Abstract
Study design:
A prospective and a case-matched control study.
Objectives:
To study the lower urinary tract dysfunction associated with bladder lithiasis in patients with spinal cord injury (SCI).
Setting:
Toledo (Spain).
Methods:
We have carried out a urodynamic study in 30 patients with SCI with lithiasis in their bladder before and 3 months after bladder endoscopic lithotripsy. This second study was compared with the urodynamic findings of a different group of 30 patients with SCI, without a history of bladder lithiasis, paired with cases by gender and date of urodynamic study.
Results:
We have found that the prevalence of neurogenic detrusor overactivity (NDO) was significantly different after bladder lithotripsy, although the cystomanometric capacity was significantly increased. A group of patients with lithiasis showed a maximum flow rate, a voiding maximum detrusor pressure and the detrusor contractility parameter Wmax lower than that in controls. On the other hand, a voiding abdominal straining was found to be significantly greater than that in controls.
Conclusions:
Bladder lithiasis affects the presence of NDO in patients with SCI. Patients with SCI who develop bladder lithiasis present a lower detrusor contractility power compared with those who do not.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) is a chronic illness that often alters urinary tract innervation and is responsible for associated neurogenic dysfunction (neurogenic lower urinary tract dysfunction (NLUTD)).
Preventive measures are essential in these cases to avoid urological complications, including bladder lithiasis. Fortunately, the prevalence of bladder lithiasis has gradually fallen in the past decades. Thus Chen et al.1 report a 29% rate of bladder calculi between 1973 and 1979 versus 8% between 1990 and 1995. This decrease has been attributed to a better understanding of their physiopathology and the application of preventive measures in clinical practice, including improved bladder drainage technique and materials, early mobilisation and better treatment of urinary tract infections (UTI).2
The diagnosis and typification of NLUTD associated with SCI is the key to prevent kidney function impairment,3 and urodynamic study is the gold standard;4 but we are aware that only a high-quality study can establish, objectively, the presence of a dysfunction and to understand its clinical implications.5 However, certain urological complications, such as UTI, can affect the outcome of such studies.6 Consequently, it can be thought that bladder lithiasis as foreign bodies irritate the bladder. However, as far as we are concerned, this hypothesis has not been checked, and it remains unknown whether bladder lithiasis affects the reliability of the urodynamic results in spinal cord-injured patients.
Our hypothesis is that bladder lithiasis also modifies the results of urodynamic study in patients with SCI. Therefore, our aim is to examine urodynamic data associated with the presence of calculi in the bladder and to compare these data with those obtained from a second urodynamic study without them. Our secondary aim is to investigate whether patients with SCI and bladder stones display urodynamic data that differ from those of patients without this complication.
Methods
A prospective study was performed in a cohort of patients with SCI and bladder lithiasis who underwent urodynamic study with the bladder lithiasis present before and 3 months after endoscopic lithotripsy. We defined bladder lithiasis as the presence of at least one bladder calculi in the bladder, diagnosed by X-ray or ultrasound and confirmed by cystoscopy.
The sample size was calculated according to Chou et al.7 Considering a mean difference in maximum detrusor pressure during voiding of 1 cm H2O and s.d. in patients with SCIs of 10 cm H2O and assuming an alpha error of 5% and statistical power of 80%, the necessary sample size was 35 patients. The inclusion criteria were stable SCI, presence of bladder lithiasis and age >18 years. Exclusion criteria were active UTI, a lower urinary tract disease other than NLUTD and a history of prior bladder interventions. The hospital’s ethics committee approved the study, and all participants signed an informed consent form.
Of the 40 patients who underwent surgery for bladder stones between May 2012 and December 2014, 35 were included in the study. Of these, 30 completed the protocol. The mean age of the participants who completed the study was 37 years (s.d.: 14.7 years). Distribution by gender was 4 females and 26 males, and the time since SCI was 76 months (s.d.: 108.5 months), median: 21 months (range: 4–443 months) and the mean age at injury was 32 years (s.d.: 14.2 years, median: 30 years, range:18–71 years).
Distribution based on the level and grade of SCI is shown in Table 1. Twenty-two subjects performed clean intermittent bladder catheterisation, nine had indwelling urinary catheters and one patient voided by reflex micturition into external condom drainage. Patients received anticholinergic treatment in 20 cases, while the remaining 10 received no urological treatment whatsoever. Drug treatment and mode of bladder emptying were maintained until the second urodynamic study was conducted (post-lithotripsy).
A case-matched control was carried out study in order to determine whether the urodynamic data detected in patients with bladder calculi differ from those of participants without lithiasis. Controls were randomly selected among patients with SCI, without bladder lithiasis and matched with cases by gender and date of second urodynamic study (post-lithotripsy). The mean age of control group was 41 years (s.d.: 15.0 years), and the time from SCI was 19 months (s.d.: 57.2 months). The urodynamic data from controls were compared with the data of the second urodynamic study (post-lithotripsy) from the cases.
Urodynamic studies were performed using an MMS Solar polygraph (MMS, Enshede, The Netherlands) following the International Continence Society specifications,8 except where specifically noted. Urodynamic transducers were calibrated at atmospheric pressure before beginning the test, according to the recommendations of Schafer et al.5 Patients were placed in a supine position. The bladder was filled using a double lumen catheter inserted through the urethra with room-temperature saline solution at the rate of 20 ml s−1. The abdominal pressure was recorded using a rectal balloon catheter. The filling phase ended when there was an involuntary detrusor contraction (neurogenic detrusor overactivity (NDO)), urinary incontinence was recorded and the patient-referred discomfort or signs of autonomic dysreflexia were observed. Stress urinary incontinence was defined as the involuntary leakage of urine during increased abdominal pressure, in the absence of a detrusor contraction. The URA parameter was used to measure urethral resistance, and detrusor contractility was quantified with the Wmax and W8020 parameters. These parameters were automatically calculated by the computer software and subsequently revised manually by the urologist to rule out artefacts.
Lithotripsy was performed endoscopically in all cases using a Calcutrip 27080 Electrohydraulic Lithotriptor (Karl Storz GmbH & Co. KG, Tuttlingen, Germany). Prior to discharge, the absence of lithiasis was verified on X-ray and ultrasound.
The study data were stored in an Access (Microsoft inc., Redmond, WA, USA) database and later exported to SPSS version 12 software (SPSS Inc., Chicago, IL, USA) for statistical analysis. The statistical tests applied were Kolmogorov–Smirnov conformity test, Fisher’ exact test for dichotomous variables and the Student’s t-test for the comparison of means of paired and independent groups. Statistical significance was established at the two-sided 95% level.
Results
The mean weight of the extracted bladder lithiasis was 1.208 mg (s.d.: 3.249 mg). The differences regarding mean age between cases and control were not statistically significant. Nevertheless, the time of SCI evolution was statistically longer in the group of cases (P=0.015).
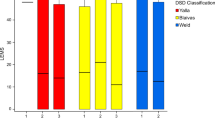
Table 2 illustrates urodynamic results before and after lithotripsy. Statistically significant differences are seen with respect to the presence of involuntary contractions and cystometric capacity (less on the urodynamic study with lithiasis).
Table 3 shows the comparison of urodynamic data between cases and controls. Statistically significant differences are observed between both groups in terms of maximum voiding flow (less in the lithiasis group), maximum detrusor voiding pressure (lower with lithiasis), maximum abdominal pressure during urination (higher in the group with bladder stones) and the Wmax bladder contractility parameter (lower in the group with bladder calculi).
Discussion
The results of this study confirmed our hypothesis that the presence of bladder lithiasis in patients with SCI significantly alters urodynamic data, albeit only during the filling phase. NDO was different in patients with calculi in the bladder than without them. DO appears in four patients before lithotripsy but disappears in one. Besides, their bladder capacity was less with calculi in the bladder.
Unlike the data observed in our study, studies conducted in non-neurogenic patients detected no significant differences in DO before and after litotripsy.9 Nevertheless, this outcome contrasts with the variability of the cystometric data and rate of DO noted on sequential urodynamic studies in non-neurogenic patients as compared with SCI patients whose cystometric variables and prevalence of DO do not vary when urodynamic studies are repeated.10 Moreover, in contrast to observations in non-neurogenic patients, the bladder-filling rate does not appear to influence the rate of NDO, as verified when the results obtained from the ambulatory urodynamic results are compared with those from the conventional study.11
In the event that the SCI lies above the parasympathetic micturition nucleus (S2–S4), voluntary control of urination is lost, as well as the spino-bulbar micturition reflexes. Consequently, after shock medullar phase, voiding becomes a spinal reflex. In addition, there is a change in afferent pathways of the sacral reflex arc, which goes from being controlled by myelinated type A delta fibres (that convey the feeling of bladder filling) to being under the control of unmyelinated type C fibres (that transmit nociceptive stimuli), and that are responsible for NDO in individuals with SCI.12 This change in neurological pathways seen in neurogenic patients implies that the stimuli that trigger urination are also different from the non-neurogenic ones. As a result, patients with NLUTD would be more sensitive to the stimuli arising from the irritation caused by the bladder stones, unlike non-neurogenic patients who would be more sensitive to the stimuli produced by bladder distension.
The cause of these urodynamic differences can be due to multiple mechanisms of action, such as the volume effect of bladder lithiasis. However, this effect is improbable because the mean volume of stone was 0.7 ml (1.208 mg divided by 1.7, which is the specific gravity for struvite). Other explanations could be the chemical effect of urine pH (which tends to be alkaline in the infective stones) or biological effects such as those of urinary infections. In light of the urodynamic differences observed with or without bladder lithiasis, this outcome must be taken into account when monitoring these patients.
Insofar as the urodynamic differences noted in the case-matched control study between SCI patients who developed bladder lithiasis versus those who did not, it must highlighted that in contrast to the previous study, the differences were observed in the voiding phase. Following lithotripsy, the participants who had developed bladder lithiasis exhibited a significantly lower maximum voiding flow, maximum voiding detrusor pressure and Wmax than the group-matched control, whereas their maximum abdominal pressure during micturition was significantly higher.
Bladder stones have typically been ascribed to an altered voiding phase resulting from bladder outlet obstruction.13 This is a theoretical hypothesis that has not been contrasted empirically, as it is not corroborated by data provided by urodynamic studies. In the cases in which this study is performed, no significant differences have been revealed as regards the degree of obstruction in patients with and without bladder stones.14 Our results are also a fly in the face of this hypothesis in patients with SCI, given that the urethral resistance parameter URA did not show significant differences between those patients who developed lithiasis and the matched control group. Another factor, such as postvoid residual urine, which would theoretically be greater in patients with bladder lithiasis,9, 14 also failed to display significant differences.
Some authors believe that, in the case of SCI, the main risk factor for bladder lithiasis is the presence of urinary catheters,1 whereas the functional changes of the urinary tract associated with lithiasis in these patients have scantly been studied. Only Donnellan and Bolton15 report NDO associated with elevated voiding pressure in these patients when they performed a urodynamic study in a group of patients with SCI and bladder stones. However, because a comparative study with a control group was not carried out, it cannot be confirmed that these data are related to bladder lithiasis.
The fundamental datum seen in our study is lower detrusor contractility in patients with bladder stones versus those without them. Other authors such as Millan-Rodriguez et al.9 also consider that detrusor underactivity is the main lower urinary tract dysfunction in non-neurogenic patients with bladder lithiasis. The longer time since SCI of the patients with lithiasis in our study might be the cause for this dysfunction.
Another datum of note derived from our study is the relationship between abdominal straining during voiding and bladder lithiasis. Salinas et al.16 verified a relationship between increased voiding abdominal straining and recurrent UTI in women. It is possible that the same mechanism might intervene in the formation of bladder calculi in patients with SCI by fostering UTI.
There are two main types of limitations to our study. First, given that it is a case-matched control study, and, as such, retrospective, we cannot be sure that there is a case–effect relationship between the functional changes of the lower urinary tract found and the presence of lithiasis. To confirm this relationship, we should carry out a prospective cohort study. Nevertheless, the low incidence of bladder lithiasis in our setting (approximately 1%) hinders this kind of study. The second limitation has to do with the sample size, as the number of patients who completed the protocol was less that the sample size initially planned. This may have masked the existence of other significant differences. However, our study did confirm the differences regarding voiding detrusor pressure, as they were greater than those expected.
Conclusions
Bladder calculi in SCI patients are associated with specific urodynamic data. During the filling phase, these calculi affect the presence of NDO, whereas during the voiding phase, patients who developed bladder lithiasis exhibited significantly less detrusor contractility than those who did not develop them.
Data archiving
There were no data to deposit.
References
Chen Y, DeVivo MJ, Lloyd LK . Bladder stone incidence in persons with spinal cord injury: determinants and trends, 1973-1996. Urology 2001; 58: 665–670.
Bartle P, Krebs J, Wöllner J, Göcking K, Pannek J . Bladder stones in patients with spinal cord injury: a long-term study. Spinal Cord 2014; 52: 295–297.
Gerridzen RG, Thijssen AM, Dehoux E . Risk factors for upper tract deterioration in chronic spinal cord injury patients. J Urol 1992; 147: 416–418.
Nosseir M, Hinkel A, Pannek J . Clinical usefulness of urodynamic assessment for maintenance of bladder function in patients with spinal cord injury. Neurourol Urodyn 2007; 26: 228–233.
Schäfer W, Abrams P, Liao L, Mattiasson A, Pesce F, Spangberg A et al. Good urodynamic practices: uroflowmetry, filling cystometry, and pressure-flow studies. Neurourol Urodyn 2002; 21: 261–274.
Arya LA, Northington GM, Asfaw T, Harvie H, Malykhina A . Evidence of bladder oversensitivity in the absence of an infection in premenopausal women with a history of recurrent urinary tract infections. BJU Int 110: 247–251.
Chou FH, Ho CH, Chir MB, Linsenmeyer TA . Normal ranges of variability for urodynamic studies of neurogenic bladders in spinal cord injury. J Spinal Cord Med 2006; 29: 26–31.
Abrams P, Cardozo L, Fall M, Griffiths D., Rosier P, Ulmsten U et al. The standardisation of terminology in coger urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology 2003; 61: 37–49.
Millán-Rodríguez F, Errando-Smet C, Rousaud-Barón F, Izquierdo-Latorre F, Rousaud-Barón A, Villavicencio-Mavrich H . Urodynamic findings before and after noninvasive management of bladder calculi. BJU Int 2004; 93: 1267–1270.
Ockrim J, Laniado ME, Khoubehi B, Renzetti R, Finazzi Agrò E, Carter SS et al. Variability of detrusor overactivity on repeated filling cystometry in men with urge symptoms: comparison with spinal cord injury patients. BJU Int 2005; 95: 587–590.
Vírseda-Chamorro M, Salinas-Casado J, de la Marta-García M, Esteban-Fuertes M, Méndez S . Comparison of ambulatory versus video urodynamics in patients with spinal cord injury. Spinal Cord 2014; 52: 551–555.
Yoshimura N, de Groat WC . Neural control of the lower urinary tract. Int J Urol 1997; 4: 111–125.
Schwartz BF, Stoller ML . The vesical calculus. Urol Clin North Am 2000; 27: 333–346.
Kim JW, Oh MM, Park HS, Cheon J, Lee JG, Kim JJ et al. Intravesical prostatic protrusion is a risk factor for bladder stone in patients with benign prostatic hyperplasia. Urology 2014; 84: 1026–1029.
Donnellan SM, Bolton DM . The impact of contemporary bladder management techniques on struvite calculi associated with spinal cord injury. BJU Int 1999; 84: 280–285.
Salinas J, Virseda M, Méndez S, Menéndez P, Esteban M, Moreno J . Abdominal strength in voiding cystometry: a risk factor for recurrent urinary tract infections in women. Int Urogynecol J 2015; 26: 1861–1865.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Vírseda-Chamorro, M., Salinas-Casado, J., Barroso-Manso, Á. et al. Influence of bladder lithiasis on lower urinary tract dynamics in patients with spinal cord injury. Spinal Cord 55, 765–768 (2017). https://doi.org/10.1038/sc.2017.46
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2017.46