Abstract
Study design:
Mixed retrospective-prospective cohort study.
Objectives:
To determine psychological and socioeconomic status, complications and quality of life in people with spinal cord injuries (SCI) after discharge from a hospital in Bangladesh.
Setting:
Bangladesh.
Methods:
All patients admitted in 2011 with a recent SCI to a hospital in Bangladesh were identified. Patients were interviewed by telephone in 2014 using translated versions of the SF12, the SCI Secondary Conditions Scale, the Centre for Epidemiologic Studies Depression Scale (CESDS) and the Participation Component of the WHODAS. Questions were also asked about employment, living and financial situation, and opportunities to get out of bed and out of the house. Data were stratified by ability to walk on discharge.
Results:
A total of 350 people were discharged with a recent SCI in 2011. By 2014, 55 had died. Of those still living, 283 were interviewed (96% follow-up rate). At the time of interview, 47% of participants were employed. One-quarter (26%) of those who were wheelchair-dependent had a pressure ulcer. The mean (s.d.) scores for the Mental and Physical Component of the SF12 were 32.0 points (5.5) and 35.8 points (3.9), respectively. The median (interquartile range) scores for the SCI Secondary Conditions Scale, CESDS and WHODAS for those who were wheelchair-dependent were 15% (10 to 19), 11 points (9 to 18) and 26 points (23 to 26), respectively.
Conclusion:
Many people with SCI in Bangladesh are house-bound, unemployed, living in poverty and have pressure ulcers. They experience moderate rates of depression and report limited quality of life.
Similar content being viewed by others
Introduction
Living with a spinal cord injury (SCI) in low and middle income countries (LMICs) is challenging. Support for people with SCI is often limited and wheelchair access may be very restricted. Our impression, based on clinical experience, is that many people living with SCI in Bangladesh and other LMICs have a high incidence of secondary complications and a limited quality of life (QOL). Many studies have investigated QOL and incidence or prevalence of complications after SCI in high income countries.1, 2, 3 Some studies have also examined these issues in LMICs.4, 5, 6, 7 However, few studies sample in a representative way—most, instead, rely on samples of convenience. Therefore, we sought to determine the psychological and socioeconomic status, complications, and QOL in people living with SCI in Bangladesh after discharge from hospital. We were particularly interested in the outcomes of people who were wheelchair-dependent because the challenges for these people are greatest. We sampled a consecutive cohort of people with SCI from the time they were discharged from hospital to ensure the sample was as representative as possible of people living in a LMIC.
Materials and Methods
Design
This study was part of a larger cohort study designed to determine survival following SCI in Bangladesh. The methods and survival data have been published elsewhere.8 In brief, all patients admitted with SCI to a large hospital in Bangladesh in 2011 were followed up by telephone in 2014. Consequently, the study was a mixed retrospective-prospective cohort study. The focus of this manuscript is the sub-cohort consisting of those who were still alive in 2014. The study received ethical approval (CRP/RE/0401/98) from the Centre for the Rehabilitation of the Paralysed (CRP) and was conducted in accordance with the Declaration of Helsinki. Participants provided informed consent.
Site and participants
Site
The cohort was drawn from patients admitted to CRP. The CRP admits approximately 390 people with recent SCI each year making it one of the largest SCI centres in the world.9, 10 It serves all people from Bangladesh regardless of income. Most patients make a small financial contribution to their care on the basis of ability to pay, but care is primarily funded by the government and not-for-profit organisations. The centre provides acute care and comprehensive inpatient rehabilitation.
Participants
The cohort was identified retrospectively from hospital records in 2014. It included all patients admitted to the CRP in 2011 with a recent SCI (less than 1 year) who were subsequently discharged home. Three sets of hospital records were cross-checked to ensure all potential participants were identified. The hospital records were used to identify the cause of injury (traumatic or non-traumatic), the date of injury, American Spinal Injuries Association Impairment Scale (AIS scores A–E)11 and the type of injury (tetraplegia or paraplegia).
Outcome
Cohort members were contacted and interviewed by telephone between March and December in 2014 (five people were interviewed in person). The following data were obtained:
Socioeconomic status
Participants were asked about their current and previous (that is, prior to SCI) marital status, accommodation, income and family support.
SCI Secondary Conditions Scale
This is a standardised assessment12 that requires participants to rate 15 common secondary complications of SCI on a 4-point scale anchored at one end with ‘not experienced in the last 3 months or not a significant problem’ and at the other end with ‘severe and chronic problem’. The telephone version of this scale has recently been validated.13 The list of complications includes those related to pressure ulcers, bladder and bowel incontinence, pain, poor blood pressure control, contractures and spasm. Responses to each item are tallied. High scores are indicative of many, chronic and severe complications. Scores were expressed as a percentage of the total possible score.
Presence of pressure ulcers
Participants were asked whether they currently had a pressure ulcer. They were only required to provide a ‘yes’ or ‘no’ response.
Out of bed and out of house questionnaire
This is a 2-item questionnaire that was designed specifically for the purpose of this study and the Bangladeshi context. The two questions were:
-
1
Have you got out of bed in the last week (yes/no)? If yes, on how many days did you get out of bed in the last week (excluding days in which you only got out of bed for toileting or showering).
-
2
Have you been out of the bounds of your home in the last week (yes/no)? If yes, on how many days did you leave the bounds of your home in the last week?
The World Health Organisation Disability Assessment Scale (WHODAS)—Participation Items (V2.0)
This is a standardised assessment of participation,14, 15 chosen because it has previously been used successfully in Bangladesh and is available in Bangla. It consists of eight questions each rated on a 5-point scale with the following anchors: ‘none’, ‘mild’, ‘moderate’, ‘severe’ and ‘extreme (or cannot do)’. The self-administered version was used even though the questions were read out over the phone. Scores are tallied to provide an overall score with a total possible score of 40 where 0 represents no problems with community participation and 40 represents extreme problems with participation.
The SF12
This is a standardised assessment of QOL. It comprises 12 questions that are rated on a 2–6-point scale depending on the question. It has been translated into Bangla, and both this and the longer SF36 have been used previously in Bangladesh.16, 17 The Physical Component Summary and the Mental Component Summary scores were obtained using the standard algorithm on the basis of US general population means and s.d. unadjusted for age and gender. Higher scores indicate better QOL. Scores were standardised so that 50 represented average functioning and the s.d. was 10 (that is, a score of 30 is equivalent to the lowest 2% of the American population).
Center for Epidemiologic Studies Depression Scale (CESDS)
This instrument is widely used to screen for depression and depressive disorders. It measures symptoms defined by the American Psychiatric Association Diagnostic and Statistical Manual (DSM-IV) for a major depressive episode. It was chosen because it has previously been used in Bangladesh and is available in Bangla.18, 19 The questionnaire contains 20 items each scored on a 4-point scale anchored at one end by ‘rarely or none of the time (less than 1 day)’ and at the other end by ‘most or all of the time (5-7 days)’. Each item refers to emotions felt over the past week. Scores are tallied. The highest possible score is 60 with higher scores indicative of more depressive symptoms. Responses were also analysed to determine the number of participants with possible, probable and major depressive symptoms. These classifications were solely based on whether participants had reported experiencing any symptoms ‘most or all of the time’ in two, three or four of the following domains: sadness (questions 2, 4 and 6), loss of interest (questions 8 and 10), appetite (questions 1 and 18), sleep (questions 5, 11 and 19), thinking (questions 3 and 20), guilt (questions 9 and 17), fatigue (questions 7 and 16), agitation (questions 12 and 13) and suicidal ideation (questions 14 and 15).
Participants were classified as being wheelchair-dependent and walking on the basis of their ability to walk on discharge. Ability to walk on discharge was determined by asking the following question (in Bangla): ‘On discharge, did you require a wheelchair for mobility on a daily basis?’ Ability to walk was used as a surrogate for severity of injury because the data could be easily and reliably collected over the telephone. The ASIA classifications were available from the medical records but were not used because they could not be verified.
Data were analysed descriptively and are reported as means (s.d.) unless skewed in which case they are reported as medians (interquartile ranges, IQR).
Results
Three hundred and fifty participants admitted to CRP in 2011 with a recent SCI survived until discharge (see Figure 1). Of these, 55 died following discharge before being interviewed and 11 were lost to follow-up (including one person who was known to be alive but could not be interviewed). Another participant was excluded because a head injury prevented him from speaking. Thus, 283 of 295 potentially eligible and alive participants (96%) were located and interviewed. The median (IQR) follow-up time was 32.6 months (30.0–35.6 months) since discharge.
The characteristics of the participants interviewed in 2014 are shown in Table 1. Two hundred and fifty-five (90%) participants were male with a median (IQR) age of 30 years (23–42). One hundred and sixty-eight (59%) participants were wheelchair-dependent and 115 (41%) were walking at the time of discharge (see Table 1). Most participants had traumatic tetraplegia (101; 36%) or traumatic paraplegia (170; 60%).
The socioeconomic status of participants is shown in Table 2. Between 1 and 19 participants did not answer particular questions about their social and financial situation (number of responses is indicated in the table). Two hundred and nine (74%) participants were married prior to injury, and of these, 11 separated or divorced after the injury (one participant was separated or divorced prior to injury). Nearly all participants returned to live at a family-owned or rented house or apartment after SCI. Two hundred and forty (85%) participants were working prior to injury and 133 (47%) were working after injury. The characteristics of those working and not working according to dependence on a wheelchair, type of injury, presence of pressure ulcer and CESDS scores are shown in Table 3. Almost two-thirds of those who were wheelchair-dependent and tetraplegic, and 80% of those with CESDS scores greater than 15 (indicative of symptoms of depression) were not working. The family income dropped from a mean of $US26 per person per month to $US20 per person per month following injury and although 190 (67%) participants were the main income earners for families prior to injury, this dropped to 85 (30%) after injury. Most participants relied on spouses or parents for care with only two participants relying on paid carers.
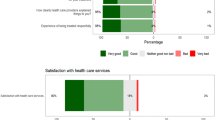
Responses to the SCI Secondary Conditions Scale, WHODAS (participation), SF12, CESD and questions about getting out of bed and home are shown in Table 4 and Figures 2 and 3. One participant did not answer one question of the CESDS. His CESDS data were not included in the analysis. Eleven participants declined to answer the sexuality question on the SCI Secondary Conditions Scale. For this reason, all data for the SCI Secondary Conditions Scale were expressed as a percentage of the total possible score. The numbers of respondents to all questions are indicated in Table 4. Participants had low scores on the SCI Secondary Conditions Scale indicating relatively few serious complications in the 3 months preceding interview. The complications most often reported were pain, spasticity and pressure ulcers, as well as complications associated with bladder, bowel and sexual dysfunction (see Figure 2). Forty-three (26%) participants who were wheelchair-dependent and two other participants (2%) who were walking had a pressure ulcer at the time of interview (see Table 4). In addition, more than 75% of participants who were wheelchair-dependent indicated on the SCI Secondary Conditions Scale that pressure ulcers had been a ‘mild to severe problem’ in the preceding 3 months (see Figure 2a) suggesting that although only 26% of participant had a pressure ulcer at the time of interview, many more had recent problems with pressure ulcers. Most participants had been out of bed in the week preceding their interviews and 244 (86%) had left their homes (Table 4). The median (IQR) WHODAS score for the participation items was 24/40 (20 to 26). The WHODAS scores were slightly lower for those who were wheelchair-dependent. More than half the participants indicated that their SCI had created ‘severe’ difficulties engaging in community activities (Figure 3).
SCI Secondary Conditions Scale results for (a) those who were wheelchair-dependent (n=168) and (b) those who were walking (n=115). The percentage of responses is on the x axis and each item of the SCI Secondary Conditions Scale on the y axis. Eleven participants declined to answer the question about sexual dysfunction and one declined to answer the question about respiratory compromise.
Participants had mean scores on the mental and physical components of the SF12 of between 32 (equivalent to the lowest 2% of the American population) and 43 points (equivalent to the lowest 34% of the American population; see Table 4). The question with the highest number of negative responses was ‘have you felt downhearted and blue?’. The median (IQR) CESDS score was 10/60 (8 to 14) where a low score indicates less depressive symptoms. However, 52 (32%) of participants who were wheelchair-dependent had scores of 16 or higher (versus 9% for participants who were walking). A score of 16 is typically used around the world to indicate sub-threshold depressive symptoms in the general population; however, some have suggested that for people with SCI, this should be raised to 19.20, 21 In addition, 21 (13%) of those who were wheelchair-dependent exhibited signs of a possible major depressive episode, 10 (6%) probable major depressive episode and 7 (4%) major depressive episode.
Discussion
This study provides descriptive data on a representative sample of survivors approximately 2.5 years after discharge from a tertiary SCI hospital in Bangladesh. The study cohort is clearly defined and there is a high rate of follow-up.
The results of the SCI Secondary Conditions Scale for this cohort are not dissimilar to those reported in high-income countries,3 however, there was a high rate of pressure ulcers in those who were wheelchair-dependent. These data align with the mortality data from our larger cohort, which indicated that 56% of the 55 deaths in the first 2.5 years following discharge were due to pressure ulcers.8 Pressure ulcers are clearly one of the biggest health risks for people with SCI in LMICs.22, 23 The participants in this cohort had all received comprehensive education about low cost strategies to prevent pressure ulcers during their inpatient rehabilitation. In addition, they had all been provided with cushions for their wheelchairs and advice on appropriate bed overlays. Regardless, there was still a high prevalence of pressure ulcers 2.5 years following discharge. This suggests that there are significant barriers preventing people with SCI in LMICs from adopting appropriate preventative strategies in the community.24 These may include limited finances and support, depression or the rural environment. If some of these barriers could be better identified, then attention could be directed at facilitating effective interventions.
Sexual dysfunction was cited as a ‘severe’ problem for 20% of participants who were wheelchair-dependent (n=33/161) and 4% of participants who were capable of walking (5/111; Figure 2). This issue requires further exploration because it is not clear whether participants were indicating sexual dysfunction or sexual dissatisfaction. Future versions of the SCI Secondary Conditions Scale need to clarify this distinction in the instructional text.13
The responses to the participation items of the WHODAS indicated limited community engagement and other areas of concern. For example, 70% of participants who were wheelchair-dependent indicated that their SCI had created ‘severe’ family problems (n=117/168) and a drain on their finances (n=125/168). Similarly, 64% indicated that they had ‘severe’ problems engaging in community activities (n=108/168) and some indicated that they could not engage in community activities at all (n=7/168; Figure 3). The situation was similar for those capable of walking although less pronounced with only 13% indicating that their SCI created ‘severe’ problems engaging in community activities (n=15/115) and none indicating that they could not engage in community activities at all. The out of bed and out of home questions were included to supplement the WHODAS because we had observed that many people with SCI who are wheelchair-dependent are bedbound and housebound. It was therefore encouraging to find that 95% of those who were wheelchair-dependent on discharge had been out of bed in the week preceding their interviews. However, one in five participants had not left their homes (Table 4) in the last week. These findings may reflect the difficulties mobilising in a wheelchair outside the bounds of the home in Bangladesh or they may reflect psychological distress. Psychological distress could reduce motivation to get out of the home. Alternatively, it may be that these participants had limited opportunities to engage in work and purposeful activities. Some participants may have been unable to leave their home because of pressure ulcers or other medical problems. Regardless of the explanation, the finding that large numbers of young adults with SCI are housebound and expressing ‘severe’ problems with their families, finances and engaging in the community is concerning.
Nearly 50% of all participants and 37% of those who were wheelchair-dependent were working after injury. Those unable to walk, with tetraplegia, and with CESDS scores greater than 15 were less likely to work than those able to walk, with paraplegia and with CESDS scores less than 16 (see Table 3). The median income per person living in the home of a person with SCI was just $US20 per month (Table 2) compared with $US26 per month prior to injury. These figures need to be interpreted in relation to the Gross Domestic Product per capita of $US80 per month for Bangladesh between 2010 and 201425 and the average poverty line in low income countries of $US60 per month (or $US2 per day).25 These findings support the widely held view that SCI in LMICs primarily affects those already living in poverty and throws families of those affected into even more severe poverty.20, 21 The reason why those with low incomes are more vulnerable to SCI in countries like Bangladesh reflects the leading causes of SCI in these countries, namely, falls related to manual labouring jobs such as picking mangoes and coconuts, and carrying heavy weights on the head.
There were signs of depression in those who were wheelchair-dependent although participants generally had lower rates of depression than those seen in people with diabetes18 or leprosy19 in Bangladesh. The SF12 data are more difficult to interpret because there are no normative data for Bangladesh and there are obvious difficulties normalising these data to the American population. It is, however, possible that those with SCI in Bangladesh fair better psychologically than those with SCI in high income countries despite the obvious challenges of living with SCI in countries like Bangladesh. This may be due to the close family structures in Bangladesh with all participants (except two) cared for by spouses and families and no participants institutionalised after discharge. There are many other societal differences between Bangladesh and high income countries that may have both positive and negative impacts on the implications of living with a SCI. Clearly, more work needs to be done to understand these issues.
It is not clear whether the results of this study can be generalised to people with SCI discharged from all hospitals in Bangladesh, or to people with SCI discharged from hospitals in other LMICs. Most people with SCI in Bangladesh and LMICs are discharged from hospitals into environments similar to those in which the patients from CRP were discharged, where there is little or no access to disability or health services. It is not known whether the quality of hospital care provided by a specialist SCI centre like CRP prepares patients for life in the community better than other hospitals, or whether the patients discharged from CRP are similar to patients discharged from other hospitals in LMICs.
The main limitation of this study is that most participants were interviewed by telephone. This creates two potential problems: it was difficult to ascertain that participants understood the questions, and participants’ responses could not be confirmed by direct observation or clinical examination. For example, questions about how often participants got out of bed and the home, or about the presence of pressure ulcers, may have been more accurately determined with a face-to-face assessment than by telephone self-report. In addition, participants may not have been willing to reveal their true psychological status over the telephone and we may have got different results if the questionnaires were administered in person. Another limitation of the study is that we were restricted to measures that were available in Bangla. These were not always the most widely used measures for people with SCI.
Many people with SCI in Bangladesh are house-bound, unemployed, living in poverty and have pressure ulcers. They experience moderate rates of depression and report limited QOL. These findings have prompted our group to set up a clinical trial (titled the CIVIC trial) which aims to determine the effectiveness of a low cost community-based model of care to support people with SCI in the community during the first 2 years following discharge from hospital in Bangladesh.26
Data archiving
There were no data to deposit.
References
Kennedy P, Lude P, Taylor N . Quality of life, social participation, appraisals and coping post spinal cord injury: a review of four community samples. Spinal Cord 2006; 44: 95–105.
van Koppenhagen CF, Post MW, van der Woude LH, de Witte LP, van Asbeck FW, de Groot S et al. Changes and determinants of life satisfaction after spinal cord injury: a cohort study in the Netherlands. Arch Phys Med Rehabil 2008; 89: 1733–1740.
Adriaansen JJ, Post MW, de Groot S, van Asbeck FW, Stolwijk-Swuste JM, Tepper M et al. Secondary health conditions in persons with spinal cord injury: a longitudinal study from one to five years post-discharge. J Rehabil Med 2013; 45: 1016–1022.
Kawu AA, Alimi FM, Gbadegesin AA, Salami AO, Olawepo A, Adebule TG et al. Complications and causes of death in spinal cord injury patients in Nigeria. West Afr J Med 2011; 30: 301–304.
Scovil CY, Ranabhat MK, Craighead IB, Wee J . Follow-up study of spinal cord injured patients after discharge from inpatient rehabilitation in Nepal in 2007. Spinal Cord 2012; 50: 232–237.
Chhabra HS, Arora M . Neglected traumatic spinal cord injuries: Causes, consequences and outcomes in an Indian setting. Spinal Cord 2013; 51: 238–244.
Singh R, Dhankar SS, Rohilla R . Quality of life of people with spinal cord injury in Northern India. Int J Rehabil Res 2008; 31: 247–251.
Hossain M, Rahman M, Herbert R, Quadir M, Bowden J, Harvey L . Two-year survival following discharge from hospital after spinal cord injury in Bangladesh. Spinal Cord e-pub ahead of print 16 June 2015 doi:2010.1038/sc.2015.2092.
Centre for Rehabilitation of the Paralysed. Annual Report: July 2009 to June 2012. 2010: CRP Printing Press, Bangladesh.
Centre for Rehabilitation of the Paralysed. Annual Report: 2012-2013, Ability not disability. 2010: CRP Printing Press, Bangladesh.
Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med 2011; 34: 535–546.
Kalpakjian CZ, Scelza WM, Forchheimer MB, Toussaint LL . Preliminary reliability and validity of a Spinal Cord Injury Secondary Conditions Scale. J Spinal Cord Med 2007; 30: 131–139.
Arora M, Harvey L, Lavrencic L, Bowden J, Nier L, Glinsky J et al. A telephone-based version of the Spinal Cord Injury Secondary Conditions Scale: A reliability and validity study. Spinal Cord (e-pub ahead of print 21 July 2015).
Wolf AC, Tate RL, Lannin NA, Middleton J, Lane-Brown A, Cameron ID . The World Health Organization Disability Assessment Scale, WHODAS II: reliability and validity in the measurement of activity and participation in a spinal cord injury population. J Rehabil Med 2012; 44: 747–755.
World Health Organisation. Measuring Health and Disability: Manual for WHO Disability Assessment Schedule (WHODAS 2.0). In: Üstün T et al (eds). Geneva, Switzerland. 2010.
Feroz AHM, Islam MN, Ten Klooster PM, Hasan M, Rasker JJ, Haq SA . The Bengali Short Form-36 was acceptable, reliable, and valid in patients with rheumatoid arthritis. J Clin Epidemiol 2012; 65: 1227–1235.
Ahmed SM, Rana AK, Chowdhury M, Bhuiya A . Measuring perceived health outcomes in non-western culture: Does SF-36 have a place? J Health Popul Nutr 2002; 20: 334–342.
Rahman M, Rahman MA, Flora MS, Karim R, Zaman MR . Depression and its association with socio-demographic characteristics among type 2 diabetes mellitus patients of Bangladesh. Mymensingh Med J 2012; 21: 490–496.
Tsutsumi A, Izutsu T, Islam MDA, Amed JU, Nakahara S, Takagi F et al. Depressive status of leprosy patients in Bangladesh: Association with self-perception of stigma. Lepr Rev 2004; 75: 57–66.
World Health Organization and The World Bank World Report on Disability. Geneva. 2011.
World Health Organization International Perspectives on Spinal Cord Injury. Geneva. 2013.
Zakrasek EC, Creasey G, Crew JD . Pressure ulcers in people with spinal cord injury in developing nations. Spinal Cord 2015; 53: 7–13.
Levy LF, Makarawo S, Madzivire D, Bhebhe E, Verbeek N, Parry O . Problems, struggles and some success with spinal cord injury in Zimbabwe. Spinal Cord 1998; 36: 213–218.
European Pressure Ulcer Advisory Panel and National Pressure Ulcer Advisory Panel. Prevention and Treatment of Pressure Ulcers: Quick Reference Guide. Washington DC, 2009.
http://data.worldbank.org/indicator/NY.GDP.PCAP.CD The World Bank. Accessed on 24th March 2015.
The Australian and New Zealand Clinical Trial Registry. ACTRN12615000630516: The CIVIC TRIAL: a randomised trial of a community-based intervention to prevent serious complications following spinal cord injury in Bangladesh. Accessed www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=368756.
Acknowledgements
We thank the staff and patients of the Centre for the Rehabilitation of the Paralysed for their assistance in collecting these data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
MSH, MAR and MMQ are employed by the Centre for the Rehabilitation of the Paralysed and received salary support to conduct the submitted work. Readers may perceive that they have an interest in portraying good outcomes following admission and discharge from this centre. The funders (The University of Sydney) had no influence or role in the collection, analysis or interpretation of the data; in writing the report; or in the decision to submit the article for publication. The researchers worked independently from the funders.
Rights and permissions
About this article
Cite this article
Hossain, M., Rahman, M., Bowden, J. et al. Psychological and socioeconomic status, complications and quality of life in people with spinal cord injuries after discharge from hospital in Bangladesh: a cohort study. Spinal Cord 54, 483–489 (2016). https://doi.org/10.1038/sc.2015.179
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2015.179
This article is cited by
-
An assessment of disability and quality of life in people with spinal cord injury upon discharge from a Bangladesh rehabilitation unit
Spinal Cord (2023)
-
Ethical issues and dilemmas in spinal cord injury rehabilitation in the developing world: a mixed-method study
Spinal Cord (2022)
-
Considerations on the psychometric properties and validity of the Spinal Cord Injury Secondary Conditons Scale
Spinal Cord (2021)
-
Understanding how a community-based intervention for people with spinal cord injury in Bangladesh was delivered as part of a randomised controlled trial: a process evaluation
Spinal Cord (2020)
-
Loss of work-related income impoverishes people with SCI and their families in Bangladesh
Spinal Cord (2020)