Abstract
Study Design:
A prospective study.
Objectives:
Analysis of epidemiological data about acute spinal cord injury (SCI) in the Czech Republic over a period of 10 years (2006–2015).
Methods:
A data collection system was implemented in the rehabilitation centres which provides care to patients with acute SCI in the Czech Republic. The recorded variables are as follows: age at time of SCI; gender; cause of injury; neurological level of injury (NLI); and its severity (ASIA Impairment Scale (AIS)). Data from 2006 to 2015 were analysed and trends were determined.
Results:
The overall number of acute SCI ranges between 250 and 300 cases annually. Two-third of the affected population are males. The average age at time of SCI is 49.1 years. The average incidence of traumatic SCI is 15.5 cases per year and is gradually decreasing. The leading cause of SCI are falls (44.5%), followed by traffic accidents (28.2%) and sports injuries including diving into water (19.7%). The incidence of non-traumatic SCI is 8.6 cases per year on average and has an upward trend. Inflammatory lesions account for 26.7% of cases, tumours account for 20.9%, and vascular related injuries make up 17.7%. The NLI occurs most often in the cervical segments (45.3%). The most frequently occurring lesions are motor incomplete: AIS D (33.3%).
Conclusion:
This study shows a stable occurrence of SCI in the Czech Republic, with cervical and motor incomplete cases being the leading ones. Epidemiological data are needed to improve the care of SCI patients and to promote an active life following it.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) is one of the most debilitating traumas, causing major and irreversible physical and psychological disability the patient and permanently affecting their lifestyle. As most SCI victims are of working age, SCI has not only a negative impact on the quality of life but also significant socio-economic consequences. They can only be mitigated by providing high-quality comprehensive multidisciplinary care in the first months after SCI, including intensive rehabilitation. The systems of care for SCI patients differ between countries, but the goals remain the same—to help the patient achieve the highest possible level of motor ability, posture control and locomotion, to attain maximum independence and activity in their daily lives. The epidemiological data would inform medical/political agencies so adequate resources are provided to meet those goals.
In the Czech Republic, the system of comprehensive care of patients with acute SCI has been set up since 2002 by the Methodical Measure of the Ministry of Health of the Czech Republic, which designated a network of specialized centres. Four spinal cord units were gradually established, which provide post-acute follow-up care to the patients. Each of these spinal cord units serves a defined intake area, with the whole Czech Republic being covered. The follow-up rehabilitation care is provided in spinal cord rehab units established in three rehabilitation centres. Every patient following SCI is first hospitalized in an acute care unit. After being stabilized for 1–2 weeks, the patient is then transferred to a regional spinal cord unit where he spends 2–3 months. This is followed by rehabilitation at the spinal cord rehab unit for a period of 3–5 months, after which the patient is discharged home.
With the specialized SCI centres put into operation, a need has arisen to monitor the incidence of SCI cases. Unfortunately, only incomplete data are available at the Institute of Health Information and Statistics of the Czech Republic. The likely reason is that there are inconsistencies in the use of diagnoses according to the International Classification of Diseases and Related Health Problems ICD-10 or that there are gaps in the data collection. Therefore, one of the tasks of the newly established Czech Spinal Cord Society was to set up a centralized system for epidemiological data collection from all the spinal cord centres, which should provide updated information on the exact number of patients newly presenting with neurological deficits after an acute SCI. This data are necessary for negotiations with health insurance companies about the reimbursement for medical equipment, with the Ministry of Health about preventive programs and also with the Ministry of Labour and Social Affairs about programs regarding of social integration, employment opportunities and planning a barrier-free environment.
The study objectives are to analyse the continuously collected epidemiological data and to establish the incidence of SCI and its trends with reference to age, gender, cause of injury and neurological level of injury (NLI) and its severity in the Czech Republic over 10 years.
Materials and methods
The data collection system was set to be as simple as possible in order to be operational on a long-term basis. Only the data from all the centres providing care to patients with SCI within the same period of time after SCI can give information regarding the actual number of these patients. The variables monitored were: age at time of SCI; gender; NLI; and severity in accordance with the International Standards for Neurological Classification of Spinal Cord Injury.1 In the first years of the monitoring, some centres only used the basic classification of the severity of SCI into complete and incomplete injuries. After participating in educational courses about the correct examination of patients with SCI presented on a regular basis since 2009 by the Spinal Cord Unit of the University Hospital Motol, sensory and motor incomplete SCI started to be classified using the ASIA Impairment Scale (AIS). NLI and AIS were rated at admission. Another differentiation criterion was the cause of injury, such that SCI cases were classified into either traumatic or non-traumatic. A traumatic case was defined as a SCI caused by external force at different levels with a persistent neurological deficit. Cauda equina injury was also included in the data set but not isolated injury of nerve roots. A non-traumatic case was defined as an acute spinal cord lesion caused by non-traumatic factors, such as infection, vascular events, neoplastic growths and other factors, such as vertebral column degenerative disorders, affecting the same neural structures as a traumatic SCI.
Data from individual centres are entered annually in the system and are presented on the web pages of the Czech Spinal Cord Society, where they are freely accessible. Although some data from the spinal cord units are missing, complete epidemiological outputs have been available from all three spinal cord rehab units for each year of the past decade. Since these rehabilitation centres provide rehabilitation care to all patients with acute SCI in the Czech Republic, the numbers of patients reported to the system every year can be considered exact. Patients who died of acute complications, those with no rehabilitation potential (for example due to a dire prognosis due to cancer) or those with minimal sensory or motor deficits (for example, those with a lower extremity motor score more than 45), were not admitted to the spinal cord rehab unit and they were not, therefore, included in the study population.
Results
The number of acute SCI cases has varied over the decade between 250 and 300 per year (Table 1). In the Czech Republic which has a 10.5 million population, the incidence of both traumatic and non-traumatic SCI combined together is 25.1 cases per one million. Separately, the incidence of traumatic SCI is ~16.5 cases and incidence of non-traumatic SCI is 8.6 cases per one million population on average. Of all cases, 73.7% occur in males and 26.3% in females, and the male-to-female ratio has not changed significantly over time. The average age of patients at time of SCI is 49.1 years, with a recently increasing tendency towards 50 years of age and over.
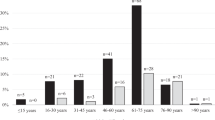
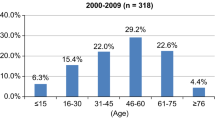
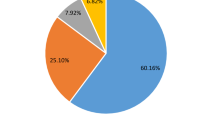
In the study period, a statistically significant trend can be seen which is a reduction in traumatic spinal cord injuries from ~200 to 150 per year and, at the same time, towards an increase in non-traumatic spinal cord injuries (P<0.05) (Figure 1). The leading cause of traumatic spinal cord injuries are falls (44.5% on average), followed by traffic accidents (28.2%). Over time, there is a statistically significant upward trend in SCI caused by falls and a significant downward trend in SCI due to traffic accidents (P<0.05). SCI caused by sports injuries and diving into water varies between 10 and 20 cases per year (9.8 and 9.9%, respectively; Figure 2). Non-traumatic SCI are caused by inflammation, more precisely spondylodiscitis or myelitis (26.7%), by tumours (20.9%) and by vascular lesions (17.7%). Other non-traumatic SCI (34.8%) are acute lesions associated with decompensation of degenerative spondylotic changes, disc herniation, spinal cord congenital defects or postoperative complications. Over time, there is a general upward trend in all non-traumatic lesions (Figure 3).
The neurological level of SCI is most often located in the cervical segments, in 45.3% of cases on average. Thoracic segments are affected in 39.9% of cases and lumbosacral segments in 14.8%. Over the decade, these proportions remain nearly unchanged. From the available data on the severity of SCI for the past 6 years, it is clear that the leading categories are motor incomplete SCI graded as AIS D (33.3%) and AIS C (30.6%), followed by sensorimotor complete SCI graded as AIS A (27.3%) and sensory incomplete SCI graded as AIS B (8.8%). Over the decade monitored, no clear trend in the distribution of cases by severity has been observed.
Discussion
Most epidemiological studies on the incidence of SCI focus on traumatic cases only. Lee et al.2 reviewed the literature concerning the epidemiological data in order to create a global map of the incidence of traumatic SCI. The global incidence of SCI in 2007 was estimated to be 23 cases per one million population, and in Western Europe to 16 cases per one million population. In our study cohort, the incidence of traumatic SCI alone is ~16.5 cases per one million on average. Most studies present data about short, 1–2-year periods of time.3, 4, 5, 6, 7, 8, 9, 10 Only some studies analyse the retrospective data for a longer period of time and thus can see particular trends in some variables.11, 12, 13, 14, 15, 16 Trends in the incidence of traumatic SCI in the European countries were studied for instance by McCaughey et al.13 who observed an upward trend over 20 years, from 13 to 17 cases per one million population. From our results, it follows that the incidence of traumatic SCI in the Czech Republic has been gradually decreasing to 14.7 cases per one million population in 2015. The literature data on the incidence of non-traumatic SCI was analysed by New et al.17 In Europe, based on the results of studies from eight countries, the incidence of non-traumatic SCI was six cases per one million population. On the basis of our data, the average incidence of non-traumatic SCI over the past decade was 8.6 cases per one million population and had an increasing trend.
The average age of patients with SCI varies across the world but tends to be higher in European countries where the trend continues. Van den Berg et al.18 report SCI to occur at the age of 43.2 years on average in Spain in 2001–2008, Ahoniemi et al.14 found SCI to affect males at 42.4 years of age on average and females at the age of 40.4 years on average in Finland in 1996–2005, while according to McCaughey et al.,13 the average age of patients with SCI was 50.7 years in Scotland in 2004–2008. In our study group, the average age at time of SCI was 49.1 years which is above the European average. However, it should be noted that both traumatic and non-traumatic cases of SCI are analysed together. Unfortunately, separate data for these two groups of patients are not available. Nevertheless, the summary data collected over the same period of time in the Spinal Cord Unit of the University Hospital Motol (which provides care to one fourth of patients with SCI) subsequently transferred to the rehabilitation centres suggest the average age to be 41.3 in those with traumatic SCI in comparison with 54.7 years in those with non-traumatic SCI. A higher average age at time of non-traumatic SCI has also been reported in Scotland (51.8 years)13 or in Italy (55 years).19
The leading cause of traumatic SCI in the Czech Republic are falls (44.5%), followed by traffic accidents (28.2%) and sports accidents including diving into water (19.7%). Similar results have been found in Sweden, Norway, Scotland, Finland or Estonia;6, 12, 13, 14, 20 but for instance, Greece, Turkey or Iran have reported traffic accidents as the leading cause of traumatic SCI (61.8%, 51% and 48.8%, respectively),6, 9, 21 and in the South Africa, 59.3% of SCI result from acts of violence.4 There is a surprising decrease in SCI due to motor vehicle accidents in the period of our study observation. Nevertheless, comparison of data about the total number of injuries from motor vehicle accidents confirms a general downward trend. In the past 3 years, there has been a significant reduction in the number of injuries due to diving accidents. This decrease is most likely related to education campaigns by various media which are publicized in the spring and summer months. These injury prevention programs warn about high-risk behaviour.
In our study cohort, a non-traumatic SCI is defined as an acute injury that occurs by a mechanism other than an external force, and that is why neurodegenerative diseases are not included. In descending order, the causes of non-traumatic SCI are inflammation (26.7%), tumours (20.9%) and vascular lesions (17.7%). Nevertheless, acute SCI caused by degenerative changes in the spine that would surely be among the leading causes are not considered separately in our study. In international literature concerning non-traumatic SCI, the results differ between studies. McCaughey et al.13 have reported vascular lesions to be the leading cause of SCI (40%), followed by infections (22.7%) and degenerative lesions (16.4%), with tumours being only the fourth leading cause of SCI (15.5%). On the other hand, Van den Berg et al.18 have reported tumours as the leading cause of SCI (34.8%), followed by mechanical (degenerative) lesions (17.6%) and vascular lesions (15.5%). However, unlike our study, their statistics also include lesions caused by multiple sclerosis which should be considered when comparing the data.
As for the neurological level of SCI in European countries, their leading locations are the cervical segments, followed by the thoracic and lumbar segments.5, 10, 12, 13 In Japan, as many as over two-third of SCI affect the cervical segments.3 On the other hand, for instance in Iran, the leading NLI was in the thoracic segments.21 In our study, the leading NLI are in the cervical segments (45.3%), followed by thoracic segments (39.9%). Multiple SCI severity approaches have been proposed. Some classify SCI into sensorimotor complete and incomplete (AIS A vs AIS B-D).12, 14, 22 Others divides SCI into motor complete and incomplete (AIS A,B vs AIS C,D),5, 23 whereas yet another grade SCI based on the original Frankel classification.3 ASIA Impairment Scale A-E is also used.13, 21, 24 One Tianjin, Chinese cohort has graded SCI cases reported results in descending order: AIS D, A, C, and B.24 A Scottish study reported similar results (AIS D, C, A, B).13 In comparison, an Iranian study reported sensorimotor complete SCI AIS A to be the leading category, followed by AIS B, C and D.21 Our findings were identical to the Scottish study in that SCI were classified, in descending order, as AIS D, C, A and B.
From our perspective, in the tertiary stage when the patients are discharged to home, the essential criterion is whether they manage the social bipedal locomotion or a wheelchair. This determines the requirements for adapting the home environment for the disabled, his/her social activities, employment opportunities and so on. Apart from patients graded AIS D, ~30% of patients with lumbar SCI are capable of bipedal locomotion. In our study cohort, these patients account for nearly 38%. One hundred and seventy persons on average join the population of wheelchair users in the Czech Republic every year.
Study limits
The data is not analysed separately for traumatic and non-traumatic SCI. It would be beneficial to compare these two groups for age, NLI and AIS. Moreover, it might also be of interest to provide the data on the age distribution of traumatic and non-traumatic SCI by cause of injury.
A certain percentage of patients cannot be transferred to the rehabilitation setting. This group includes patients who die of severe complications in the acute stage, those with high quadriplegia requiring long-term mechanical ventilation, non-compliant patients or those with significant comorbidities unable to cope with the rehabilitation process. In point of fact, the focus is on the number of patients who complete their rehabilitation in a rehabilitation setting and subsequently are discharged to home.
A source of more insightful data, for example about demographic characteristics, social status, complications and outcome over time, would be the National Registry which falls under the health care law. This still needs to be set up.
Conclusion
This study presented the results from 10 years of monitoring the epidemiological status of acute SCI in the Czech Republic. The incidence of traumatic SCI is 16.5 cases per one million population and that of non-traumatic SCI is 8.6 cases per one million population. Precisely opposite trends can be seen in the incidence of the two types of SCI over the 10-year period of time—the incidence of traumatic SCI is decreasing, while that of non-traumatic SCI is increasing. The age at SCI also has an upward trend. SCI causes and neurological characteristics do not vary significantly over time and are comparable with those in other European countries.
The centralized comprehensive systematic care for patients with SCI in the Czech Republic makes it possible to reduce complications in all stages of SCI and to provide intensive rehabilitation for the time necessary to reduce the neurological deficit and to achieve the fullest possible use of the patient's potential. The epidemiological research data help adjust not only the system of care to the patients' needs in the long-term and focus research strategies but also provide the information needed to underpin negotiations with policy makers in order to maximize the active life of the SCI population.
Data archiving
There were no data to deposit.
References
Kirshblum S, Waring W, Biering-Sorensen F, Burns SP, Johansen M, Schmidt-Read M et al. Reference for the 2011 revision of the International Standards for Neurological Classification of Spinal Cord Injury. J Spinal Cord Med 2011; 34: 547–554.
Lee BB, Cripps RA, Fitzharris M, Wing PC . The global map for traumatic spinal cord injury epidemiology: update 2011, global incidence rate. Spinal Cord 2014; 52: 110–116.
Katoh S, Enishi T, Sato N, Sairyo K . High incidence of acute traumatic spinal cord injury in a rural population in Japan in 2011 and 2012: an epidemiological study. Spinal Cord 2014; 52: 264–267.
Joseph C, Delcarme A, Vlok I, Wahman K, Phillips J, Nilsson Wikmar L . Incidence and aetiology of traumatic spinal cord injury in Cape Town, South Africa: a prospective, population-based study. Spinal Cord 2015; 53: 692–696.
Nijendijk JH, Post MW, van Asbeck FW . Epidemiology of traumatic spinal cord injuries in The Netherlands in 2010. Spinal Cord 2014; 52: 258–263.
Divanoglou A, Levi R . Incidence of traumatic spinal cord injury in Thessaloniki, Greece and Stockholm, Sweden: a prospective population-based study. Spinal Cord 2009; 47: 796–801.
Karamehmetoğlu SS, Nas K, Karacan I, Sarac AJ, Koyuncu H, Ataoğlu S et al. Traumatic spinal cord injuries in southeast Turkey: an epidemiological study. Spinal Cord 1997; 35: 531–533.
Hoque MF, Grangeon C, Reed K . Spinal cord lesions in Bangladesh: an epidemiological study 1994 - 1995. Spinal Cord 1999; 37: 858–861.
Karacan I, Koyuncu H, Pekel O, Sümbüloglu G, Kirnap M, Dursun H et al. Traumatic spinal cord injuries in Turkey: a nation-wide epidemiological study. Spinal Cord 2000; 38: 697–701.
van Asbeck FW, Post MW, Pangalila RF . An epidemiological description of spinal cord injuries in The Netherlands in 1994. Spinal Cord 2000; 38: 420–424.
Bjørnshave Noe B, Mikkelsen EM, Hansen RM, Thygesen M, Hagen EM . Incidence of traumatic spinal cord injury in Denmark, 1990-2012: a hospital-based study. Spinal Cord 2015; 53: 436–440.
Hagen EM, Eide GE, Rekand T, Gilhus NE, Gronning M . A 50-year follow-up of the incidence of traumatic spinal cord injuries in Western Norway. Spinal Cord 2010; 48: 313–318.
McCaughey EJ, Purcell M, McLean AN, Fraser MH, Bewick A, Borotkanics RJ et al. Changing demographics of spinal cord injury over a 20-year period: a longitudinal population-based study in Scotland. Spinal Cord 2016; 54: 270–276.
Ahoniemi E, Alaranta H, Hokkinen EM, Valtonen K, Kautiainen H . Incidence of traumatic spinal cord injuries in Finland over a 30-year period. Spinal Cord 2008; 46: 781–784.
Knútsdóttir S, Thórisdóttir H, Sigvaldason K, Jónsson H Jr, Björnsson A, Ingvarsson P . Epidemiology of traumatic spinal cord injuries in Iceland from 1975 to 2009. Spinal Cord 2012; 50: 123–126.
Aito S, Tucci L, Zidarich V, Werhagen L . Traumatic spinal cord injuries: evidence from 30 years in a single centre. Spinal Cord 2014; 52: 268–271.
New PW, Cripps RA, Bonne Lee B . Global maps of non-traumatic spinal cord injury epidemiology: towards a living data repository. Spinal Cord 2014; 52: 97–109.
van den Berg ME, Castellote JM, Mahillo-Fernandez I, de Pedro-Cuesta J . Incidence of nontraumatic spinal cord injury: a Spanish cohort study (1972–2008). Arch Phys Med Rehabil 2012; 93: 325–331.
Citterio A, Franceschini M, Spizzichino L, Reggio A, Rossi B, Stampacchia G . Gruppo Italiano Studio Epidemiologico Mielolesioni. Nontraumatic spinal cord injury: an Italian survey. Arch Phys Med Rehabil 2004; 85: 1483–1487.
Sabre L, Pedai G, Rekand T, Asser T, Linnamägi U, Kõrv J . High incidence of traumatic spinal cord injury in Estonia. Spinal Cord 2012; 50: 755–759.
Derakhshanrad N, Yekaninejad MS, Vosoughi F, Sadeghi Fazel F, Saberi H . Epidemiological study of traumatic spinal cord injuries: experience from a specialized spine center in Iran. Spinal Cord 2016; 54: 901–907.
Dahlberg A, Kotila M, Leppänen P, Kautiainen H, Alaranta H . Prevalence of spinal cord injury in Helsinki. Spinal Cord 2005; 43: 47–50.
Löfvenmark I, Norrbrink C, Nilsson-Wikmar L, Hultling C, Chakandinakira S, Hasselberg M . Traumatic spinal cord injury in Botswana: characteristics, aetiology and mortality. Spinal Cord 2015; 53: 150–154.
Zhou Y, Wang XB, Kan SL, Ning GZ, Li YL, Yang B et al. Traumatic spinal cord injury in Tianjin, China: a single-center report of 354 cases. Spinal Cord 2015; 54: 670–674.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kriz, J., Kulakovska, M., Davidova, H. et al. Incidence of acute spinal cord injury in the Czech Republic: a prospective epidemiological study 2006–2015. Spinal Cord 55, 870–874 (2017). https://doi.org/10.1038/sc.2017.20
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2017.20
This article is cited by
-
Long-term trends and risk factors of tracheostomy and decannulation in patients with cervical spinal cord Injury
Spinal Cord (2024)
-
A functional outcome prediction model of acute traumatic spinal cord injury based on extreme gradient boost
Journal of Orthopaedic Surgery and Research (2022)
-
Prospective epidemiological update on traumatic spinal cord injury in Ireland
Spinal Cord Series and Cases (2019)
-
Sepsis in mechanically ventilated patients with spinal cord injury: a retrospective analysis
Spinal Cord (2019)