Abstract
Study design:
Case–control study.
Objectives:
To investigate the level of autonomic nervous system dysfunction in patients with spinal cord injury and to determine its effect on the basal metabolic rate and oxygen consumption during daily living activities.
Setting:
Turkish Armed Forces Rehabilitation Center, Ankara, Turkey.
Methods:
Thirty-six patients with chronic spinal cord injury (SCI) were allocated into two groups according to the presence of autonomic nervous system dysfunction. Autonomic nervous system dysfunction was investigated with the measurements of blood pressure and heart rate during urodynamic examination and several provocative maneuvers (standing at tilt table, forcing deep respiration and Valsalva). Groups were compared in terms of the basal metabolic rate and oxygen consumption during daily living activities. Measurement of the basal metabolic rate was determined by indirect calorimetry under standardized conditions. Total body fat mass and lean tissue mass were measured in all participants using dual-energy X-ray absorptiometry by standard methods. Telemetric intrapulmonary gas exchange analyzer was used to measure oxygen consumption during daily living activities.
Results:
There was no statistically significant difference between the groups in age, time since injury, body mass lean and fat rates, or sensory and motor scores (P>0.05). Basal metabolic rates and oxygen consumption during daily living activities were not different between the groups (P>0.05).
Conclusions:
These results suggest that the presence of autonomic dysfunction does not change oxygen consumption at rest and during daily living activities.
Similar content being viewed by others
Introduction
Obesity is a common complication after spinal cord injury (SCI). Muscle paralysis and inactivity lead to alterations in body composition including a decrease in lean tissue mass and an increase in body fat.1 In parallel, the probability of adverse metabolic sequels such as glucose intolerance/insulin resistance, hyperlipidemia and cardiovascular diseases increases with lengthened life expectancy in patients with SCI.2, 3, 4, 5 Depressed total daily energy consumption causes an increase in risk of obesity.
Basal metabolic rate (BMR) is the amount of energy needed to sustain the involuntary activities of the body including maintaining muscle tone, body temperature and proper functioning of the heart, lungs and gastrointestinal tract. These involuntary activities are mostly regulated by the autonomic nervous system.6, 7 Thus, it might be thought that disorders of sympathetic control cause alterations in basal metabolic activity and oxygen consumption.8, 9, 10, 11, 12, 13 After SCI, autonomic nervous system dysfunction is a common complication mostly seen in patients with T6 or upper-level injuries. Monroe et al.14 showed that total energy consumption and the resting metabolic rate were lower in patients with SCI compared with that in able-bodied people and claimed that this difference might be due to reduced sympathetic nervous system activity, as well as a decrease in physical activity. However, they did not assess the level of autonomic nervous system activity in their study. Another study15 found that patients with T6 or upper-level injuries and autonomic dysfunction had lower BMR compared with patients with T7 or lower-level injuries. It was concluded that autonomic dysfunction might have an effect on BMR. The effect of autonomic nervous system dysfunction on oxygen consumption has not been studied.
The objectives of this study were to investigate the effect of autonomic nervous system dysfunction on task-related oxygen consumption during daily living activities and BMR patients with SCI and to determine daily energy need of patients with the different spinal injury level.
Materials and methods
Study design and participants
A case–control study design was undertaken. Thirty-six patients with SCI who were admitted to our rehabilitation center were considered for inclusion against the following inclusion criteria: (1) chronic SCI (minimum duration of 6 months post injury), (2) SCI of traumatic origin, (3) ASIA (American Spinal Injury Association) impairment scale of A or B, (4) inability to walk and (5) age of 18–55 years (young adult and middle-aged population). Patients were excluded if they had (1) lower motor neuron injury (cauda equina and conus medullaris syndrome), (2) thyroid dysfunction, (3) cardiopulmonary instability, (4) amputation (5) heterotopic ossification, (6) pressure ulcer, (7) infection, (8) concomitant head trauma and (5) history of chronic alcohol intake. All participants provided written informed consent. The study protocol was approved by the Local Ethics Committee.
Procedures and outcome measures
The patients were allocated into two groups. Group I includes the patients without autonomic nervous system dysfunction and Group II includes the patients with autonomic nervous system dysfunction. The diagnosis of autonomic nervous system dysfunction was based on mainly abnormalities in autonomic control of cardiovascular system. Therefore, autonomic dysfunction in the study actually referred to autonomic cardiovascular dysfunction. First of all, autonomic nervous system dysfunction was investigated with the measurements of blood pressure and heart rate during urodynamic examination. A blood pressure of >140/90 mm Hg and a heart rate of >100 beats per minute were regarded as autonomic dysreflexic response. In addition, each patient was assessed with several provocative maneuvers to detect autonomic dysfunction. Provocative tests were orthostatic hypotension while standing at the tilt table (a decrease in systolic blood pressure by at least 20 mm Hg or in diastolic blood pressure by at least 10 mm Hg within 3 min of orthostatic challenge was defined as criteria of orthostatic hypotension), ratio of maximum and minimum R–R distance at electrocardiogram with six forcing deep respiration in a minute (a ratio below 1.20 was abnormal) and the ratio of maximum and minimum heart rate during Valsalva maneuver (a ratio below 1.10 was abnormal).16, 17 An abnormal response to either urodynamics, orthostatic challenge or in the heart rate variability response to deep breathing or Valsalva was sufficient to classify them as having autonomic dysfunction. It means that if a patient had an abnormal response in one of the tests, he or she was considered as having autonomic dysfunction even if all other tests were normal. All provocative tests were listed in Table 1.
Demographic data including age, time elapsed since injury, etiology of injury, injury level and AIS (American Spinal Injury Association Impairment Scale) grading were recorded. Clinical parameters including total motor and sensory score obtained from the standardized AIS (American Spinal Injury Association Impairment Scale) clinical exam, the total functional independence measure score18 and the average Ashworth Scale19 score assessed on lower extremity muscles for spasticity were evaluated because of their possible effects on functionality and energy expenditure in SCI. Patients were also assessed with the following outcome measures: (1) BMR measured by indirect calorimetry, (2) body composition assessed using dual-energy X-ray absorptiometry and (3) oxygen consumption during daily living activities measured by telemetric intrapulmonary gas exchange analyzer.
Measurements of BMR were determined by indirect calorimetry under standardized conditions, using a nose clip and a respiratory valve with rubber mouthpiece held in place by a mechanical arm. The automatic gas analyzer (Sensormedics 29c; Sensormedics, Yorba Linda, CA, USA) was calibrated before each measurement and was also regularly calibrated for volume. All measurements were performed between 0800 and 0930 hours after an overnight fast (12–14 h), and room temperature was maintained at 22–24 °C. Each patient rested for 10 min before the start of the measurement and was given the opportunity to get acquainted with the new environment, mouthpiece and nose clip. During the measurement, the patient was supine on a bed. The gas analyzing system measured VO2 consumption continuously over a period of 45 min, and printouts were made at 1 min intervals, describing the mean values per minute. The first 15 min of each recording were discarded, as measured values have been shown to be significantly higher compared with a subsequent period of measurement20 and to ensure a steady state.21, 22
Lean and fatty tissue mass was measured in all participants using DXA by standard methods (model PDX-MD; Lunar Radiation, Madison, WI, USA). Whole-body scanning of the subjects, positioned prone on the scanner table, was performed with a congruent beam of stable dual-energy radiation at two different energies. The ratio of absorption between the two X-rays of different energies was linearly related to the free fat mass tissue compartment.13
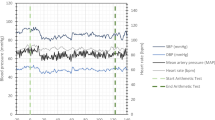
Telemetric intrapulmonary gas exchange analyzer (Oxycon Mobile, Jäger, Würzburg, Germany) was used to measure oxygen consumption during daily living activities. It is a lightweight (950 g) portable spirometric device. The device measures the oxygen concentration through an electrochemical sensor and data are transmitted telemetrically and recorded on a personal computer. During activities, the device was comfortably strapped to the chest or the back of the patients. Oxygen uptake (VO2)(ml min−1) and carbon dioxide output (VCO2) were measured with the breath-by-breath method. Before data collection, the system was calibrated using the calibration gas cylinder to ensure that all parameters were at baseline levels to avoid any misleading readings. Each patient practiced using the facemask of the device beforehand. After an adequate rest period with the facemask, the measurement was carried out during daily living activities including upper body dressing, lower body dressing, bed to chair transfer and toilet transfer. Those activities were chosen because they are also assessed in the functional independence measure. In addition, energy expenditure was measured during a single tour of wheelchair training track that is specially designed for wheelchair users. A single tour of this track included wheelchair activities of going uphill, going upstairs, going downstairs, passing over barriers with different heights and going on different grounds including sandy, gravelly and rocky. It took 20 min to perform all those activities consecutively. VO2 and VCO2 were determined during the final 15 min of the activities to ensure a steady state.
Statistical analysis
To achieve a minimal clinically important difference for VO2 (3.4±3.5 ml min−1) based on literature with regard to spinal cord injury, 18 patients per group were calculated using the 5% significance level and 80% power. Thirty-six patients with SCI were included in the study.
Data analysis was performed using SPSS for Windows, version 13.0 (SPSS Inc., Chicago, IL, USA). Data are presented as mean±s.d., unless otherwise indicated. An independent-sample t-test and χ2 test/Fisher’s exact test were used to compare patents’ baseline characteristics between the two study groups. An independent-sample t-test was used to compare outcome measures between the groups. A value of P<0.05 was considered statistically significant.
Results
Thirty-six male subjects with a mean age of 24.5±3.8 years in Group I and 27.7±8.1 years in Group II participated in the study. There were no significant differences in patients’ demographics and baseline data between the groups (P>0.05). Detailed demographic and clinical characteristics of the patients are presented in Table 2.
Comparison of oxygen consumption, carbon dioxide production, lean tissue mass, fatty tissue mass and BMR did not show a significant difference between Group I and Group II (P>0.05). Study outcome data are presented in Table 3.
Discussion
The study aimed to investigate the changes in energy metabolism to define the effects of autonomic dysfunction in SCI. The results showed that there was no difference between the patients with SCI who had autonomic dysfunction and those who had not in terms of task-related oxygen consumption during daily living activities and BMR.
The possible effects of autonomic dysfunction on energy metabolism in chronic SCI were first reported by Bucholz et al.23 No difference was found in paraplegics with the spinal injury level affecting cardiac sympathetic innervation in terms of energy expenditure. The limitations of that study were that functional capacity of the subjects was not measured and energy expenditure was measured with a formula using heart rate monitoring. The specific effect of autonomic dysfunction on energy metabolism was investigated in a study by Yılmaz et al.15 The difference in BMR was close to significant between patients with T6 or upper-level injuries and patients with T7 or lower-level injuries. In that study, the presence of autonomic dysfunction was predicted using injury level only, and there was no other objective assessment. Autonomic dysfunction occurs most often in patients with spinal lesions above the T6. However, it can occur rarely in patients with a lesion as low as T10.24 There were four patients with spinal lesions below T6 who had autonomic dysfunction in the present study. They all had complete neurological lesion with the spinal level of T8 and T9.25 In this study, the presence of autonomic dysfunction was determined after a detailed evaluation of the autonomic nervous system. With more reliable assignment of patient groups, it can be assumed that the data provided in this study are more reliable.
However, the findings of this study may be considered surprising because the current knowledge of physiology should have indicated that cardiovascular autonomic dysfunction would have an impact on energy metabolism. It could therefore be expected that the presence of autonomic dysfunction would have a role in oxygen consumption and BMR of patients with SCI. As a result of these findings, some hypotheses to account for this perplexity may be suggested. Some adaptive mechanisms elicited after SCI may lead to a compensatory regulation in energy metabolism against autonomic dysfunction. This adaptation might occur by means of humoral receptor mechanisms. This proposition may be studied in future laboratory research comparing patients with SCI in the acute stage and the chronic stage. The renin–angiotensin system might be one of those adaptive mechanisms. There is evidence that the role of the renin–angiotensin system in maintaining blood pressure is changed in patients with SCI.24 However, the data of blood pressure were lacking in the present study; hence, a comparison could not be implemented between the groups. It would be worth investigating whether the way the cardiovascular system responds during everyday activities differs between patients with or without autonomic dysfunction. A limitation of this study is that validation and reliability of the mobile telemetric intrapulmonary gas exchange analyzer is not known in patients with SCI. However, the measurement of oxygen consumption was performed with a portable device while performing daily living activities and using a wheelchair on a specially designed track. It seemed to be a rational method for measuring task-oriented energy expenditure in SCI. Real conditions were provided for patients with SCI rather than a laboratory setting. A similar method has been used in sports activities for wheelchair users.26 As another limitation, it should be noted that all the measurements of autonomic dysfunction used in the study might not be relevant when taking into consideration the adjustments of the cardiovascular system during everyday activities that might impact on oxygen consumption. For example, the presence of autonomic dysreflexia may not be as good a measure as the response to orthostatic challenge.
Conclusion
These results suggest that the presence of autonomic dysfunction after SCI does not make any changes in BMR and oxygen consumption during daily living activities. Future studies should focus on the effect of autonomic dysfunction on energy expenditure during exercise and other high-intensity activities in patients with SCI.
Data archiving
There were no data to deposit.
References
Kocina P . Body composition of spinal cord injured adults. Sports Med 1997; 23: 48–60.
Bauman WA, Adkins RH, Spungen AM, Waters RL . The effect of residual neurological deficit on oral glucose tolerance in persons with chronic spinal cord injury. Spinal Cord 1999; 37: 765–771.
Karlsson AK . Insulin resistance and sympathetic function in high spinal cord injury. Spinal Cord 1999; 37: 494–500.
Maki KC, Briones ER, Langbein WE, Inman-Felton A, Nemchausky B, Welch M et al. Associations between serum lipids and indicators of adiposity in men with spinal cord injury. Paraplegia 1995; 33: 102–109.
Krum H, Howes LG, Brown DJ, Ungar G, Moore P, McNeil JJ et al. Risk factors for cardiovascular disease in chronic spinal cord injury patients. Paraplegia 1992; 30: 381–388.
Berne MR, Levy NM (eds). Physiology 3rd edn. Mosby: New York, NY, USA. 1998.
Guyton CA, Hall EJ (eds). Medical Physiology 10th Turkish edn. Nobel Tıp Press: Istanbul, Turkey. 2001.
Jeon JY, Steadward RD, Wheeler GD, Bell G, McCargar L, Harber V . Intact sympathetic nervous system is required for leptin effects on resting metabolic rate in people with spinal cord injury. J Clin Endocrinol Metab 2003; 88: 402–407.
Saad MF, Alger SA, Zurlo F, Young JB, Bogardus C, Ravussin E . Ethnic differences in sympathetic nervous system-mediated energy expenditure. Am J Physiol 1991; 261: 789–794.
Toubro S, Sorensen TI, Ronn B, Christensen NJ, Astrup A . Twenty-four hour energy expenditure: the role of body composition, thyroid status, sympathetic activity, and family membership. J Clin Endocrinol Metab 1996; 81: 2670–2674.
Acheson KJ, Ravussin E, Schoeller DA, Christin L, Bourquin L, Baertschi P et al. Two-week stimulation or blockade of the sympathetic nervous system in man: influence on body weight, body composition, and twenty four-hour energy expenditure. Metabolism 1988; 37: 91–98.
Buemann B, Astrup A, Madsen J, Christensen NJ . A 24-h energy expenditure study on reduced-obese and nonobese women: effect of beta-blockade. Am J Clin Nutr 1992; 56: 662–670.
Bauman WA, Spungen AM, Wang J, Pierson RN . The relationship between energy expenditure and lean tissue in monozygotic twins discordant for spinal cord injury. J Rehabil Res Dev 2004; 41: 1–8.
Monroe MB, Tataranni PA, Pratley R, Manore MM, Skin-ner JS, Ravussin E . Lower daily energy expenditure as measured by a respiratory chamber in subjects with spinal cord injury compared with control subjects. Am J Clin Nutr 1998; 68: 1223–1227.
Yilmaz B, Yasar E, Goktepe S, Alaca R, Yazicioglu K, Dal U et al. Basal metabolic rate and autonomic nervous system dysfunction in men with spinal cord injury. Obesity 2007; 15: 2683–2687.
Ravits JM . AAEM minimonograph #48: autonomic nervous system testing. Muscle Nerve 1997; 20: 919–937.
Hilz MJ, Dütsch M . Quantitative studies of autonomic function. Muscle Nerve 2006; 33: 6–20.
Hall KM, Cohen ME, Wright J, Call M, Werner P . Characteristics of the functional independence measure in traumatic spinal cord injury. Arch Phys Med Rehabil 1999; 80: 1471–1476.
Craven BC, Morris AR . Modified Ashworth Scale reliability for measurement of lower extremity spasticity among patients with SCI. Spinal Cord 2010; 48: 207–213.
Isbell TR, Klesges RC, Meyers AW, Klesges LM . Measurement reliability and reactivity using repeated measurements of resting energy expenditure with a facemask, mouthpiece, and ventilated canopy. J Parenter Enteral Nutr 1991; 15: 165–168.
Warner JT, Bell W, Webb DK, Gregory JW . Daily energy expenditure and physical activity in survivors of childhood malignancy. Pediatr Res 1998; 43: 607–613.
Firouzbakhsh S, Mathis RK, Dorchester WL, Oseas RS, Groncy PK, Grant KE et al. Measured resting energy expenditure in children. J Pediatr Gastroenterol Nutr 1993; 16: 136–142.
Buchholz AC, McGillivray CF, Pencharz PB . Physical activity levels are low in free-living adults with chronic paraplegia. Obes Res 2003; 11: 563–570.
Popa C, Popa F, Grigorean VT, Onose G, Sandu AM, Popescu M et al. Vascular dysfunctions following spinal cord injury. J Med Life 2010; 3: 275–285.
Garstang SV, Miller-Smith SA . Autonomic nervous system dysfunction after spinal cord injury. Phys Med Rehabil Clin N Am 2007; 18: 275–296.
Abel T, Platen P, Rojas Vega S, Schneider S, Strüder HK . Energy expenditure in ball games for wheelchair users. Spinal Cord 2008; 46: 785–790.
Acknowledgements
The study was supported by the Scientific and Technological Research Council of Turkey (107S165).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Yilmaz, B., Göktepe, S., Yaşar, E. et al. The effect of autonomic nervous system dysfunction on oxygen consumption during daily living activities in patients with spinal cord injury. Spinal Cord 55, 300–303 (2017). https://doi.org/10.1038/sc.2016.111
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2016.111