Abstract
Study design:
This is a mixed-method consensus development project.
Objectives:
The objective of this study was to identify a top ten list of priorities for future research into spinal cord injury (SCI).
Setting:
The British Spinal Cord Injury Priority Setting Partnership was established in 2013 and completed in 2014. Stakeholders included consumer organisations, healthcare professional societies and caregivers.
Methods:
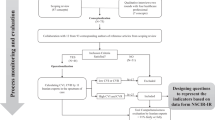
This partnership involved the following four key stages: (i) gathering of research questions, (ii) checking of existing research evidence, (iii) interim prioritisation and (iv) a final consensus meeting to reach agreement on the top ten research priorities. Adult individuals with spinal cord dysfunction because of trauma or non-traumatic causes, including transverse myelitis, and individuals with a cauda equina syndrome (henceforth grouped and referred to as SCI) were invited to participate in this priority setting partnership.
Results:
We collected 784 questions from 403 survey respondents (290 individuals with SCI), which, after merging duplicate questions and checking systematic reviews for evidence, were reduced to 109 unique unanswered research questions. A total of 293 people (211 individuals with SCI) participated in the interim prioritisation process, leading to the identification of 25 priorities. At a final consensus meeting, a representative group of individuals with SCI, caregivers and health professionals agreed on their top ten research priorities.
Conclusion:
Following a comprehensive, rigorous and inclusive process, with participation from individuals with SCI, caregivers and health professionals, the SCI research agenda has been defined by people to whom it matters most and should inform the scope and future activities of funders and researchers for the years to come.
Sponsorship:
The NIHR Oxford Biomedical Research Centre provided core funding for this project.
Similar content being viewed by others
Introduction
Over the past decade, public and patient involvement (PPI) in setting healthcare research agendas and developing subsequent research projects has gathered serious momentum in the United Kingdom and elsewhere.1 PPI in healthcare research comes with a range of perceived benefits, including healthcare service users’, or consumers’, increased awareness and knowledge about their condition, as well as researchers’ greater understanding and insight into the medical and social implications of the medical condition under study.2 Moreover, PPI helps identify relevant research topics, it improves appropriateness of outcome measures used in research and it assures that study findings are being disseminated in a user-friendly way.3, 4 Finally, setting the right and relevant research priorities by people to whom it matters most is one way of reducing waste and costs associated with redundant research activities.5
Although substantial progress has been made with regard to PPI in medical areas such as oncology,6, 7 dementia care8 and internal medicine,9 little is known about patients’, caregivers’ and healthcare professionals’ preferred research questions into spinal cord injury (SCI). Many esteemed experts in SCI research have co-authored papers outlining recommendations and guidance for future research activities.10, 11, 12, 13 However, these guiding documents do contain little to no considerations from consumers’ perspectives.
The quality of life of people living with SCI is determined by a range of factors. Not only do health issues, including motor, bowel, bladder and sexual functions, have a substantial impact on the consumers’ well-being, other social aspects of life such as relationships with friends and family members or employment are equally important determinants.14 In their comprehensive review, Simpson et al.14 propose a closer alignment between identified health and life domains and research being carried out by academics. However, priorities for personal well-being do not always translate into research priorities easily. For instance, although relationships with friends and family members have been identified as the highest life domain priority among people with SCI,14 this does not necessarily mean that the same people wish for researchers to carry out further research into this aspect. Thus, although the questions ‘what matters most to you’ and ‘what do you think researchers should investigate’ may cover similar areas, in essence these two questions have a different meaning and therefore answers to these questions cannot be simply interchanged.
Although results from a number of small-scale SCI research priority workshops have been published in the literature,15, 16 to the authors’ knowledge no results of a systematic, consumer-focused national priority setting exercise for SCI research has been published so far. Here, we describe the methodology and the results of a recently completed British, multi-stakeholder priority setting partnership for SCI research.
Materials and Methods
Setting up the partnership
The British Spinal Cord Injury Priority Setting Partnership was established in 2013, with the first stakeholder meeting held in April 2013. Stakeholders included (i) consumer organisations (Spinal Injuries Association, Cauda Equina Syndrome UK Charity and Transverse Myelitis Society); (ii) healthcare professional societies (British Association of Spine Surgeons, Society of British Neurological Surgeons, UK Spine Societies Board, Multidisciplinary Association of Spinal Cord Injury Professionals and British Association of Spinal Cord Injury Specialists); and (iii) caregiver representatives. Support and guidance was provided by the James Lind Alliance (JLA)—a National Institute for Health Research (NIHR)-supported organisation, which aims to identify gaps in scientific, medical and psychosocial knowledge that matters most to patients, caregivers and health professionals—and the Stoke Mandeville Spinal Foundation (now called Stoke Mandeville Spinal Research), a research charity promoting the conduct of meaningful, world-class research into SCI. Other partner organisations that supported this PSP are shown in Supplementary Table 1.
Adults with spinal cord dysfunction due to trauma or non-traumatic causes, including transverse myelitis, and individuals with a cauda equina syndrome (henceforth grouped and referred to as SCI) were invited to participate in this priority setting partnership. The Steering Group comprised representatives from each stakeholder organisation, including an independent information manager (HCA); they met face to face four times and participated in monthly teleconferences throughout 2013 and 2014. During these meetings, a protocol detailing the methods was developed, and the progress of the entire process was monitored. The project protocol was primarily based on the methodology described in the JLA Guidebook, which has been used to set priorities across a range of healthcare conditions.17 The protocol covered the following four key stages:
-
i)
Gathering of research questions.
-
ii)
Grouping questions and checking of existing research evidence.
-
iii)
Open interim prioritisation to identify the 25 highest ranked priorities.
-
iv)
A final consensus meeting to reach agreement on the top ten research priorities.
The Steering Group had voting rights and the mandate to reword research questions where needed, while ensuring that the original meaning of the question was not lost. The NIHR Oxford Biomedical Research Centre provided core funding for this project, with partners, including individual patients, caregivers and clinicians, contributing with their time and expertise on a voluntary basis.
Stage I: Gathering research questions
A survey was developed for collecting research questions; see Supplementary Document 1. Part A of the questionnaire covered various questions about the survey participants and part B covered the key survey question: ‘What question(s) would you like researchers to answer that will help improve the treatment and care of people living with SCI?’ Participants were encouraged to keep questions concise and were advised that there was no limit to the number of questions to pose. A pilot survey was tested on five patients and five healthcare professionals, and comments were incorporated into the final survey version. Next, an online survey version was developed, and during a period of three months anyone residing in Britain with an interest in SCI was invited to participate. Participants were also given the option of being provided with a paper version. Information about the survey was widely disseminated to targeted survey participants through service user organisations, professional societies and hospitals. Advertisements inviting people to participate were also displayed in specialist SCI centres across the UK.
In all, 403 respondents submitted a total of 784 entries. Table 1 presents the profiles of respondents.
Stage II: Processing research questions
This stage was carried out by the information manager, whose role was to determine, from all the entries submitted, those that were SCI research questions that had not yet been adequately answered by research. All steps were double-checked by the lead author, as well as by the Steering Group. The steps taken include the following:
-
1
Removing entries that were not specifically concerned with SCI, addressed paediatric SCI or that were not researchable questions.
-
2
Grouping questions into categories so that questions addressing similar topics and aspects were grouped together.
-
3
Identifying duplicate questions within each category and agreeing on wording to merge these questions where appropriate.
-
4
Converting, where possible, entries to Patient, Intervention, Comparison and Outcome (PICO) format.
-
5
Systematically searching published literature (using the Medline database, PubMed interface and Cochrane database) for existing systematic reviews and randomised controlled trials published within the past 10 years that adequately answer the research question and remove these from the data. Literature showing either conflicting results on the effects of interventions or substantial methodological shortcomings were deemed inconclusive.
-
6
Develop the ‘long list’ of research questions known as uncertainties.
Following these steps, the list of 784 original entries was narrowed down to a long list of 109 SCI research uncertainties. The research uncertainties fell into the following (arbitrary) categories: ‘Access to and organisation of healthcare’ (n=12), ‘Ageing’ (n=3), ‘Arm and hand function’ (n=8), ‘Assistive technologies and engineering’ (n=6), ‘Autonomic system and dysreflexia’ (n=1), ‘Bladder’ (n=10), ‘Bladder and bowel’ (n=2), ‘Bowel’ (n=2), ‘Breathing’ (n=3), ‘Cardiovascular and lymphatic’ (n=2), ‘Cure, repair and regeneration’ (n=10), ‘Diagnosis and prognosis’ (n=6), ‘Fatigue’ (n=1), ‘Fitness, mobility and walking’ (n=5), ‘Medical devices and orthotics’ (n=3), ‘Medication’ (n=4), ‘Nutrition and weight management’ (n=4), ‘Pain’ (n=5), ‘Posture and musculoskeletal’ (n=1), ‘Psychology and coping’ (n=3), ‘Recurrence of transverse myelitis’ (n=6), ‘Skin and pressure sores’ (n=3), ‘Spasticity’ (n=8), ‘Surgical and acute management’ (n=4) and ‘Syringomyelia’ (n=2).
Stage III: Open interim prioritisation
A second online interim survey with the long list of uncertainties was conducted for 6 weeks between May and June 2014. Similar to stage I, this interim survey was widely disseminated, and those with an interest in SCI were invited to take part. The wording of the long list of uncertainties was reviewed by the Steering Group, and wording in some cases was altered to make the uncertainty more understandable or glossary terms were added to explain complex words that may not be generally well known to the public. Uncertainties were grouped in themes, for example, ‘Arm and hand function’, which were presented in alphabetical order. Survey participants were asked to vote on how they would prioritise research for each uncertainty on a scale of 1 to 5 (1 being not a priority, 5 being a very high priority). Results of this prioritisation stage were disseminated by the information manager, and uncertainties were ranked in the order of priority following non-weighted, frequency statistic analysis.
A total of, 293 participants completed the online interim survey and voted on the priority of researching each uncertainty. The demographics of the survey participants were very similar to those of stage I; for a breakdown of interim survey respondents, see Supplementary Table 2. There was considerable similarity between the top priorities as voted for by patients and by healthcare professionals (data available upon request). Although the top 25 uncertainties were taken to the final workshop, all of the 109 research uncertainties have been published on the UK Database of Uncertainties about the Effects of Treatments (UK DUETs), which is accessible online.18
Stage IV: Final consensus meeting
On the basis of the ranked results from the interim survey, the top 25 uncertainties were taken forward for discussion and further prioritisation at a workshop in July 2014. Representatives from partner organisations were invited to the workshop, as well as healthcare professionals, carers and those with SCI. A carefully selected group of 20 representatives—7 patient representatives, 1 caregiver and 11 healthcare professionals—participated in the workshop. The consensus meeting was led by three experienced and independent JLA-affiliated facilitators who ensured that everyone had an equal opportunity to share his or her perspective, and discussions were finished within the pre-specified time slots.
All participants were sent the short list of 25 uncertainties in advance of the workshop and were asked to individually reflect on the research questions, to write down any comments and to rank these questions in order of priority. This enabled participants to be familiar with the uncertainties for discussion at the workshop and to ensure that everyone had something to contribute in the first small-group discussion. After an initial introduction, participants were separated into three small groups with an even mix of patients, carers and healthcare professionals.
The first small-group discussions focused on the similarities and differences between individuals’ rankings. Facilitators used cards with the uncertainty written in the front, laying them on a table so that it was clear for participants to see. Group members were given information about the original submitted entries, which led to this uncertainty, how many submitted questions had contributed to this uncertainty and the previous interim survey voting information. Initial discussion about the uncertainties enabled participants to begin to appreciate different or similar points of view. After this first small-group discussion, the agreed initial ranking of uncertainties from each individual small group was recorded.
In the second small-group session, groups were mixed so that participants were with mostly new people, while keeping an even distribution of patients, carers and healthcare professionals. The cards had been rearranged to show the combined rank of uncertainties so far from the three small groups. This second group session gave participants a second chance to discuss the ranking of the uncertainties with new people, enabling individual groups to challenge the existing ranking of uncertainties. Again, the new ranking of uncertainties from this session was recorded.
In a final large group discussion, all workshop attendees came together at the end of the day to discuss the aggregate ranked list of the uncertainties. Cards were placed on the floor and participants gathered around for the discussion and were asked to focus on agreeing a top 10. This was a final opportunity for participants to make a case for any particular uncertainty and its position in the list before the final result was decided and agreed upon.
Results
The final ranked list of the top 10 uncertainties that was agreed upon during the prioritisation workshop is presented in Table 2. As five research questions were merged into two different research questions during the workshop, the complete ‘post-workshop’ list contained 22 ranked research priorities; see Supplementary Table 3. All of the 109 research uncertainties have been published in the UK DUETs, which is accessible online.18
Discussion
To the authors’ knowledge, this is the first paper to report the results of a systematically conducted, national, multi-stakeholder priority setting exercise for research into SCI. Following a comprehensive, rigorous and inclusive process, with participation from individuals with SCI, caregivers and health professionals, an SCI research agenda has been defined by people to whom it matters most and should inform the scope and future activities of funders and researchers for the years to come. Involvement of both the public and healthcare professionals has given this top 10 list credibility and face validity, which should prompt both academia and research funding bodies to reconsider their research themes and funding streams. The outcomes of this partnership resonated public hope surrounding stem cell research into SCI.19 However, nine other practical research priorities clearly indicate that SCI research involves much more areas than cell therapies alone.
The number one research priority addresses the effects of activity-based interventions during SCI rehabilitation. Activity-based interventions comprise a variety of approaches, which aim to restore muscle function and sensation below the spinal cord lesion rather than compensating strength and agility of intact muscle groups above the lesion. As such activity-based interventions are also being called activity-based restorative therapies (ABRTs). However, the exact meaning of these terminologies remains ambiguous and should prompt investigators to report specifications of the ABRTs under study carefully. Research into ABRTs has intensified over the past decade, and although positive preliminary outcomes have been reported, the optimal duration, intensity, timing and patient profiles for ABRTs are yet to be determined.20
Because of lack of space, we cannot discuss the rest of the identified research priorities in detail. However, it merits highlighting the absence of three medical conditions that are frequently encountered in the SCI population in the top 10: neuropathic pain, sexual dysfunction and pressure ulcers. After the interim prioritisation stage (stage III), the highest ranked question on neuropathic pain was ‘Is Gabapentin safe and effective to use for reducing neuropathic pain in SCI patients?’. This question was ranked place 29, and thus it did not proceed to the final workshop. The Steering Group was surprised not to see any question concerning neuropathic pain featuring in the top 25 questions and no explanation could be found for this. Although a number of questions about sexual dysfunction were raised in stage I, for example, ‘How can sex be improved? There needs to be more help at the rehabilitation phase.’, no specific research questions were raised on this topic, and hence no question covering this aspect was included in the interim-prioritisation survey. It has been shown that sexual dysfunction has a significant impact on one’s quality of life.21 However, surprisingly enough our results demonstrate that this particular domain does not elicit a strong call for research into this topic.
Although the question ‘Which wheelchair cushions are most effective in prevention of pressure ulcers in wheelchair users after spinal cord injury?’ was discussed during the final workshop and ranked place 19, the reason for not ending up any higher can primarily be explained by the outcomes of the ‘James Lind Alliance Pressure Ulcer Partnership’. In their top 12 research priorities for pressure ulcers,22 research priority number four (that is, ‘What is the relative effectiveness of the different types of pressure relieving beds, mattresses, overlays, heel protectors and cushions (including cushions for electric and self-propelling wheelchairs) in preventing pressure ulcers?’) broadly covered the question raised during the SCI priority setting partnership. As this question had already been flagged up by the pressure ulcer partnership, the workshop participants felt that there was no priority to include a similar question in the top ten list for SCI research priorities.
Our results confirmed the hypothesis that previously identified priorities for personal well-being after SCI cannot simply be translated into SCI research priorities. In their review, Simpson and colleagues distinguished two broad domains of priorities among individuals with SCI: a health and a life domain.14 The results of SCI priority setting partnership clearly demonstrate that the large majority of identified research fall into the health domain.
So far, little research has been published on involving consumers in defining actual research priorities for SCI. In 2006, Abma15 published results of a feasibility study using a ‘participatory methodology’ for defining an SCI research agenda in The Netherlands. In this small-scale study, three key stakeholders were involved, namely the Dutch SCI consumer organisation, researchers and healthcare professionals. A list of six non-ranked research themes was compiled following analysis of three interviews with researchers, three interviews with consumers and two focus groups in which a total of twelve consumers and one caregiver participated. The results of the current research priority partnership represent the perspectives and input from a large group of stakeholders across Britain. Although similar research prioritisation exercises to be conducted in Western Europe may yield similar outcomes,23 the generalisability of the identified top 10 research priorities may be limited in other countries because of cultural differences and varying systems of care.
Several discussions about the survey’s inclusion criteria were held at the beginning of this partnership. As individuals living with SCI face a range of identical medical and psychosocial issues no matter what caused the spinal cord lesion, adults with a variety of causes of acquired spinal cord lesions—(non-)traumatic SCI, transverse myelitis and cauda equina syndrome—were invited to participate. Survey participants were advised that research questions concerning SCI in children were not processed, as this is a highly specialised area deserving specific attention. An international collaboration of healthcare professionals with an interest in paediatric SCI is currently preparing an international research prioritisation exercise using a different methodology, which allows accommodating for different languages. In line with the JLA’s philosophy, the Steering Group did not encourage scientists and full-time clinical researchers to participate in the surveys/workshop. However, it was impossible to exclude them from participating in online surveys (stage I and III). Notwithstanding the exclusion of scientists from the current priority setting exercise, the Steering Group hopes to see the identified research priorities being taken forward to a balanced dialogue between SCI health service users and scientists.
A key strength of our work is PPI involvement throughout the entire process of this partnership. Rather than academics alone, this project has been led by representatives from a wide range of consumer and healthcare professional organisations. In addition, the wide range of consumers involved in this project—for example, both newly injured and chronic SCI subjects with a variety of causes, levels and severities of spinal cord lesions—resulted in a balanced representation of the entire SCI community. Nonetheless, despite efforts to involve more caregivers at each stage of the prioritisation process, we had a small response rate from this group and so it is acknowledged that further work is needed to involve this group in future prioritisation of research. A substantial number of entries received during stage I did not address a research question specifically. For instance, some participants asked ‘when will a cure be found’, and others asked questions about the organisation and access to healthcare services for SCI. Although these questions did not proceed to stage III, most of these questions were grouped as ‘non-researchable questions’, and a collated list was sent to partner organisations, which allowed them to review their supportive and educational materials and see whether these questions had already been addressed or not. Other entries were brief and covered a topic—for instance, ‘bowel function’ without specifying the actual research question. These examples demonstrate that there is scope for optimising input from PPI through improving public understanding of how to frame a research question. Organisations promoting PPI, such as the NIHR-funded advisory group ‘INVOLVE’, have begun to address these issues and have published a number of PPI training materials. Future healthcare consumer survey studies should signpost to these materials.
Although this research prioritisation project has reached its objectives, there are—as of yet—no plans to monitor the impact of its outcomes. Two key questions about the impact of PPI remain to be elucidated: (i) whether funders will confidently support priorities identified by non-academic stakeholders, and (ii) whether funded research on identified priority areas indeed contributes a meaningful difference to the SCI community.24 Since the first brief communication of the top 10 research priorities results,25 the Steering Group has had a number of dialogues with research funding bodies, including the NIHR. The closure of this SCI research priority setting partnership has led to a call to action: SCI researchers should take on the priorities identified in this partnership, design appropriate studies and convince funding organisations about the best ways of achieving scientific progress in these identified areas of research.
Data Archiving
There were no data to deposit.
References
Parkes JH, Pyer M, Wray P, Taylor J . Partners in projects: preparing for public involvement in health and social care research. Health Policy 2014; 117: 399–408.
Brett J, Staniszewska S, Mockford C, Herron-Marx S, Hughes J, Tysall C et al. A systematic review of the impact of patient and public involvement on service users, researchers and communities. Patient 2014; 7: 387–395.
Petit-Zeman S, Locock L . Health care: bring on the evidence. Nature 2013; 501: 160–161.
Brett J, Staniszewska S, Mockford C, Herron-Marx S, Hughes J, Tysall C et al. Mapping the impact of patient and public involvement on health and social care research: a systematic review. Health Expect 2014; 17: 637–650.
Chalmers I, Bracken MB, Djulbegovic B, Garattini S, Grant J, Gülmezoglu AM et al. How to increase value and reduce waste when research priorities are set. Lancet 2014; 383: 156–165.
Pattison N, Lee M . Two tribes coming together: patient and public involvement in cancer research. Eur J Cancer Care 2014; 23: 1–2.
Thompson J, Bissell P, Cooper CL, Armitage CJ, Barber R . Exploring the impact of patient and public involvement in a cancer research setting. Qual Health Res 2014; 24: 46–54.
Iliffe S, McGrath T, Mitchell D . The impact of patient and public involvement in the work of the Dementias & Neurodegenerative Diseases Research Network (DeNDRoN): case studies. Health Expect 2011; 16: 351–361.
Hull D, Barton D, Guo K, Russell C, Aucott B, Wiles D . Patient and public involvement to support liver disease research. Br J Nurs 2012; 21: 972–976.
Ditunno JF Jr, Burns AS, Marino RJ . Neurological and functional capacity outcome measures: essential to spinal cord injury clinical trials. J Rehabil Res Dev 2005; 42: 35–41.
Groah SL, Charlifue S, Tate D, Jensen MP, Molton IR, Forchheimer M et al. Spinal cord injury and aging: challenges and recommendations for future research. Am J Phys Med Rehabil 2011; 91: 80–93.
Heinemann AW, Steeves JD, Boninger M, Groah S, Sherwood AM . State of the Science in Spinal Cord Injury Rehabilitation 2011: informing a new research agenda. Spinal Cord 2012; 50: 390–397.
Tate DG, Boninger ML, Jackson AB . Future directions for spinal cord injury research: recent developments and model systems contributions. Arch Phys Med Rehabil 2011; 92: 509–515.
Simpson LA, Eng JJ, Hsieh JT, Wolfe DL . The health and life priorities of individuals with spinal cord injury: a systematic review. J Neurotrauma 2012; 29: 1548–1555.
Abma TA . Patients as partners in a health research agenda setting: the feasibility of a participatory methodology. Eval Health Prof 2006; 29: 424–439.
Weaver FM et al. Creating a research agenda in SCI based on provider and consumer input. SCI Psychosocial Process 2001; 14: 77–88.
Cowan K, Oliver S . The James Lind Alliance Guidebook 2013.
UK Database of Uncertainties about the Effects of Treatments (UK DUETs). Uncertainties: spinal cord diseases. http://www.library.nhs.uk/duets/SearchResults.aspx?tabID=294&catID=15617 (Last accessed on 2 November 2015).
Granger N, Franklin RJ, Jeffery ND . Cell therapy for spinal cord injuries: what is really going on? Neuroscientist 2014; 20: 623–638.
Jones ML, Harness E, Denison P, Tefertiller C, Evans N, Larson CA . Activity-based therapies in spinal cord injury: clinical focus and empirical evidence in three independent programs. Top Spinal Cord Inj Rehabil 2012; 18: 34–42.
Noreau L, Noonan VK, Cobb J, Leblond J, Dumont FS . Spinal cord injury community survey: a national, comprehensive study to portray the lives of Canadians with spinal cord injury. Top Spinal Cord Inj Rehabil 2014; 20: 249–264.
James Lind Alliance Pressure Ulcer Partnership (JLAPUP). Top 12 pressure ulcer research priorities. https://www.york.ac.uk/news-and-events/news/2013/research/pressure-ulcer-research/ (Last accessed on 2 November 2015).
Kennedy P, Lude P, Taylor N . Quality of life, social participation, appraisals and coping post spinal cord injury: a review of four community samples. Spinal Cord 2006; 44: 95–105.
Petit-Zeman S, Firkins L, Scadding JW . The James Lind Alliance: tackling research mismatches. Lancet 2010; 376: 667–669.
van Middendorp JJ, Allison H, Cowan K . Top ten research priorities for spinal cord injury. Lancet Neurol 2014; 13: 1167.
Acknowledgements
This project was supported by funding provided by the NIHR Oxford Biomedical Research Centre. This project was undertaken by the Stoke Mandeville Spinal Research, a research charity.
Disclaimer
The work presented here represents the views of the authors and not necessarily those of the funding bodies.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on the Spinal Cord website
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
van Middendorp, J., Allison, H., Ahuja, S. et al. Top ten research priorities for spinal cord injury: the methodology and results of a British priority setting partnership. Spinal Cord 54, 341–346 (2016). https://doi.org/10.1038/sc.2015.199
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2015.199
This article is cited by
-
The effect of early mobilisation (< 14 days) on pathophysiological and functional outcomes in animals with induced spinal cord injury: a systematic review with meta-analysis
BMC Neuroscience (2024)
-
Surveying people with spinal cord injuries in Brazil to ascertain research priorities
Scientific Reports (2023)
-
Research priorities to enhance life for people with spinal cord injury: a Swedish priority setting partnership
Spinal Cord (2023)
-
Approaches to prioritising research for clinical trial networks: a scoping review
Trials (2022)
-
Grieving a disrupted biography: an interpretative phenomenological analysis exploring barriers to the use of mindfulness after neurological injury or impairment
BMC Psychology (2021)