Abstract
Study design:
Retrospective observational study.
Objectives:
The objective of this study was to determine the rehabilitation potential and the extent to which it is realized in a cohort of spinal cord injury patients using the Spinal Cord Injury-Ability Realization Measurement Index (SCI-ARMI) and to study the clinical factors that influence this realization.
Setting:
Two spinal units in Italy.
Methods:
Consecutive patients were assessed at the end of an in-patient rehabilitation program using the Spinal Cord Independence Measure and the International Standards for Neurological Classification of Spinal Cord Injury. On the basis of these data and of the age and gender of the patients, we calculated the SCI-ARMI score. Regression analyses were performed to study the relationship between clinical factors and the extent to which rehabilitation potential is realized.
Results:
We examined the data for 306 patients. Most patients were discharged without having reached their rehabilitation potential, with an SCI-ARMI score <80%. SCI-ARMI scores at discharge were positively influenced by etiology and the lesion level and correlated negatively with lesion severity and the presence of complications during rehabilitation.
Conclusion:
The SCI-ARMI is an effective tool that can be used to measure the achievement of rehabilitation potential in SCI patients and to identify groups of patients who are at risk of not meeting their rehabilitative potential.
Similar content being viewed by others
Introduction
The Spinal Cord Injury-Ability Realization Measurement Index (SCI-ARMI) is a tool that is based on the Spinal Cord Independence Measure (SCIM), which evaluates the success of rehabilitation and the rehabilitation potential of spinal cord injury (SCI) patients after controlling for their clinical (motor scores) and demographic (gender and age) factors.1, 2
Ability realization is defined as the ratio of the observed and maximum possible performance of daily activities, for any level of severity of an SCI. The SCI-ARMI score is ability realization, expressed as a percentage. The difference between an SCI-ARMI score of 100 (representing 100% ability realization) and the score before rehabilitation reflects the rehabilitation potential when the neurological deficit is stable. The change in the ability realization during rehabilitation is primarily considered to indicate the effect of rehabilitation.
The SCI-ARMI instrument was introduced in 2004.1 Since then, several versions of this tool have been developed. A newly published version is based on SCIM III3 and incorporates clinical (motor scores of the International Standards for Neurological Classification of Spinal Cord Injury) and demographic factors (age and gender).4
In developing the SCI-ARMI, the 95th percentile of SCIM III values at discharge from rehabilitation (SCIM95) was used to provide a conservative estimate of the maximum possible performance of daily activities for each AMS value. A quadratic formula, based on the data of 661 SCI patients from 6 countries, generated the best estimation of the SCIM95.4 The original quadratic model for the SCIM95, which was a function of AMS alone, was extended by adding age at admission to rehabilitation and gender as factors. These additions had statistically significant effects on the SCIM95 (P>0.03), and there were no interactions with AMS or between age and gender. Adding country of residence to the model had no further statistically significant effects on SCIM95. The latest version of the SCI-ARMI (Figure 1) is obtained by dividing the individual’s SCIM III score by the calculated SCIM95 score, expressed as a percentage. The formula produces similar values between countries.
The aim of this study was to apply the newest version of the SCI-ARMI to a group of patients to evaluate the extent of their ability realization and examine the clinical factors that influence the realization of their rehabilitation potential.
Patients and methods
We retrospectively examined the data for consecutive patients who were hospitalized at two specialized Italian centers between 1 January 2007 and 31 December 2013 for their first rehabilitation after SCI. The exclusion criteria were patients who showed neurological deterioration. Whenever a patient was discharged or transferred for more than 3 weeks, the readmission was considered a second admission, and the patient was excluded.
For each patient, we recorded the following data:
-
– Age.
-
– Gender.
-
– Total hospitalization duration (acute+rehabilitation stay).
-
– Etiology of the lesion (traumatic or nontraumatic).
-
– Associated lesions (traumatic brain injury, nonvertebral fractures that required surgery, severe facial injuries that affected the sense organs, major chest injury that required a chest tube or mechanical ventilation, severe hemorrhaging or damage to any internal organ that required surgery)5 were categorized (only for patients with traumatic lesions) as present or absent.
-
– Medical complications (pressure sores, deep vein thrombosis, pulmonary embolism, heterotopic ossifications, urological complications, pain, spasticity and depression) on admission to rehabilitation and during the rehabilitation stay were recorded as present or absent.6
-
– Major surgical interventions.
At admission and discharge, neurological status was evaluated as per the International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) with regard to motor scores, neurological level and American Spinal Injury Association (ASIA) Impairment Scale (AIS) scores.7
Functional status at admission and discharge was evaluated using SCIM III.3
On the basis of these data, we calculated the SCI-ARMI score, which is the percentage of rehabilitation potential that is met by the patients (Figure 1).
Statistical analysis
Descriptive values, expressed as mean±s.d. (median and range), were supplied for all continuous clinical data, whereas frequencies and percentages were reported for categorical data.
Regression analyses were performed to test the influence of independent variables on SCI-ARMI. We considered the SCI-ARMI at discharge as a continuous outcome and seven selected independent variables as predictors. Explanatory variables were categorical (ASIA and lesion level), dichotomous (etiology, surgical treatment, complications at admission, complications during hospitalization) or continuous (length of stay in the hospital).
Univariate regression models were run, and significant predictors were then included in the multivariate estimation. The multivariate model was estimated by stepwise regression, including one variable at a time and testing the significance of the predictors stepwise. We calculated F-test P-values to determine the significance of the association between the predictors and the outcome, the relative proportion of the explained variability and the coefficients of all significant explanatory variables and their 95% confidence intervals (95% CIs). Predictors were considered to be significant at an α level of 0.05.
The association between predictors was then analyzed to avoid multicollinearity. The Wilcoxon Mann–Whitney test and the Kruskal–Wallis test were used for continuous predictors, and Pearson’s χ2 test was used for categorical variables.
In a subset of 225 patients, specific complications were included in the multivariate regression model to identify those that influenced SCI-ARMI scores at discharge.
Results
The study sample comprised 319 subjects, but 13 cases with missing data were omitted from the database. Thus, we examined the data on 306 patients. There were 230 males and 76 females, and the mean age was 47.8±17.7 (median 48, range (15; 86)) years; the mean duration from lesion onset to discharge from rehabilitation was 5.2±3.4 (4.7 (0.5; 17.4)) months. There were 114 patients with a cervical lesion, 141 with a thoracic lesion and 51 with lumbar lesions. AIS grade at admission was A in 102, B in 36, C in 56 and D in 112 patients. With regard to etiology, 172 patients had a traumatic lesion, and 134 had a nontraumatic lesion. Associated lesions were recorded only in patients with traumatic lesions. Of 172 patients, 105 (61%) had one or more associated lesions. Complications were present in 117 patients at admission and developed in 113 patients during the rehabilitation stay; 221 patients underwent surgical treatment (Table 1).
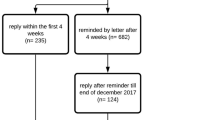
The mean SCI-ARMI percentage at discharge was 73.0±21.3% (median 78.6%, range (14.3; 119.2)); <50% of patients were discharged with an SCI-ARMI score that exceeded 80% (Figure 2).
By univariate regression analysis, there was a strong effect of nearly all variables; surgical treatment was at the limit of significance, and associated lesions did not affect the outcome (Table 2). Thus, all significant variables were entered into the multivariate analysis. The resulting model produced accounted for 20% of the variability in SCI-ARMI scores at discharge. SCI-ARMI scores at discharge were not influenced by the presence of complications at admission, the length of stay in the rehabilitation center or having undergone surgical intervention (Table 3). SCI-ARMI scores increased with traumatic etiology (+14 points) and in patients with thoracic and lumbar versus cervical lesions (thoracic +5 points, lumbar +12 points); however, they were negatively influenced by the presence of complications during rehabilitation (~−10 points) and AIS grades A, B and C compared with AIS D (AIS A −7 points, B and C −13 points) (Table 3).
Because complications at admission and length of stay lost their significance on entering the multivariate model, we examined their association with the other predictors (Table 4). Length of stay correlated with all other variables—higher in patients with AIS grades A, B and C versus grade D; traumatic etiology; complications at admission and during rehabilitation; cervical and thoracic versus lumbar lesions; and surgical intervention. Moreover, in constructing a multivariate model with LOS as the outcome and the other variables as predictors, the set of predictors explained the variability in LOS better than SCI-ARMI (R2=0.3427). This result justified the removal of LOS from the set of predictors to avoid multicollinearity. Complications at admission were more frequent in patients with complications during rehabilitation and those who underwent surgical treatment and were significantly less common in those with AIS grade D compared with A, B and C and those with lumbar-level lesions. Even in this case, the removal of complications at admission from the set of predictors was justified, based on their robust correlation with the other variables (Table 4).
Using the data on a subsample of 225 patients, we constructed a multivariate regression model that included the type of complication at admission and during rehabilitation to analyze which category influenced SCI-ARMI scores at discharge. None of the complications at admission significantly affected the outcome, whereas respiratory, urological and ‘other’ complications (including pain, spasticity, depression and surgical emergencies) during rehabilitation negatively influenced the rehabilitation potential. In particular, respiratory complications reduced SCI-ARMI scores by ~16%, compared with roughly 13% for urological complications and about 10% for ‘other’ complications (Table 5).
Discussion
The ability to estimate the likelihood of success before rehabilitation and to measure success after rehabilitation is required to answer patients’ questions regarding their functional status at discharge, plan efficient allocation of available resources for rehabilitation and predict the resources that will be needed after discharge. Such ability also allows one to determine the efficacy of the care during rehabilitation and modify the treatment to improve outcomes in overall function or on specific tasks.8
Predicting the rehabilitation potential of SCI subjects
Several disability rating scales (Modified Barthel Index, Functional Independence Measure and Spinal Cord Independence Measure) have been proposed and used to evaluate SCI patients on admission and during the course of rehabilitation, assess treatment efficacies and weigh the burden of care.9, 10, 11 However, these instruments are unable to assess the disability weighted for the neurological deficit and thus evaluate the independent value of rehabilitation in improving function beyond the effects of neurological recovery, despite its wide acceptance.12, 13, 14 For SCI patients with complete lesions, in whom the likelihood of significant neurological recovery is low or absent, the difference between functional status at admission and discharge is likely to reflect the effectiveness of rehabilitation solely, but for those with incomplete SCI, who might experience natural neurological recovery, the differences in disability scores do not represent the net effect of the treatment.2
To overcome this problem, the SCI-ARMI, based on the Spinal Cord Independence Measure, was developed in the Spinal Department of Loewenstein Rehabilitation Hospital, Israel, and first published in 20041 to detect changes in functional performance that are independent of neurological changes, constituting a new approach to quantitating the prospect and success of rehabilitation. The initial version of the SCI-ARMI merely took into account the relationship between SCIM and AIS motor scores.1
A newer version of the instrument that incorporates the effects of age and gender was developed and validated in a multicenter international study,4 in which the authors chose discharge values, based on the presumption that at discharge from rehabilitation, ability realization was the highest score that was attainable. Nevertheless, they acknowledged that function might be further enhanced after discharge in certain individuals, necessitating a dedicated study. They also affirmed that the formula could be modified to incorporate new clinical variables with regard to their influence in achieving functional potential.4
Thus, the aims of our retrospective study were to apply the new formula to the data on SCI patients from two SCI centers in Italy to determine whether they were discharged, having achieved their entire rehabilitation potential and study the relationship between SCI-ARMI scores at discharge and clinical variables that, based on previous studies and our clinical experience, could influence functional outcomes in SCI patients.
Goals after rehabilitation
With regard to this issue, our data indicate that most patients were discharged without having achieved their full rehabilitation potential. Independent of the possible reasons below, we have demonstrated the value of the SCI-ARMI in assessing patients with SCI. It might be particularly useful to highlight groups of patients who are at greater risk of failing to achieve their rehabilitative potential and establish different and more appropriate rehabilitative paths for this subset before and after discharge.
The inability to achieve complete functional potential in most of our patients might be attributed to our organizational infrastructure. Because of the scarcity of dedicated beds for SCI patients and continuous pressure by the National Health Service to shorten rehabilitation stays for such subjects, it is possible that patients are discharged as soon as they reach a certain level of independence and routed to alternate levels of care. Although the possibility that patients are released as soon as they are dischargeable has been demonstrated,15 we have merely inferred such patterns, based on our clinical experience, necessitating a dedicated prospective study, possibly involving centers with various health-care systems and disparate reimbursement systems.
Factors that might influence the realization of rehabilitation potential
With regard to the factors that might influence SCI-ARMI values at discharge, we performed regression analysis and examined several clinical factors, including etiology, level and severity of the lesion, the presence of associated lesions (in patients with traumatic SCI), the presence of complications at admission and during rehabilitation and a history of surgery for the spinal cord lesion.
In this study, etiology of the lesion had a strong effect on the realization of rehabilitation potential, with traumatic SCI having a positive effect on SCI-ARMI scores in the univariate and multivariate regression analyses. The influence of etiology on outcomes in SCI patients has been examined in several articles15, 16, 17, 18 but remains debated. Certain authors have found that patients with traumatic SCIs have better outcomes than their nontraumatic counterparts but failed to provide any explanations for this finding.16 Other groups reported comparable levels of independence between the two etiologies.15, 17, 18 In all these works, the authors agree that the two cohorts have disparate clinical and demographic profiles (in particular, age and neurological features), attributing the eventual differences in outcome between groups to these features. However, in our study, age and neurological status were already included in the SCI-ARMI; thus, they do not explain the effect of etiology on SCI-ARMI scores, which remains to be determined.
Level (lower lesions) and completeness (less severe) of the lesion had a positive effect on SCI-ARMI scores. Patients with less severe lesions and lower lesions have less independence to achieve and recover faster and thus have a greater chance of achieving their rehabilitation potential during an in-patient rehabilitation stay, which, although it is longer than in other countries, is limited. One can argue that it is incorrect to add lesion level and severity to the analysis, because elements of the neurological examination (motor scores) already exist in the formula. However, we decided to add these data, based on previous studies that have demonstrated the importance of total motor scores and their distribution.19, 20 Equivalent motor scores have different meanings in a tetraplegic or a paraplegic patient with regard to AIS impairment and functional status.
The lack of an effect of the associated lesions on the outcomes of traumatic SCI patients is well established and thus expected. Associated lesions might affect the level of independence of SCI patients at admission5 and likely the length of rehabilitation stay, although insignificantly in most cases.5, 21 However, the outcome at discharge is usually not influenced, and patients with traumatic SCIs, with or without associated traumas, achieve the same level of independence for similar lesion severities.
The negative effect of complications during rehabilitation on SCI-ARMI scores is the most significant finding of this study and highlights the value of the formula in identifying groups of patients who are at risk of poorer rehabilitation outcomes. There are a few studies on the impact of complications on SCI patient outcomes that have focused primarily on the impact of pressure sores22, 23 and reported that patients with pressure sores have worse Functional Independence Measure scores at discharge and longer LOSs than patients without pressure sores.
In contrast, in our series, pressure sores did not have an impact on SCI-ARMI scores at discharge, although they were the most frequent complication. Our only explication for this discrepancy is that we included all types of pressure sores, without grading their severity. Low-severity pressure sores (which are likely the predominant complications) might not affect patient outcomes.
There were no data on respiratory, urological and ‘other’ complications in the literature, and we cannot offer any explanation for their influence on ability realization. Thus, this issue requires a dedicated study before complications during rehabilitation are included in the next iteration of the SCI-ARMI formula. These data are an example of the value of the SCI-ARMI in evaluating the quality of rehabilitation and identifying patients who are at risk. Good rehabilitation is supposed to prevent and treat complications to elicit optimal outcomes. The effects of complications on SCI-ARMI can be considered part of the effects of rehabilitation. It is possible that, in a subset of our patients, rehabilitation was suboptimal, and, functional outcomes might have been lower, in part through the appearance or recurrence of complications.
Limitations
This work has several limitations. The regression model accounts for only 20% of the variability of in-ARMI scores, likely because the main factor that affects SCI-ARMI, besides AMS, age and gender, is the efficacy of rehabilitation. However, this datum might also indicate effects of other variables on SCI-ARMI that were not considered in this study. For example, the sensory scores of patients were not considered, because they were missing or not completely reliable. Associated lesions and complications were recorded dichotomously as present or absent. However, as discussed, the severity of these factors and their impact on rehabilitation can vary. Thus, they deserve a separate ad hoc analysis. Further, certain aspects of SCI (clinical aspects or complications), such as pain, spasticity and depression, were considered as complications only if they were very severe, whereas their severity could have been graded and better correlated to functional potential realization.
It would be interesting to determine the SCIM III items that were less achieved and the ADLs for which more rehabilitation time might be essential. Unfortunately, because of the retrospective nature of the study, we do not have the values of single activities.
We had no means to weigh the impact of bureaucratic or organization-dependent decisions. Researchers from both centers acknowledge that some patients are discharged without having reached their rehabilitation potential, necessitating a longer follow-up to determine whether SCI-ARMI scores continue to increase while the patients are at home. Further, it is possible that, after discharge, the rise in SCI-ARMI scores could accelerate, because some patients might find it easier to develop new strategies and coping solutions while living in real-life situations.
Conclusions
The SCI-ARMI is an effective tool that monitors the development and achievement of rehabilitation potential in SCI patients and identifies groups of patients who are at risk of failing to meet their rehabilitative potential. According to our data, the etiology, level and severity of the lesion and the presence of complications affect the development of rehabilitation potential. Thus, these factors must be taken into account in future versions of the SCI-ARMI.
Data archiving
There were no data to deposit.
References
Catz A, Greenberg E, Itzkovich M, Bluvshtein V, Ronen J, Gelernter I . A new instrument for outcome assessment in rehabilitation medicine: Spinal Cord Injury Ability Realisation Measurement Index (SCI-ARMI). Arch Phys Med Rehabil 2004; 85: 399–404.
Aidinoff E, Benjamini Y, Galili T, Polliack T, Front L, Bluvshtein V et al. Non-linear formulas for the spinal cord injury ability realisation measurement index (SCI-ARMI). Spinal Cord 2012; 50: 324–327.
Catz A, Itzkovich M, Tesio L, Biering-Sorensen F, Weeks C, Laramee MT et al. A multi-center international study on the Spinal Cord Independence Measure, version III: Rasch psychometric validation. Spinal Cord 2007; 45: 275–291.
Scivoletto G, Glass C, Anderson KD, Galili T, Benjamin Y, Front L et al. An international age and gender controlled model for the spinal cord injury ability realization measurement index (SCI-ARMI). Neurorehabil Neural Rep 2015; 29: 25–32.
Scivoletto G, Farchi S, Laurenza L, Tamburella F, Molinari M . Impact of polytrauma on functional and neurological outcomes of patients with spinal cord injury. Scand J Trauma Resus Emerg Med 2013; 21: 42.
Pagliacci MC, Celani MG, Zampolini M, Spizzichino L, Franceschini M, Baratta S et al. Gruppo Italiano Studio Epidemiologico Mielolesioni: Spinal cord lesion management in Italy: a 2-year survey. Spinal Cord 2003; 41: 620–628.
American Spinal Injury Association. International Standards for Neurological Classifications of Spinal Cord Injury (Revised). American Spinal Injury Association: Chicago, IL, USA,. 2000, pp 1–23.
Wilson JR, Grossman RG, Frankowski RF, Kiss A, Davis AM, Kulkarni AV et al. Clinical Prediction Model for long-term functional outcome after traumatic spinal cord injury based on acute clinical and imaging factors. J Neurotrauma 2012; 29: 2263–2271.
Roth E, Davidoff G, Haughton J, Ardner M . Functional assessment in spinal cord injury: a comparison of the Modified Barthel Index and the 'adapted' Functional Independence Measure. Clin Rehabil 1990; 4: 277–285.
Grey N, Kennedy P . The Functional Independence Measure: a comparative study of clinician and self ratings. Paraplegia 1993; 31: 457–461.
McDowell I, Newell C . Measuring Health: A Guide to Rating Scales and Questionnaires. Oxford University Press: New York, NY, USA,. 1996, pp 47–121.
Guttmann L . Spinal Cord Injuries, Comprehensive Management and Research. Blackwell Scientific: Oxford, UK,. 1973, pp 639–645.
Burns AS, Ditunno JF . Establishing and maximizing functional outcomes after spinal cord injury: a review of current and future directions in rehabilitation management. Spine 2001; 26: S137–S145.
Roth EJ, Heinemann AW, Lovell LL, Harvey RL, McGuire JR, Diaz S . Impairment and disability: their relation during stroke rehabilitation. Arch Phys Med Rehabil 1998; 79: 329–335.
Scivoletto G, Farchi S, Laurenza L, Molinari M . Traumatic and non-traumatic spinal cord lesions: an Italian comparison of neurological and functional outcomes. Spinal Cord 2011; 49: 391–396.
McKinley WO, Seel RT, Gadi RK, Tewksbury MA . Nontraumatic vs. traumatic spinal cord injury: a rehabilitation outcome comparison. Am J Phys Med Rehab 2001; 80: 693–699.
Ones K, Yilmaz E, Beydogan A, Gultekin O, Caglar N . Comparison of functional results in non-traumatic and traumatic spinal cord injury. Disabil Rehabil 2007; 29: 1185–1191.
Gupta A, Taly AB, Srivastava A, Vishal S, Murali T . Traumatic vs non-traumatic spinal cord lesions: comparison of neurological and functional outcome after inpatient rehabilitation. Spinal Cord 2008; 46: 482–487.
Steeves JD, Kramer JK, Fawcett JW, Cragg J, Lammertse DP, Blight AR et alEMSCI Study Group. Extent of spontaneous motor recovery after traumatic cervical sensorimotor complete spinal cord injury. Spinal Cord 2011; 49: 257–265.
Kramer JL, Lammertse DP, Schubert M, Curt A, Steeves JD . Relationship between motor recovery and independence after sensorimotor-complete cervical spinal cord injury. Neurorehabil Neural Rep 2012; 26: 1064–1071.
Putz C, Schuld C, Gantz S, Grieser T, Akbar M, Moradi B et al. The effect of polytrauma as a possible confounder in the outcome of monotraumatic vs polytraumatic paraplegic patients: a clinical cohort study. Spinal Cord 2011; 49: 721–727.
Wang H, Niewczyk P, Divita M, Camicia M, Appelman J, Mix J et al. Impact of pressure ulcers on outcomes in inpatient rehabilitation facilities. Am J Phys Med Rehabil 2014; 93: 207–216.
New PW, Rawicki HB, Bailey MJ . Nontraumatic spinal cord injury rehabilitation: pressure ulcer patterns, prediction, and impact. Arch Phys Med Rehabil. 2004; 85: 87–93.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Scivoletto, G., Bonavita, J., Torre, M. et al. Observational study of the effectiveness of spinal cord injury rehabilitation using the Spinal Cord Injury-Ability Realization Measurement Index. Spinal Cord 54, 467–472 (2016). https://doi.org/10.1038/sc.2015.153
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2015.153