Abstract
Design:
Retrospective and prospective observational.
Objective:
Analyse causes of death after traumatic spinal cord injury (tSCI) in persons surviving the first year post injury, and establish any trend over time.
Setting:
Two spinal centres in Great Britain.
Methods:
The sample consisted of 5483 patients with tSCI admitted to Stoke Mandeville and Southport spinal centres who were injured between 1943 and 2010, survived first year post injury, had residual neurological deficit on discharge and were British residents. Mortality information, including causes of death, was collected up to 31 December 2014. Age-standardised cause-specific mortality rates were calculated for selected causes of death, and included trends over time and comparison with the general population.
Results:
In total, 2322 persons (42.3% of the sample) died, with 2170 (93.5%) having a reliable cause of death established. The most frequent causes of death were respiratory (29.3% of all certified causes), circulatory, including cardiovascular and cerebrovascular diseases (26.7%), neoplasms (13.9%), urogenital (11.5%), digestive (5.3%) and external causes, including suicides (4.5%). Compared to the general population, age-standardised cause-specific mortality rates were higher for all causes, especially skin, urogenital and respiratory; rates showed improvement over time for suicides, circulatory and urogenital causes, no significant change for neoplasms, and increase for skin and respiratory causes.
Conclusions:
Leading causes of death after tSCI in persons surviving the first year post injury were respiratory, circulatory, neoplasms and urogenital. Cause-specific mortality rates showed improvement over time for most causes, but were still higher than the general population rates, especially for skin, urinary and respiratory causes.
Similar content being viewed by others
Introduction
Life expectancy following spinal cord injury (SCI) has improved significantly since World War II owing to advances in medicine, emergency services and life-long care.1, 2, 3, 4, 5 As people with SCI live longer, the leading causes of death start showing a shift from the typical SCI-related mortality towards that of the ageing general population.1, 2, 3, 4, 6, 7, 8 However, the risk of dying is still higher in SCI than in the general population for most causes, and especially for those that are SCI-related.5, 6, 7, 8, 9
Having the latest information about causes of death is a necessary prerequisite for developing preventative and therapeutic measures as part of the life-long care after SCI, with the aim of improving longevity and quality of life of people with SCI.
The only study in the UK, by Frankel et al., 1998, included persons injured between 1943 and 1990 and analysed their long-term survival and causes of death up to 1993.1 The current work is an extension of that study, looking at causes of death in the updated sample and establishing trends over the 70-year study period 1944–2014.
Setting
The study took place at the two oldest British spinal centres—the National Spinal Injuries Centre at Stoke Mandeville Hospital, Buckinghamshire Healthcare NHS Trust and the North West Regional Spinal Injuries Centre at Southport Hospital, Southport and Ormskirk NHS Trust.
Methods
Study design
Retrospective medical records' data review and retrospective and prospective mortality data collection.
Sample
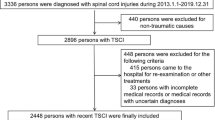
The sample consisted of all patients with traumatic SCI who were injured between 1943 and 2010, admitted to Stoke Mandeville and Southport spinal centres, survived the first year post injury, had residual neurological deficit on discharge and were British residents.
The sample was identified through a thorough medical record review at the two spinal centres, with records dating back to 1944 at Stoke Mandeville and 1948 in Southport.
Data collection
Patient demographic and injury information was collected from the medical records at the two spinal centres.
Survival status up to and including 31 December 2014 and death certificates for the deceased were supplied by the Medical Research Information Service, Health and Social Care Information Centre (HSCIC) on behalf of the UK Office for National Statistics (ONS). Data exchange was done through a secure HSCIC Data Exchange Service. For those individuals known to have died, causes of death were identified from the death certificates and, when available, from autopsy reports. For those who died at one of the spinal centres, additional information was collected from their medical notes at the centre, where available. The UK ONS also produced national mortality figures for the general population of England and Wales.
Data analysis
Data analyses were performed on an anonymised database using Statistical Package for the Social Sciences (SPSS), Version 17 (SPSS Inc., Chicago, IL, USA), SPSS version 22 (International Business Machines (IBM) Corporation, Armonk, NY, USA) and Statistical Analysis System (SAS) (SAS Institute Inc., Cary, NC, USA) programmes.
Descriptive statistics were used for presenting the sample.
For analysis purposes, the sample was divided into three injury severity groups, based on the International Standards for Neurological Classification of Spinal Cord Injury.10 In cases where a complete neurological examination according to the International Standards for Neurological Classification of Spinal Cord Injury was not performed and recorded (most cases admitted before the 1990s), the classification was done according to the Frankel classification.11 The three groups were as follows: those with tetraplegia and American Spinal Injuries Association Impairment Scale (AIS) or Frankel grade A, B or C (tetra ABC), those with paraplegia and AIS/Frankel grade A, B or C (para ABC), and those with incomplete AIS/Frankel grade D injuries regardless of the level (all Ds). For more detailed analysis, the tetra ABC group was further divided into three subgroups as follows: those on either full-time or part-time permanent mechanical ventilation or phrenic nerve stimulation (ventilator-dependent), the high tetraplegia (C1-C4 ABC) group, and the low tetraplegia (C5-C8 ABC) group.
Causes of death were reported in percentages for all the deceased, and separately by neurological grouping (as defined above), by study period (1944–1969, 1970–1989, 1990–2004, 2005–2014), by age at death grouping (0–29, 30–44, 45–59 and 60+) and by time since injury grouping (1–5, 6–10, 11–30 and 30+ years). Because of a relatively small number of SCI deaths in the 1944–1969 period, it was merged with the 1970–1989 period for the combined analysis by neurological grouping and study period, so that the three periods were 1944–1989, 1990–2004 and 2005–2014.
Causes of death were coded in the International Classification of Diseases version 9 (ICD-9) codes up to and including year 2000 and in ICD-10 codes since 2000. For analysis purposes, the causes of death were grouped according to ICD-10.12
In cases with multiple causes of death listed on death certificates, the cause of death used in the study was the underlying cause, which is defined by the World Health Organization as the disease or injury that initiated the train of events leading directly to death, or the circumstances of the accident or violence which produced the fatal injury.13 The same definition was used by the UK ONS when reporting the general population causes of death, as well as by other SCI mortality studies.4, 7, 8
If septicaemia was listed as the primary cause of death on the death certificate, every attempt was made to identify the source of septicaemia from death certificates and medical records, and code it under that organ system. The same was done with all available old death certificates from the original study.1 Only if there was no obvious source of septicaemia was it left as the underlying cause of death as ‘septicaemia of unclear origin’.
For suicide as the underlying cause of death, the UK ONS 2014 definition was used, by which suicide includes intentional self-harm, as well as injury/poisoning of undetermined intent for persons over the age of 14 years.
Age-standardised cause-specific mortality rates and 95% confidence limits were calculated for the selected causes of death for each time period by applying age-cause-specific mortality rates to the age distribution of the 2013 European Standard Population. This process adjusts for the fact that the population since 2005 is older than that in previous time periods and would have artificially higher cause-specific mortality rates without adjusting for its older average age. The process of direct calculation of age-standardised rates is analogous to the indirect adjustment of age differences achieved by calculating standardised mortality ratios. The three periods for this analysis were the same as for the combined frequency analysis described above—1944–1989, 1990–2004 and 2005–2014. These age-standardised rates were then used to assess trends over time, and to compare rates for the latest time period among persons with SCI to those of the general population of comparable age. The general population figures used for comparison were age-standardised cause-specific mortality rates for England and Wales 2014, which were weighted to match the gender distribution in the SCI group for the latest time period (79.2% male and 20.8% female). Mortality rates were expressed in number of deaths per 100 000 persons at risk per year.
Statement of ethics
The study was approved by Berkshire Research Ethics Committee (REC), REC reference number 11/H0505/1.
We certify that all applicable institutional and governmental regulations concerning the ethical use of patient identifiable data were followed during the course of this research.
Results
Sample characteristics
The total sample included 5483 persons with traumatic SCI—3179 from the original survival study1 and 2304 added in the current follow-up study. The mean age at injury for the total updated sample was 35.12 years (range 0.5–90.99, median 30.68); 79.7% of the sample was male, 31.1% had tetraplegia ABC (1.4% ventilator-dependent, 6.3% C1–C4 ABC and 23.4% C5–C8 ABC), 41.2% had paraplegia ABC and 27.7% had incomplete D lesion. Demographic and injury characteristics changed over the 70-year study period, with the average age at injury increasing over time, as well as the proportion of females and of cervical injuries, particularly high cervical injuries. A detailed description of the sample can be found in our recently published life-expectancy paper.5
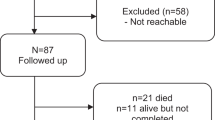
On 31 December 2014, there were 2958 persons (54% of the sample) still alive, 2322 (42.3%) had died and 203 (3.7%) were lost to follow-up (mainly because of not registering with the local medical and social care services, or because of moving abroad). Of the 2322 deceased, the majority (65.3%) died in hospital, 22% at home, 8.2% in nursing home, 2.4% in hospice and the remaining 2.1% elsewhere. Most in-hospital deaths, especially in the later study period, occurred in patients’ local hospitals and not at the spinal centres. For 2170 (93.5% of all the deceased) patients, a reliable cause of death could be established from the death certificates, supplemented with information from medical notes for those who died at spinal centres, and from autopsy reports, when available. Only 22.9% of the deceased had an autopsy report, mainly in the earlier decades (32% in the 1944–1969 study period, 26% in 1970–1989, 24.1% in 1990–2004 and 12.6% in the 2005–2014 period).
Causes of death
Over the entire study period, the most frequent causes of death were respiratory (29.3% of all documented causes of death), circulatory, including cardiovascular and cerebrovascular diseases (26.7%), neoplasms (13.9%), urogenital (11.5%), digestive (5.3%) and external causes, including suicide, self-harm of undetermined intent, crime and accidents (4.5%). The ranking order for the leading causes was the same for both genders, with a slightly higher percentage of men than women dying of circulatory causes (27.7 vs 22.6%), and a higher percentage of women dying of respiratory causes (34.2 vs 28.1%), but the differences were not quite statistically significant (chi-square test, P=0.07).
Table 1 shows causes of death for the entire 70 years' observation and by the four study periods (decades of death), as well as main demographic and SCI characteristics of the deceased for each time period.
Analysed over time, leading causes of death in the 1944–1969 period were urogenital (32.8%), circulatory (24.2%), respiratory (17.2%) and skin-related (7.8%); those in the 1970–1989 period were circulatory (27.8%), respiratory (24.7%), urogenital (18.2%) and neoplasms (12.8%); those in the 1990–2004 period were circulatory (30.9%), respiratory (29.9%), neoplasms (14.2%) and urogenital (6.1%), and those in the 2005–2014 period were respiratory (34.1%), circulatory (21.8%), neoplasms (15.9%) and urogenital (8.7%).
The most frequent respiratory causes were respiratory tract infections (23.5% of all certified deaths), mainly pneumonia and bronchopneumonia, including sepsis and pneumonia listed as multiple causes. In 2.9% patients, the underlying cause of death was a chronic obstructive pulmonary disease, mainly chronic bronchitis and emphysema, and the remaining 2.9% were other respiratory causes, which included respiratory arrest, respiratory failure and a few post-procedural disorders and tracheostomy malfunctions.
Heart diseases were the most frequent circulatory cause of death, accounting for 18.4% of all deaths overall. Because it was not always possible to conclude, from death certificates alone, whether heart disease was ischaemic or non-ischaemic, they were not presented separately in the table. However, 65% of all heart causes were reported as ischaemic in death certificates (myocardial infarction, atherosclerotic heart disease) and of the remaining 35% (cardiomyopathy, hypertensive heart disease, heart failure and cardiac arrest), some were likely to have been ischaemic, too; however, in the absence of a post-mortem examination, this remains uncertain. The same is true of the cerebrovascular causes (6.3% of all deaths); most of them were reported as stroke or cerebrovascular incidents, but not specified as haemorrhage or infarction. Pulmonary embolism was the cause of death in <1% of cases overall, and the remaining 1.1% of circulatory causes were mainly ruptured aortic aneurism and a few cases of severe peripheral vascular diseases.
The most frequent neoplasms for the entire sample were of the digestive, respiratory and urinary system. The ranking was the same for the male gender, with digestive system neoplasms accounting for 25.7%, respiratory system neoplasms accounting for 24.9% and urinary system neoplasms accounting for 18.7% of all neoplasms in males. For the female gender, the most frequent was breast cancer (23%), followed by digestive (21.3%) and respiratory (11.5%) system neoplasms. Bladder cancer accounted for 9.6% of all neoplasms. Ten percent of all neoplasms were of unknown primary site.
Among urogenital causes, urinary tract infections, including urosepsis, were the most frequently reported cause of death, followed closely by renal failure.
Digestive causes included those affecting the upper gastrointestinal tract (perforated gastric and duodenal ulcers), the biliary system (alcoholic and other cirrhosis, liver failure, pancreatitis) and the lower gastrointestinal tract (bowel obstruction, volvulus and bowel perforation).
Among external causes of death, the most frequent were suicides, which, combined with self-harm of undetermined intent, in line with the UK ONS definition of suicide, accounted for 3.2% of all deaths overall (3.5% in males and 2.4% in females). The most common suicide methods were drug overdose, other poisoning, hanging, drowning, fall (jump from height) and firearms. Deaths due to criminal activities were very rare, only two cases, both in men, and both lethal gunshot wounds. Accidents included fire, falls, drowning and road traffic accidents.
Sepsis was reported as the primary cause of death in 2% of all death certificates. In 0.7%, the source of infection could be identified and those deaths were classified under relevant organ system (most frequently urinary, respiratory and skin), and the remaining 1.3% under sepsis of unclear origin. Further 6.6% of death certificates had sepsis listed as a secondary cause, and 0.7% under multiple causes.
The 1.2% of deaths due to ill-defined causes were reported as ‘unclear’, ‘unascertained’ or ‘open verdict’ in the death certificates.
Analysed by SCI severity, respiratory diseases were the leading cause of death in persons with tetraplegia ABC (42.4%), and circulatory diseases in persons with paraplegia ABC (27.7%) and in functionally incomplete SCI—all Ds (33.4%) (Table 2). In persons with high-level tetraplegia, respiratory causes accounted for more than half of all causes of death—53.2% in ventilator-dependent tetraplegia and 52.2% in C1–C4 ABC tetraplegia. A combined analysis by level of injury and study period showed that in persons with tetraplegia (ventilated, C1–C4 ABC and C5–C8 ABC), respiratory causes ranked first throughout the study. In persons with functionally complete paraplegia (para ABC), urinary causes ranked first in the early decades and were replaced by circulatory diseases as the leading cause of death in later decades. In persons with functionally incomplete injury (all Ds), circulatory diseases ranked first until the latest time period, when they were replaced by respiratory causes (Table 3).
The proportion and ranking of causes of death also varied when analysed by age at death and by time since injury (both P<0.01). In the 0–29-year-old group, the leading causes of death were external causes, including suicides (28.4% of all deaths in this group). In all other age groups, the leading causes were respiratory, followed by circulatory, the percentage of both rising with age. The proportion of circulatory causes, but not respiratory, also rose with time since injury, so that circulatory causes ranked first in all groups injured for more than 10 years. The proportion of external causes of death, on the other hand, declined with both age and time post injury. (Two tables, with analyses by age and by time since injury, are available online as Supplementary Information.)
Cause-specific mortality rates
Table 4 shows cause-specific mortality rates for the selected causes of death by the three study periods (1944–1989, 1990–2004 and 2005–2014) in the SCI sample, as well as the latest general population rates for England and Wales for the year 2014. Over time, there was a marked reduction in suicide rate and in circulatory causes of death rate. Urogenital and skin causes showed a good decrease in mortality rates initially, but increased in the latest time period, especially skin rates. Cancer rates showed minimal improvement, whereas no progress was noted in respiratory or the category of all other causes combined. Comparing the latest SCI period with the general population rates, there was only a small excess of cancer rate in the SCI group (14% higher). All other rates were significantly elevated compared to the general population, and especially for skin (30 times higher), urogenital (12 times higher) and respiratory causes (five times higher). Rates for suicide were 2.7 times higher, for circulatory causes two times higher and for all other causes 1.9 times higher than those in the general population.
Discussion
The aim of the study was to investigate causes of death in people surviving the first year post tSCI in Great Britain and to establish any trend over time.
When interpreting the study results, it is worth noting that the sample demographic and SCI characteristics changed over the 70-year study period, as this might have had an effect on causes of death (older age at injury and at death, longer time since injury, higher proportion of females and of cervical injuries, particularly high cervical injuries).
For the overall 70-year study period, the leading causes of death were respiratory, circulatory, neoplasms and urogenital. The proportion of individual causes differed over time: in the early study decades, urinary causes ranked first, but were only fourth in the latest decades, whereas respiratory causes moved from the third to the first place. In the early decades, skin-related causes ranked fourth, but more than halved in proportion since then.
Causes of death also varied by level and completeness of injury, so that respiratory diseases were the leading cause of death in persons with tetraplegia throughout the study and circulatory disease in persons with paraplegia and functionally incomplete SCI (all Ds) group (Tables 2 and 3).
The general population mortality figures for England and Wales showed the following ICD-10 broad disease groups with the largest numbers of deaths in 2014: cancers (neoplasms) accounted for 29% of all deaths in that year, followed closely by circulatory diseases (including heart disease and strokes) with 27% of all deaths, and respiratory diseases (including pneumonia) with 13% of all deaths. Comparing the SCI results for the latest study period 2005–2014 with this, the same three disease groups were the leading causes of death in our study, but in a different order and proportion: respiratory were first, with 34.1% of all deaths in that period, circulatory came second with 21.8% and neoplasms were third with 15.9%.
Selected age-standardised cause-specific mortality rates shown over time in Table 4 give a more precise picture of causes of death, and especially of their trends, than just pure frequencies, as rates are adjusted for age differences over time and take into account exposure of the whole observed sample over the given time period. The selected rates had a mainly good trend, towards reduction, especially for suicides, urogenital and circulatory diseases, and, to a lesser extent, for neoplasms. Rates for urogenital causes saw a dramatic reduction by the end of the twentieth century, but then showed a slight increase in the latest study period, even though they were still less than half of what they had been in the earliest study period. Rates for skin-related causes, namely pressure sores, represent a small proportion of all deaths, but, after the initial improvement, showed a marked increase in the latest study decade. Skin- and respiratory-related causes both had higher mortality rates at the end of the study than at the beginning.
The reduction in the rate of circulatory causes of death in the later study decades is very likely due to increased awareness, prevention, screening and early intervention in cardiovascular and cerebrovascular diseases implemented nationwide, including persons with SCI.
Similarly, the reduction during the middle study period in causes of death associated with spinal cord, such as urinary and skin, can be, at least partly, attributed to improved long-term care after spinal injury, including regular follow-ups at the spinal centres, prevention and timely intervention for SCI-related complications. Similar trends were found in studies that spanned over several decades.1, 2, 6, 7, 8 However, the risk of dying of SCI-related causes was still much higher than that in the general population, and of particular concern is the rise in mortality rates for skin and urinary causes in the latest study decade. As most of them were infections, they will be addressed in more detail with the infections later in the discussion.
Rates for respiratory causes showed no improvement and were higher at the end of study than at the beginning, even though they did show a decreasing trend in the latest study period (from 712.4 up to 878.6 and down to 793.3). A likely contributing factor for an increase in respiratory causes over the course of the study was the rise in the percentage of persons with tetraplegia, particularly in the middle study period. In addition to this, respiratory arrest and pneumonia, especially in the elderly, were sometimes given as cause of death in the absence of another clear cause; thus, respiratory causes are probably somewhat over-reported in death certificates.
Comparing the latest study period only (2005–2014) to the general population cause-specific mortality rates for 2014 (Table 4), there was only a small excess of cancer in SCI, probably due to bladder cancer, which accounted for 9.6% of all cancers in our study. This would be consistent with the USA SCI Model System findings of standardised mortality ratio (SMR) of 6.7 for bladder cancer.14 All other cause-specific mortality rates were significantly higher compared to those in the general population, with multiples fairly consistent with US data (DeVivo MJ, personal communication, 07 January 2017).
Compared with the original study by Frankel et al. 1998 (ref. 1) and other mortality studies, similar leading causes of death were found.6, 7, 8, 15, 16, 17, 18 In our study, and in all the cited studies, respiratory diseases were the leading cause of death after SCI, most strongly associated with the higher level of injury, and not showing improvement over time. However, compared to other studies, respiratory causes represented a higher proportion of deaths in our study, as did urogenital causes, whereas at the same time septicaemia and other infectious diseases were much rarer.6, 7, 8 A likely explanation is that in our study, the underlying cause of death was septicaemia of unclear origin only if there was no obvious source of septicaemia, as explained in the Methods section. Had all cases with sepsis listed under multiple causes of death been grouped together, there would have been 9.3% cases of sepsis in our study, which is close to the USA report of 10%.7 However, looking at all the infections listed as the leading cause of death, mainly respiratory, but also urinary and skin, with or without sepsis mentioned in death certificates, infections accounted for over a third of all deaths in all study periods (Table 1). Although most other causes of death showed an improvement over time, this did not change much during the study observation period. Cause-specific mortality rates showed a lack of improvement for respiratory causes throughout the study, most of which were infections, and a rise in rates in the latest study decade for urogenital causes, most of which were urinary infections, and for skin-related causes, namely infected pressure sores. Similar trends were reported in a recent American publication.19 This finding could, at least partly, explain the slowing down of life-expectancy improvement seen since the 1980s, and reported in our associated long-term survival paper.5 This also identifies the areas of care where further improvements in SCI care are possible, but in order to fully understand the problem, more detailed research is needed into underlying reasons. They could include, but are not limited to, in-hospital and community treatment of infections, antibiotic use and resistance, but also a potential discrepancy between increasing demands on specialist services because of the rising prevalence of SCI and available specialised SCI care provisions.
External causes, particularly violence and suicides, were less frequent in our study, especially in the later decades. It is not always possible to compare UK suicide statistics with those of other countries because many countries, including Canada, United States and France, use a narrower suicide definition. In spite of using the broader definition, which includes both suicide and self-harm of undetermined intent, the UK suicide figures were still lower, both for the general population and for the persons with SCI.15, 16, 17, 20, 21
Limitations
Only 22.9% of the deceased in our sample had a post-mortem report, so for most cases we had to rely on the accuracy of death certificates, sometimes supplemented by the information in medical notes for those who died in one of the two spinal centres.
Trends could have been affected by changes in reporting practices on death certificates over the long study period, including changes in thoroughness of reporting multiple causes.
Although the cause-specific mortality rates were adjusted for age differences over time, other differences in factors such as gender and injury severity could bias the trend in death rates. Given the increase in proportion of patients with tetraplegia over time, particularly high tetraplegia, there would be proportionately more person-years of high tetraplegia in the latest time period, and the trend of reduction in rates would be underestimated (more progress achieved than apparent).
A small percentage (1.2%) of deaths in our study was due to ill-defined causes. A further 6.5% of deaths had death certificates missing (mainly deaths before 1990) and those cases were excluded from the frequency analyses. Finally, 3.7% of the sample was lost to follow-up.
Strengths
The sample size and the length of the observation period allowed meaningful analysis of trends.
As suggested in the associated life-expectancy paper,5 the results of this study could be generalised for the whole country, as the study sample can be considered representative of the British SCI population.
Conclusions
Leading causes of death in persons surviving the first year post tSCI were respiratory, circulatory, neoplasms and urogenital. The proportion of individual causes differed during the study observation period and varied with the severity and duration of injury and age at death. In the early study decades urinary causes ranked first, but only fourth in the latest decades, whereas respiratory causes moved from the third to the first place. Respiratory diseases were the leading cause of death in persons with tetraplegia and in all age groups over the age of 30, and circulatory disease in persons with paraplegia and functionally incomplete SCI. Cause-specific mortality rates after SCI showed reduction over time for most leading causes, but, compared with the latest general population rates, were still higher for all leading causes, and especially for skin, urinary and respiratory diseases.
Data archiving
There were no data to deposit.
References
Frankel HL, Coll JR, Charlifue SW, Whiteneck GG, Gardner BG, Jamous MA et al. Long-term survival in spinal cord injury: a fifty year investigation. Spinal Cord 1998; 36: 266–274.
Geisler WO, Jousse AT, Wynne-Jones M, Breithaupt D . Survival in traumatic spinal cord injury. Paraplegia 1983; 21: 364–373.
Whiteneck GG, Charlifue SW, Frankel HL, Fraser MH, Gardner BP, Gerhart KA et al. Mortality, morbidity, and psychosocial outcomes of persons spinal cord injured more than 20 years. Paraplegia 1992; 30: 617–630.
DeVivo MJ, Stover SL . Long-term survival and causes of death. In: Stover SL, DeLisa JA, Whiteneck GG (eds) Spinal Cord Injury: Clinical Outcomes from the Model Systems. Aspen Publishers: Gaithersburg, MD. 1995, pp 289–316.
Savic G, DeVivo MJ, Frankel HL, Jamous MA, Soni B, Charlifue S . Long-term survival after traumatic spinal cord injury – a 70 year British study. Spinal Cord, (e-pub ahead of print 14 March 2017; doi:10.1038/sc.2017.23).
Hartkopp A, Bronnum-Hansen H, Seidenschnur AM, Biering-Sorensen F . Survival and causes of death after traumatic spinal cord injury. A long-term epidemiological survey from Denmark. Spinal Cord 1997; 35: 76–85.
DeVivo MJ, Krause JS, Lammertse DP . Recent trends in mortality and causes of death among persons with spinal cord injury. Arch Phys Med Rehabil 1999; 80: 1411–1419.
Middleton JW, Dayton A, Walsh J, Rutkowski SB, Leong G, Duong S . Life expectancy after spinal cord injury: a 50-year study. Spinal Cord 2012; 50: 803–811.
Soden RJ, Walsh J, Middleton JW, Craven ML, Rutkowski SB, Yeo JD . Causes of death after spinal cord injury. Spinal Cord 2000; 38: 604–610.
American Spinal Injury Association International Standards for Neurological Classification of Spinal Cord Injury, revised 2011, updated 2015. American Spinal Injury Association: Atlanta, GA, USA, 2015.
Frankel HL, Hancock DO, Hyslop G, Melzak J, Michaelis LS, Ungar GH et al. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. Paraplegia 1969; 7: 179–192.
World Health Organisation (WHO) The International Classification of Diseases version 10 (ICD-10) 2nd edn. WHO: Geneva, Switzerland. 2004.
World Health Organisation (WHO). Health Topics. Mortality. WHO 2016. Available at: http://www.who.int/topics/mortality/en/ (accessed on 28 December 2016).
Nahm LS, Chen Y, DeVivo MJ, Lloyd LK . Bladder cancer mortality after spinal cord injury over 4 decades. J Urol 2015; 193: 1923–1928.
Lidal IB, Snekkevik H, Aamodt G, Hjeltnes N, Biering-Sørensen F, Stanghelle JK . Mortality after spinal cord injury in Norway. J Rehabil Med 2007; 39: 145–151.
Hagen EM, Lie SA, Rekand T, Gilhus NE, Gronning M . Mortality after traumatic spinal cord injury: 50 years of follow-up. J Neurol Neurosurg Psychiatry 2010; 81: 368–373.
Ahoniemi E, Pohjolainen T, Kautiainen H . Survival after spinal cord injury in Finland. J Rehabil Med 2011; 43: 481–485.
Krause JS, Cao Y, DeVivo MJ, DiPiro ND . Risk and protective factors for cause-specific mortality after spinal cord injury. Arch Phys Med Rehabil 2016; 97: 1669–1678.
DeVivo MJ, Chen Y, Krause JS, Saunders LL . Trends in age-adjusted cause-specific mortality rates after spinal cord injury [abstract]. Top Spinal Cord Inj Rehabil 2012; 18: 214.
Cao Y, Massaro JF, Krause JS, Chen Y, DeVivo MJ . Suicide mortality after spinal cord injury in the United States: injury cohorts analysis. Arch Phys Med Rehabil 2014; 95: 230–235.
Kennedy P, Garmon-Jones L . Self-harm and suicide before and after spinal cord injury: a systematic review. Spinal Cord 2017; 55: 2–7.
Acknowledgements
The study was financially supported by the Buckinghamshire Healthcare NHS Trust Charitable Spinal Fund and the Ann Masson Legacy for Spinal Research Fund, UK. The original study (1) was supported in part by the National Institute on Disability and Rehabilitation Research grant #H133.G90010, USA. We thank the Medical Records staff at Stoke Mandeville and Southport Spinal Centres, and especially Mrs Pauline Bateman, for their help with medical notes retrieval.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on the Spinal Cord website
Supplementary information
Rights and permissions
About this article
Cite this article
Savic, G., DeVivo, M., Frankel, H. et al. Causes of death after traumatic spinal cord injury—a 70-year British study. Spinal Cord 55, 891–897 (2017). https://doi.org/10.1038/sc.2017.64
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2017.64
This article is cited by
-
Pulmonary function and sarcopenia as predictors of dysphagia in cervical spinal cord injury
Spinal Cord (2024)
-
Cardiac risk stratification and adverse outcomes in surgically managed patients with isolated traumatic spine injuries
European Journal of Trauma and Emergency Surgery (2024)
-
Correlates of metabolic syndrome in people with chronic spinal cord injury
Journal of Endocrinological Investigation (2024)
-
Impact of Neurogenic Lower Urinary Tract Dysfunction on Bowel Symptoms
Current Bladder Dysfunction Reports (2023)
-
Stem Cell Therapy in Spinal Cord Injury-Induced Neurogenic Lower Urinary Tract Dysfunction
Stem Cell Reviews and Reports (2023)