condom catheter, a chronic indwelling catheter or used periodic catheterization had CRP values that were not statistically significantly different from one another (P=0.551–0.999), but each was statistically significantly different from participants who did not use a catheter. Therefore, catheter use was considered as a dichotomous variable. Catheter use was strongly associated with report of a current UTI, as 21 out of the 25 persons with a current UTI used a catheter. Persons who reported a respiratory illness (4.10; 95% CI: 2.28, 5.01 mg l−1) in the past week had greater CRP values compared to persons without an illness (2.54; 95%CI: 2.14, 2.97 mg l−1, P=0.096). Participants who were self-identified as being white had lower CRP values compared to non-white participants (P=0.038). Each measure of adiposity was also statistically significantly positively associated with CRP, with a significant trend across quartiles (Table 3).
Multivariable associations
Due to the high level of collinearity between the DXA-derived measures of adiposity (Pearson r=0.705–0.979, P<0.0001) and a significant correlation between these measures with BMI (r=0.393–0.689, P<0.0001), we created five multivariable models including each adiposity measure separately with other predictors (Table 4). Each adiposity measure (including BMI) was statistically significantly associated with CRP levels in multivariate models (P<0.001). There was a significant positive linear trend across adiposity measure quartiles (not shown), so the continuous measures were used in the final models. Urinary catheter use also remained statistically significantly associated with CRP (P=0.002–0.013), with a better model fit than either current UTI or UTI in the previous year. Participants with a respiratory illness in the week before testing (usually a mild cold) had significantly greater CRP levels (P=0.005–0.015), as did those who were identified as non-white (P=0.001–0.041). In each model (Table 4), participants who reported a current ulcer had a higher CRP compared to persons without an ulcer that was not statistically significant (P=0.096–0.173). Associations with an ulcer reported in the past year (P=0.254–0.450) were weaker and not significant.
In four multivariable models (Table 4), there was a significant linear trend across mobility categories with CRP (P<0.001–0.018), and a suggestive relationship in an additional model (P=0.069). When included in these models, SCI level and completeness was not a statistically significant predictor of CRP (P=0.554–0.974).
Effect of chronic disease
In order to account for effects of comorbid diseases on CRP as potential confounders, we individually added heart disease, diabetes, hypertension, COPD, asthma and any obstructive lung disease (asthma or COPD) into the final multivariable models. The effects of measures of adiposity, urinary catheter, respiratory illness in the past week, current skin ulcer, race and mobility mode did not meaningfully change (data not shown). Heart disease was significantly associated with a greater CRP (P=0.021–0.039) in all models as was hypertension in the model that included gynoid fat (P=0.015). Hypertension in other models (P=0.100–0.157), diabetes (P=0.198-0.770), COPD (P=0.786–0.976), asthma (P=0.163–0.372) and any obstructive lung disease (asthma or COPD) (P=0.305–0.440) were not significantly associated with CRP.
Discussion
In this cross-sectional study in a cohort of individuals with chronic SCI, we found that measures of adiposity (BMI, percentage total body fat, percentage trunk fat, percentage android fat and percentage gynoid fat), mobility mode, catheter use, race and respiratory illness in the past week were all independently associated with circulating levels of CRP. There was a strong linear association found between SCI level and CRP in univariable models (P<0.0001) that was not evident after adjustment for mobility mode. We previously reported similar results in a smaller study (n=63) in our earlier chronic SCI cohort, indicating that these findings are reproducible in the SCI population.25 The effects of clinical factors identified in multivariable models were not affected after adjustment for comorbidities that included heart disease, hypertension, diabetes, COPD and asthma. Although heart disease history was significantly associated with a higher CRP value in multivariate models, it did not confound the relationship between the clinical factors included in the multivariable models and CRP.
Pressure ulcers and UTIs have been previously associated with an elevated CRP level.9, 10 The participants in this cohort were tested when they were feeling well and were able to sit upright for study-related procedures. This likely explains why relatively few persons reported a current skin ulcer (11.2%) and its weak association with CRP in the multivariate models. Considerably more persons (25.2%) reported a skin ulcer in the past year. Similarly, few persons in our cohort reported a current UTI (7.4%), but many reported having a UTI in the past year (40.2%). Both chronic, intermittent and condom catheter use are known correlates of chronic bacteriuria and pyuria,28 which is most likely responsible for the higher CRP values associated with catheter use.
We directly assessed percent fat in the android, gynoid and trunk regions, as well as total body fat by DXA scan. In SCI, due to a decrease in lean mass and increase in fat mass and in central (truncal) fat,6, 7, 29 BMI may not accurately assess adiposity.30 However, we found similar effects of BMI and other measures of adiposity on CRP levels in multivariate models, most likely attributable to the high degree of correlation between the fat measures.
Our findings support the hypothesis that physiologic changes that occur following SCI attributable to decreased mobility, bladder dysfunction and skin ulcers contribute to CRP and systemic inflammation and, therefore, potentially future risk of cardiovascular disease. Many studies in persons without SCI have found higher levels of CRP to be associated with lower levels of physical activity.1, 2, 3, 31 Evidence that chronic or recurrent infection may be associated with cardiovascular disease comes from positive associations between periodontal disease and carotid intima-media thickness,32 and the timing of a myocardial infarction and a preceding systemic respiratory tract33 or urinary tract infection34 in persons without chronic SCI.
A considerable stength of this study is the use of a comprehensive standardized approach allowing the consideration of multiple factors potentially associated with CRP in a large chronic SCI cohort. Limitations include reliance on self-report of current ulcer, UTI and of chronic medical conditions. However, we have previously validated the use of self-report of chronic medical conditions in this population.14 Misclassification would make it more difficult to detect the true associations with CRP.
Our study findings support the importance of studying modifiable factors in chronic SCI that can impact health. A longitudinal study is needed to assess the relationship between factors identified, chronic elevations in CRP and subsquent effects on cardiovacular health. Addressing modifiable factors related to obesity, reduced physical actvity and recurrent infection could potentially help in lowering the risk of cardiovascular disease among those with chronic SCI.
References
Kasapis C, Thompson PD . The effects of physical activity on serum C-reactive protein and inflammatory markers: a systematic review. J Am Coll Cardiol 2005; 45: 1563–1569.
Nicklas BJ, You T, Pahor M . Behavioural treatments for chronic systemic inflammation: effects of dietary weight loss and exercise training. CMAJ 2005; 172: 1199–1209.
Fischer CP, Berntsen A, Perstrup LB, Eskildsen P, Pedersen BK . Plasma levels of interleukin-6 and C-reactive protein are associated with physical inactivity independent of obesity. Scand J Med Sci Sports 2007; 17: 580–587.
Penninx BW, Kritchevsky SB, Newman AB, Nicklas BJ, Simonsick E, Rubin S et al. Inflammatory markers and incident mobility limitation in the elderly. J Am Geriatr Soc 2004; 52: 1105–1113.
Ferrucci L, Harris TB, Guralnik JM, Tracy RP, Corti MC, Cohen HJ et al. Serum IL-6 level and the development of disability in older persons. J Am Geriatr Soc 1999; 47: 639–646.
Spungen AM, Adkins RH, Stewart CA, Wang J, Pierson RN Jr, Waters RL et al. Factors influencing body composition in persons with spinal cord injury: a cross-sectional study. J Appl Physiol 2003; 95: 2398–2407.
Maggioni M, Bertoli S, Margonato V, Merati G, Veicsteinas A, Testolin G . Body composition assessment in spinal cord injury subjects. Acta Diabetol 2003; 40 (Suppl 1): S183–S186.
Edwards LA, Bugaresti JM, Buchholz AC . Visceral adipose tissue and the ratio of visceral to subcutaneous adipose tissue are greater in adults with than in those without spinal cord injury, despite matching waist circumferences. Am J Clin Nutrition 2008; 87: 600–607.
Segal JL, Gonzales E, Yousefi S, Jamshidipour L, Brunnemann SR . Circulating levels of IL-2R, ICAM-1, and IL-6 in spinal cord injuries. Arch Phys Med Rehabil 1997; 78: 44–47.
Frost F, Roach MJ, Kushner I, Schreiber P . Inflammatory C-reactive protein and cytokine levels in asymptomatic people with chronic spinal cord injury. Arch Phys Med Rehabil 2005; 86: 312–317.
Pearson TA, Mensah GA, Alexander RW, Anderson JL, Cannon RO, Criqui M et al. Markers of inflammation and cardiovascular disease. Circulation 2003; 107: 499–511.
LaVela SL, Evans CT, Prohaska TR, Miskevics S, Ganesh SP, Weaver FM . Males aging with a spinal cord injury: prevalence of cardiovascular and metabolic conditions. Arch Phys Med Rehabil 2012; 93: 90–95.
DeVivo MJ, Krause JS, Lammertse DP . Recent trends in mortality and causes of death among persons with spinal cord injury. Arch Phys Med Rehabil 1999; 80: 1411–1419.
Garshick E, Kelley A, Cohen SA, Garrison A, Tun CG, Gagnon D et al. A prospective assessment of mortality in chronic spinal cord injury. Spinal Cord 2005; 43: 408–416.
Osterthun R, Post MWM, van Asbeck FWA, van Leeuwen CMC, van Koppenhagen CF . Causes of death following spinal cord injury during inpatient rehabilitation and the first five years after discharge. Spinal Cord 2014; 52: 483–488.
Rabadi MH, Mayanna SK, Vincent AS . Predictors of mortality in veterans with traumatic spinal cord injury. Spinal Cord 2013; 51: 784–788.
Sabre L, Rekand T, Asser T, Korv J . Mortality and causes of death after traumatic spinal cord injury in Estonia. J Spinal Cord Med 2013; 36: 687–694.
Whiteneck GG, Charlifue SW, Frankel HL, Fraser MH, Gardner BP, Gerhart KA et al. Mortality, morbidity, and psychosocial outcomes of persons spinal cord injured more than 20 years ago. Paraplegia 1992; 30: 617–630.
Nash MS, Tractenberg RE, Mendez AJ, David M, Ljungberg IH, Tinsley EA et al. Cardiometabolic syndrome in people with spinal cord injury/disease: guideline derived and nonguideline risk components in a pooled sample. Arch Phys Med Rehabil 2016; 97: 1696–1705.
Wang TD, Wang YH, Huang TS, Su TC, Pan SL, Chen SY . Circulating levels of markers of inflammation and endothelial activation are increased in men with chronic spinal cord injury J Formosa Med Assoc. 2007; 106: 919–928.
Huang CC, Liu CW, Weng MC, Chen TW, Huang MH . Assocation of C-reactive protein and insulin resistance in patients with chronic spinal cord injury. J Rehabil Med 2008; 40: 819–822.
Liang H, Mojtahedi MC, Chen D, Braunschweig CL . Elevated C-reactive protein associated with decreased high-density lipoprotein cholesterol in men with spinal cord injury. Arch Phys Med Rehabil 2008; 89: 36–41.
Gibson AE, Buchholz AC, Ginis KM . C-Reactive protein in adults with chronic spinal cord injury: increased chronic inflammation in tetraplegia vs paraplegia. Spinal Cord 2008; 46: 616–621.
Laughton GE, Buchholz AC, Ginis KM, Goy RE . Lowering body mass index cutoffs better identifies obese persons with spinal cord injury. Spinal cord 2009; 47: 757–762.
Morse LR, Stolzmann K, Nguyen HP, Jain NB, Zayac C, Gagnon DR et al. Association between mobility mode and C-reactive protein levels in men with chronic spinal cord injury. Arch Phys Med Rehabil 2008; 89: 726–731.
Kirshblum SC, Waring W, Biering-Sorensen F, Burns SP, Johansen M, Schmidt-Read M et al. Reference for the 2011 revision of the International Standards for Neurological Classifications of Spinal Cord Injury. J Spinal Cord Med 2011; 34: 547–554.
Ferris BG . Epidemiology Standardization Project (American Thoracic Society). Am Rev Respir Dis 1978; 188: 1–120.
Nicolle LE, Bradley S, Colgan R, Rice JC, Schaeffer A, Hooton TM . Infectious Diseases Society of America guidelines for the diagnosis and treatment of asymptomatic bacteriuria in adults. Clinical Infectious Diseases 2005; 40: 643–654.
Jones LM, Legge M, Goulding A . Healthy body mass index values often underestimate body fat in men with spinal cord injury. Arch Phys Med Rehabil 2003; 84: 1068–1071.
Cirnigliaro CM, LaFountaine MF, Dengel DR, Bosch TA, Emmons RR, Kirshblum SC et al. Visceral adiposity in persons with chronic spinal cord injury determined by dual energy x-ray absorptiometry. Obesity 2015; 23: 1811–1817.
Mora S, Lee IM, Buring JE, Ridker PM . 2006. Association of physical activity and body mass index with novel and traditional cardiovascular biomarkers in women. JAMA 2006; 295: 1412–1419.
Aarabi G, Eberhard J, Reissmann D, Heydecke G, Seedorf U . Interaction between periodontal disease and atherosclerotic vascular disease-fact or fiction? Atherosclerosis 2015; 241: 555–560.
Barnes M, Heywood AE, Mahimbo A, Rahman B, Newall AT, Macintyre CR . Acute myocardial infarction and influenza: a meta-analysis of case–control studies. 2015; 101: 1738–1747.
Sims JB, de Lemos JA, Maewal P, Warner JJ, Peterson GE, McGuire DK . Urinary tract infection in patients with acute coronary syndrome: a potential systemic inflammatory connection. Am Heart J 2005; 149: 1062–1065.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest. Supported by VA Rehabilitation Research and Development Merit Review Grant B6618R and I01 RX000792 from the U.S. Department of Veterans Affairs Rehabilitation Research and Development Service; and NIH Grant R01 AR059270. The contents do not represent the views of the U.S. Department of Veterans Affairs or the United States Government.
Rights and permissions
About this article
Cite this article
Goldstein, R., Walia, P., Teylan, M. et al. Clinical factors associated with C-reactive protein in chronic spinal cord injury. Spinal Cord 55, 1088–1095 (2017). https://doi.org/10.1038/sc.2017.81
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2017.81
This article is cited by
-
Serum C-reactive protein is an early, simple and inexpensive prognostic marker for the progression of intramedullary lesion on magnetic resonance imaging from acute to subacute stage in patients with spinal cord injury
Spinal Cord (2021)
-
Guideline for the identification and management of cardiometabolic risk after spinal cord injury: a case of unsubstantiated recommendations
Spinal Cord Series and Cases (2019)
-
Clinical associations with telomere length in chronic spinal cord injury
Spinal Cord (2019)
-
FEV1 and FVC and systemic inflammation in a spinal cord injury cohort
BMC Pulmonary Medicine (2017)