Abstract
Study design:
This is a single-center retrospective study.
Objectives:
The objective of this study was to study the clinical symptoms and electrophysiological features of C6–7 myelopathy.
Setting:
This study was conducted at the Department of Orthopedic surgery, Yamaguchi University Graduate school of medicine, Japan.
Methods:
A total of 20 patients with cervical compressive myelopathy were determined by spinal cord-evoked potentials or a single level of obvious magnetic resonance imaging (MRI)-documented cervical spinal cord compression. Neurological examinations included manual muscle testing and investigation of deep tendon reflex, including Hoffmann sign, and of sensory disturbance areas. Motor-evoked potentials (MEPs), compound muscle action potentials (CMAPs) and F-wave were recorded from bilateral abductor digit minim and abductor halluces muscles. Central motor conduction time was calculated as follows: MEPs latency−(CMAPs latency+F latency−1)/2 (ms).
Results:
Eighteen patients (90%) had negative Hoffmann sign. Eight patients (40%) had no sensory disturbance in the upper limbs and 8 patients (40%) had no muscle weakness in the upper limbs. We determined that patients had cervical myelopathy when their central motor conduction time measured in abductor digit minim was longer than 6.76 ms (+2 s.d.). Using this definition, the sensitivity for myelopathy was 42.8%.
Conclusion:
Patients with C6–7 myelopathy may lack clinical symptoms in their hands and central motor conduction time measured in abductor digit minim tended to be less prolonged, and it only showed symptoms in their lower limbs as gait disturbance. Surgeons should bear in mind the possibility of disorders of caudal C6–7 when they encounter patients with no or few symptoms in their hands and with leg weakness or numbness.
Similar content being viewed by others
Introduction
The frequency of diagnosis for cervical compressive myelopathy has recently increased, reflecting an aging society. The initial clinical symptoms of cervical compressive myelopathy are general numbness and sensory disturbance in the upper limbs, reaching motor dysfunction with progression of the myelopathy. It is not difficult to diagnose cervical compressive myelopathy in typical cases by using appropriate physical and radiographic examinations. However, we have experienced a small number of patients with cervical compressive myelopathy who had only slight or no obvious clinical signs in the upper limbs. This absence of neurological signs in the upper limbs can lead to erroneous diagnosis of thoracic or lumbar spinal diseases.
However, C6–7 myelopathy is a relatively rare condition, and there have not been many studies to date. The clinical and electrophysiological findings associated with this condition therefore remain unclear. The diagnosis of C6–7 myelopathy can be difficult, depending on the distinctive neurological signs present. We have previously measured multimodal spinal cord-evoked potentials (SCEPs) to diagnose the responsible level of cervical compressive myelopathy. SCEPs are a useful and reliable way to investigate the functional integrity of the spinal cord when magnetic resonance imaging (MRI) shows evidence of compression at several levels.1, 2, 3 In the present study, we assessed the clinical symptoms and electrophysiological findings in patients with C6–7 myelopathy with the aim of elucidating the characteristic features of this condition.
Patients and methods
Patients
A total of 20 patients with cervical compressive myelopathy were determined by intraoperative SCEPs to have a single site of conduction abnormality at the intervertebral level, or a single level of obvious MRI-documented cervical spinal cord compression. These comprise 7 cases with cervical spondylotic myelopathy, 10 with cervical disc herniation and 3 with ossification of the longitudinal ligament of the cervical spine. Central motor conduction time had been measured in 15 patients before surgery, as described below. The average patient age was 58.6 (range 40–79) years. Patients underwent cervical laminoplasty and measurement of SCEPs when MRI showed multiple compressions. They underwent anterior decompression with spinal fusion when MRI showed a single-level compression.
Written informed consent with the approval of Yamaguchi University Graduate School of Medicine was obtained for the preoperative MRI investigations and electrophysiological studies in patients. Patients who fulfilled the criteria given below were included in the study.
A diagnosis of myelopathy was established on the basis of the presence of hyperreflexia, upper or lower extremity sensory disturbance and obvious MRI-documented cervical spinal cord compression. Sensory and motor nerve conduction velocities in peripheral nerves were within normal limits. Patients who had peripheral neuropathy, cephalopathy or thoracic compressive myelopathy were excluded.
Magnetic resonance imaging
All patients underwent MRI with a 1.5-T imaging system (Siemens Japan, Tokyo, Japan). Sections were 5-mm thick with a 2-mm gap between intersections. T1- and T2-weighted sagittal and axial images were obtained.
Neurological symptoms
We performed several neurological examinations including manual muscle testing, investigation of deep tendon reflexes including the Hoffmann sign and evaluation of areas of sensory disturbance by pin prick or light touch. Similar to previous reports, we made presumptions on the involved area of the spinal cord based on neurological signs.
We hypothesized that sensory disturbance in the little finger sometimes also includes the ring finger; involvement of C8 sensory segment, and in the middle and ring fingers; involvement of C7, according to dermatome by Brain and Watson.4 We hypothesized the myotomal distribution as follows: triceps in C6–8 cord segments (main myotome, C7), extensor digit communis in C7 and C8 cord segments (C8) and abductor digit minim in C8 and T1 cord segments (C8).
We hypothesized that localization of the reflex center of triceps would be at C7, and of the Hoffmann sign at C8. Diminished deep tendon reflex results from involvement of the lower motor neuron, and exaggerated deep tendon reflex results from involvement of the upper motor neuron. For example, normal or diminished triceps tendon reflex and positive Hoffmann sign indicate involvement of C5–6 level, and normal triceps tendon reflex and negative Hoffmann sign indicate caudal to C6–7 level. We assessed triceps tendon reflex, Hoffmann sign and patella tendon reflex.
Recording of central motor conduction time
All electrophysiological assessments were performed using a Nicolet Viking 4 instrument (Natus Medical Incorporated, San Carlos, CA, USA). Self-adhesive surface recording electrodes were placed on target muscles. Motor-evoked potentials (MEPs) were recorded from bilateral abductor digit minim and abductor halluces muscles. Transcranial magnetic stimulation was delivered using the Magstim 200 instrument (The Magstim Company, Carmarthenshire, UK) with a circular coil having an outer diameter of 140 mm. Transcranial magnetic stimulation was applied while the patient exerted isometric voluntary contraction of the target muscles. The coil was held with its center on the Cz position of the 10–20 system for recording MEPs from the abductor digit minim and moved frontally for recording MEPs from the abductor halluces. Transcranial magnetic stimulation intensity was set at 20% above the MEP threshold. At least 4 consecutive trials were recorded and superimposed. The shortest onset latency of the MEPs was recorded (MEP latency).
Compound muscle action potentials (CMAPs) and F waves were recorded following supramaximal electric stimulation of the ulnar nerve at the wrist and of tibial nerves at the ankle. Sixteen serial responses were obtained, and the shortest latency of F waves was measured. Peripheral motor conduction time was calculated as follows: (CMAPs latency+F latency−1)/2. Central motor conduction time was calculated as follows: MEPs latency−Peripheral motor conduction time (ms); Figure 1). The baseline-to-negative peak amplitudes of the m waves and MEPs were measured. All muscle responses were amplified and filtered with a band-pass of 5–5000 Hz.
MEP latency was recorded in the abductor digit minim (ADM) muscle or in the abductor halluces (AH) muscle by transcranial magnetic stimulation. The conduction time from the cerebral cortex to the motor segment was defined as central motor conduction time. This was derived by subtracting the peripheral motor conduction time from the MEP latency.
Control subjects
Thirty healthy subjects (average age, 42.6 years; age range, 23–73 years) with no history of injury or pathology to the upper limb were also evaluated as a control group. They underwent medical examination consisting of a detailed history regarding motor and sensory dysfunctions, followed by thorough physical examination. Exclusion criteria were a history of upper limb symptoms, glove and stocking sensory symptoms, diabetes mellitus, any form of medication, and abnormal tendon reflexes or sensory and motor examination.
Recording of SCEPs for the diagnosis of symptomatic lesions
SCEPs following transcranial electric stimulation (TES-SCEPs) and spinal cord stimulation (Spinal-SCEPs) were recorded intraoperatively in prone position when we performed cervical laminoplasty. TES was delivered as square pulses of 0.2 ms duration and at an intensity of 100 mA through needle electrodes (13R25, Dantec Dynamics, Skovlunde, Denmark) placed on the skull. The anode was placed 7 cm laterally to the right of the vertex on a line joining the external auditory meatus. The cathode was placed on the opposite side. Spinal-SCEPs were delivered by an epidural catheter electrode (UKG-100–2PM, Unique Medical corporation, Tokyo, Japan) inserted into the dorsal epidural space from the C7–T1 and T11–T12 interlaminar space. Square wave pulses (0.2 ms duration, 3 Hz rate) were delivered at an intensity of 15–20 mA. Before surgery, all SCEPs were recorded intraoperatively with recording electrodes (13R25, Dantec Dynamics) inserted in the ligamentum flavum at each interlaminar space. A reference electrode was inserted into the subcutaneous tissue in the posterior aspect of the neck for the recording of Spinal-SCEPs and TES-SCEPs. All SCEP signals were amplified and filtered with a band-pass of 20–3000 Hz using a standard evoked potential/electromyography machine (Nicolet Viking, Natus Medical Incorporated, San Carlos, CA, USA). An average of 40–60 TES-SCEPs and 40–50 spinal-SCEPs responses were obtained. Two different averaged responses were superimposed and displayed. For both TES-SCEPs and Spinal-SCEPs, intervertebral levels with a marked reduction in the size of the negative peak (>50%) were considered to be significant (Figure 2).2, 3
Statistical analysis
The upper limits for central motor conduction time were determined as the mean+2 s.d.). Mann–Whitney's U-test was used for comparison of test results between the patient and control groups. P-values <0.05 were regarded as statistically significant.
Results
All patients showed neurological recovery after cervical surgery.
Clinical findings
Detailed clinical findings are shown in Table 1.
Initial symptoms
Eleven patients (55%) showed initial symptoms in the upper limbs, whereas 9 patients (45%) had initial symptoms in the trunk or lower limbs manifesting as numbness or gait disturbance.
Sensory disturbance
Eight patients (40%) had no sensory disturbance in the upper limbs, 2 (10%) patients had disturbance in all fingers, 1 (5%) patient in the middle to little fingers and 8 (40%) patients in the little finger and/or ring finger (Figure 3).
Muscle weakness
Eight patients (40%) had no muscle weakness in the upper limbs. One patient (5%) had muscle weakness in the triceps brachii muscle, 7 (35%) patients in the extensor digit communis and 10 (50%) patients in the abductor digit minim (Table 2).
Deep tendon reflex and Hoffmann sign
Eleven patients (55%) had diminished or absent triceps tendon reflex and 18 (90%) had negative Hoffmann sign (Table 3). Fifteen patients (75%) showed exaggerated patella tendon reflex.
Central motor conduction time
The normal value (mean±s.d.) for central motor conduction time in abductor digit minim was 5.14±0.81 ms (range 3.85–6.82 ms), and in abductor halluces it was 11.41±1.32 ms (range 8.95–13.6 ms).
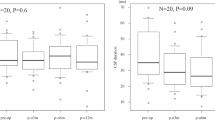
Central motor conduction time in abductor digit minim was measured in 15 patients, and in 14 of these the central motor conduction time was successfully recorded (Table 4). The mean value for central motor conduction time in abductor digit minim was 6.94±2.14 ms (range 4.2–11.5 ms), and it was significantly longer than normal values (P=0.001). We determined whether patients had cervical compressive myelopathy when central motor conduction time in abductor digit minim was longer than 6.76 ms (+2 s.d.). Using this definition, the sensitivity for myelopathy was 42.8%.
Central motor conduction time in abductor halluces was successfully recorded in 13 of 15 patients. The mean value for central motor conduction time in abductor halluces was 18.04±4.51 ms (range 13.2–27), and this was significantly longer than normal values (P<0.001). We determined that patients had cervical compressive myelopathy when central motor conduction time in abductor halluces was longer than 14.05 ms (+2 s.d.). Using this definition, the sensitivity for myelopathy was 92.3% (Figure 4).
Discussion
The major findings of this study are that most patients with C6–7 myelopathy had no or few neurological signs in the upper limbs, and that the sensitivity of central motor conduction time in abductor digit minim was less than that of central motor conduction time in abductor halluces.
Area of sensory disturbance
Several authors reported that the border between C8 and T1 sensory segments in the spinal cord is at the level of the C6–7 disc.6, 7 Compression of the spinal cord at the C6–7 disc level could lead to involvement of the C8 sensory segment or of the T1 sensory segment. Hence, most patients would show no or only localized sensory disturbance, mostly in the little fingers of their hands. Eight patients (40%) had sensory disturbance in their little finger that sometimes also included the ring finger; involvement of C8 sensory segment,4 but some patients had disturbance in the thumb to middle finger. Although the reasons for this are unclear, one possible explanation is concomitant C7 radiculopathy. C7 nerve roots would distribute the lesion mainly to the middle and ring fingers.4 Yoss5 reported that sensory disturbance in thumbs was affected by the C6 nerve root, in the index and middle fingers by the C7 root and in the ring and little fingers by the C8 root. However, the distributed lesion of a single nerve root overlaps the lesion of the adjacent nerve root. Yoss5 also reported that the distribution of sensory disturbance located only in the thumb indicated involvement of the C6 nerve root, whereas the distribution of sensory disturbance from the thumb to the middle or to all fingers indicated involvement of the C7 nerve root.
Distribution of muscle weakness
The patients in our study had muscle weakness, and half of them showed muscle weakness of abductor digit minim. We feel that abductor digit minim would be the key muscle for the diagnosis of C6–7 myelopathy. As the main myotome of abductor digit minim is C8, this resulted from involvement of the C8 motor segment.7, 8 However, because of individual variation with this myotome, patients whose T1 segment distributed abductor digit minim dominantly would have no muscle weakness of abductor digit minim.
Extensor digit communis muscle weakness was almost accompanied with abductor digit minim muscle weakness in our study. As extensor digit communis would be contributed by C7 and C8 motor segment, this resulted from involvement of the C8 motor segment.
Deep tendon reflex and Hoffmann sign
The Hoffmann sign is reported to occur in 60–80% of patients with cervical compressive myelopathy, and it is therefore a useful neurological sign affecting pyramidal tracts.9, 10 This sign was negative for most patients with C6–7 myelopathy in our study and could be a feature of this condition, and it indicated involvement of C8 segment. Chikuda et al.11 reported that in patients with cervical compressive myelopathy hyperreflexia showed the highest sensitivity followed by the Hoffmann sign. In the present study, 15 patients (75%) had exaggerated patella tendon reflex and only 2 patients had positive Hoffmann sign.
Neurological level diagnosis
In summary, the neurological findings of C6–7 myelopathy could coexist with involvement of the C8 segment or T1 segment and C7 nerve root.
Neurological examination of patients with cervical compressive myelopathy according to neuroimaging is reported to be moderately accurate and reliable for determining the neurological level of disease. However, Seichi et al.7 reported that responsible levels in some patients could not be determined by neuroimaging when there were multiple increased signal changes. MRI can also show spinal cord compression or increased signal intensity changes despite clinically asymptomatic presentation.12 Although SCEPs may carry risks of infection or cerebral fluid leakage, multimodal SCEPs have some advantages. We have diagnosed the responsible level by using SCEPs to investigate the dysfunction of spinal cord when MRI showed compressions at several levels. We performed the level diagnosis of cervical compressive myelopathy based on SCEP abnormalities rather than on MRI findings. However, the neurological findings were not always concordant with the electrophysiological diagnosis. This resulted from the lesions of the spinal cord because of compression, and therefore they vary widely. Another reason is that the myotomal distribution varies between different individuals. It is therefore difficult to accurately identify the responsible level, and this was a limitation of our study.
Central motor conduction time
Measurement of central motor conduction time is a useful way to assess electrophysiological functioning of the corticospinal tract in patients with cervical compressive myelopathy, and it has been widely reported as a non-invasive and objective method for evaluating the central motor pathway.13, 14 However, the central motor conduction time in abductor digit minim tended to be less prolonged in patients with C6–7 myelopathy, with the central motor conduction time in abductor halluces more obviously prolonged. We previously reported that central motor conduction time in abductor digit minim can be a useful examination tool for the screening of cervical compressive myelopathy that is rostral to the C5–6 level.14 Nakanishi et al.15 reported that low central motor conduction time in abductor digit minim/central motor conduction time in abductor halluces ratios provide complementary information for the screening of patients with thoracic myelopathy. In fact, however, the sensitivity of central motor conduction time in abductor halluces for C6–7 myelopathy could be high, and the sensitivity of central motor conduction time in abductor digit minim could be very low. Diagnosis of the patients with myelopathy caudal C6–7 should include assessment of central motor conduction time in abductor halluces.
Differential diagnosis of C6–7 myelopathy
The neurological findings were consistent with the involvement of segment and long tracts. Involvement of long tracts would be consistent with numbness, sensory disturbance,2, 16 clumsiness of hands17 and prolongation of central motor conduction time.18, 19 Hand symptoms tend to be obvious in more proximal levels than C6–7. Both segment and long tracts correlated with hands became damaged in more upper levels than C6–7, but only segment correlated with hands in C6–7. It is also possible to explain negative Hoffmann sign and the absence of hand symptoms in patients with C6–7 myelopathy. The explanation could be that the anatomical features that compressed the spinal cord at the C6–7 could lead to involvement of the C8 segment and the long tract caudal to T1, or to involvement of the T1 segment and long tract caudal to T2. Therefore, the neurological and electrophysiological findings in C6–7 were characteristic.
Thoracic myelopathy and lumbar stenosis diseases must be considered in the differential diagnosis of C6–7 myelopathy, as patients with this condition would not be detected by neurological abnormalities in their hands.
Some authors7, 20 reported that sensory disturbance in the little finger with or without involvement of the ring finger was accurate for the diagnosis of C6–7 myelopathy. If the patients’ major complaint is gait disturbance, it is important to carefully examine the clinical findings from their hand and assess diagnostic imaging including the cervicothoracic junction. The characteristic symptoms make diagnosis challenging and could potentially lead to misdiagnosis and the subsequent progression of myelopathy, thus resulting in poor outcomes.
Conclusion
We assessed neurological examination and electrophysiological findings for the diagnosis of C6–7 myelopathy. Almost half of the patients could not be detected by neurological abnormalities in their hands, and central motor conduction time in abductor digit minim tended to be less prolonged.
Surgeons should bear in mind possible disorders of caudal C6–7 when they encounter patients with no or few symptoms in the hands and with leg weakness or numbness.
Data Archiving
There were no data to deposit.
References
Tani T, Yamamoto H, Kimura J . Cervical spondylotic myelopathy in elderly people: a high incidence of conduction block at C3-4 or C4-5. J Neurol Neurosurg Psychiatry 1999; 66: 456–464.
Imajo Y, Kato Y, Yonemura H, Kanchiku T, Suzuki H, Taguchi T . Relative vulnerability of various spinal tracts in C3-4 cervical spondylotic myelopathy: multi-modal spinal cord evoked potentials. Spinal Cord 2011; 49: 1128–1133.
Kanchiku T, Taguchi T, Kaneko K, Fuchigami Y, Yonemura H, Kawai S . A correlation between magnetic resonance imaging and electrophysiological findings in cervical spondylotic myelopathy. Spine 2001; 26: 269–274.
Brain L, Watson J . Brain's Disease of the Nervous System, 7th edn. Oxford Univesity press: London, UK. 1969, 40–43.
Yoss RE . Significance of symptoms and signs in localization of involved root in cervical disc protrusion. Neurology 1958; 7: 674–685.
Louis R . Surgery of the Spine Surgical Anatomy and Operative Approaches. Spiringer-Verlag: Berlin/Heidelberg/New York. 1983, 86–116.
Seichi A, Takeshita K, Kawaguchi H, Matsudaira K, Higashikawa A, Ogata N et al. Neurologic level diagnosis of cervical stenotic myelopathy. Spine 2006; 31: 1338–1343.
Chiba T, Konoeda F, Higashibara M, Kamiya H, Oishi C, Hatanaka Y et al. C8 and T1 innervation of forearm muscles. Clin Neulophysiol 2015; 4: 837–842.
Rhee JM, Heflin JA, Hamasaki T, Freedman B . Prevalence of physical sign in cervical myelopathy. A prospective, controlled study. Spine 2009; 34: 890–895.
Houten JK, Noce LA . Clinical correlation of cervical myelopathy and the Hoffmann sign. J Neurosurg Spine 2008; 9: 237–242.
Chikuda H, Seichi A, Takeshita K, Shoda N, Ono T, Matsudaira K et al. Correlation between pyramidical signs and the severity of cervical myelopathy. Eur Spine J 2010; 19: 1684–1689.
Nakashima H, Yukawa Y, Suda K, Yamagata M, Ueta T, Kato F . Abnormal findings on magnetic resonance images of the cervical spines in 1211 asymptomatic subjects. Spine 2015; 40: 392–398.
Di Lazzaro V, Restuccia D, Colosimo C, Tonali P . The contribution of magnetic stimulation of the motor cortex to the diagnosis of cervical spondylotic myelopathy. Correlation of central motor conduction to distal and proximal upper limb muscles with clinical and MRI findings. Electrienceph Clin Neurophysiol 1992; 85: 311–320.
Funaba M, Kanchiku T, Imajo Y, Suzuki H, Yoshida Y, Nishida N et al. Transcranial magnetic stimulation in the diagnosis of cervical compressive myelopathy; comparison with spinal cord evoked potentials. Spine 2015; 40: E161–E167.
Nakanishi K, Tanaka N, Sasaki H, Kamei N, Hamasaki T, Yamada K et al. Assessment of central motor conduction time in the diagnosis of compressive thoracic myelopathy. Spine 2010; 35: E1593–E1598.
Ichihara K, Taguchi T, Sakuramoto I, Kawano S, Kawai S . Mechanism of the spinal cord injury and the cervical spondylotic myelopathy: new approach based on the mechanical features of the spinal cord white and gray matter. J Neurosurg 2003; 99: 278–285.
Ono K, Ebara S, Fuji T, Yonenobu K, Fujiwara K, Yamashita K . Myelopathy hand. New clinical sign of cervical cord damage. J Bone Joint Surg Br 1987; 69: 215–219.
Kaneko K, Taguchi T, Morita H, Yonemura H, Fujimoto H, Kawai S . Mechanism of prolonged central motor conduction time in compressive cervical myelopathy. Clin Neurophysiol 2001; 6: 1035–1040.
Nakanishi K, Tanaka N, Fujiwara Y, Kamei N, Ochi M . Corticospinal tract conduction block results in the prolongation of central motor conduction time in compressive cervical myelopathy. Clin Neurophysiol 2006, 623–627.
Matsumoto M, Ishikawa M, Ishii K, Nishizawa T, Maruiwa H, Nakamura M et al. Usefulness of neurological examination for diagnosis of the affected level in patients with cervical compressive myelopathy: prospective comparative study with radiological evaluation. J Neurosurg Spine 2005; 2: 535–539.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Disclaimer
The manuscript submitted does not contain information about medical device(s)/drug(s). No benefits in any form have been received or will be received by a commercial party related directly or indirectly to the subject of this article.
Rights and permissions
About this article
Cite this article
Funaba, M., Kanchiku, T., Imajo, Y. et al. Characteristics of C6–7 myelopathy: assessment of clinical symptoms and electrophysiological findings. Spinal Cord 54, 798–803 (2016). https://doi.org/10.1038/sc.2015.203
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2015.203
This article is cited by
-
Funicular pain: a case report of intermittent claudication induced by cervical cord compression
BMC Musculoskeletal Disorders (2020)
-
Grip force control during object manipulation in cervical myelopathy
Spinal Cord (2020)
-
The contribution of neurophysiology in the diagnosis and management of cervical spondylotic myelopathy: a review
Spinal Cord (2016)