Abstract
Objectives:
Acute spinal cord ischemia syndrome (ASCIS) due to coronary invasive intervention is rarely seen. In this case report we wish to highlight the mortality and morbidity of this entity.
Methods:
Case report.
Results:
A 60-year-old woman, diagnosed with acute myocardial infarction, presented with paresthesia and paraparesis of her legs after coronary invasive intervention. Magnetic resonance imaging showed hyperintensity from T6 to T10 consistent with ASCIS. Despite immediately starting rehabilitation program the patient never regained ambulation.
Conclusion:
Spinal cord infarction secondary to coronary intervention is rare, but when it presents the mortality and morbidity are high.
Similar content being viewed by others
Introduction
Acute spinal cord ischemia is a rare but mortal disease. The frequency of acute spinal cord ischemia syndrome was 1.2% of all stroke admissions to a community hospital during a 52-month period.1 Aortic pathologies, atherosclerosis, degenerative spine diseases, cardiac source of embolus, systemic hypotension and epidural anesthesia are etiological factors.2 There are only a few case reports about acute spinal cord ischemia as a complication of percutaneous coronary intervention in the literature.3, 4 Despite various clinical presentations, it usually presents as an acute intense back pain followed by paresthesia, progressive weakness of legs, paraparesis and loss of sphincter control. Magnetic resonance imaging (MRI) of the spine is the diagnostic tool.
Case report
A 60-year-old woman presented with chest pain that started with increasing intensity 2 h before she was admitted to our emergency department. The patient has diabetes mellitus, hypertension and hypercholesterolemia. The patient is a heavy cigarette smoker with a smoking history of 40 pack-years. The electrocardiogram showed no ischemic change, while cardiac injury marker troponin I was found to be 8, 89 pg ml−1. Owing to persistent chest pain, the patient was referred to the catheterization laboratory. At coronary angiography, the right coronary artery was found to be obstructed 90% in the proximal segment. The lesion was successfully treated with a stent implant and the patient was transferred to the coronary intensive care unit. After intervention, the chest pain subsided but the patient started to complain about an acute, intense lumbar pain, paresthesia and weakness of the lower extremities.
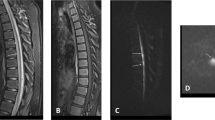
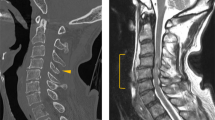
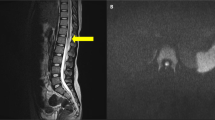
Apart from lost ability of sensation and moving of the lower extremities, the physical examination revealed no abnormal vital findings. The heart rate was 86 beats min−1, blood pressure 130/79 mm Hg, artery oxygen saturation 96%, body temperature 36.7 °C and peripheral pulses normal. A cranium computerized tomography did not show any bleeding or ischemia. On neurological examination, the patient’s mental functions were normal, and so were upper extremity reflexes and muscle strength. Deep tendon reflexes were absent, and muscle strength was bilaterally 0/5 in all key muscles of the lower extremities by manual muscle testing. While light touch and pin prick sensation was absent below T5, vibration and positional senses were preserved. Owing to neurological findings, the patient was thought to have an ASCİS caused by the intervention. MRI had already detected hyperintensity in T2 W imaging from T6 to T10 in sagittal (Figure 1) and transversal (Figure 2) views and focal cord enlargement from T6 to T10 with associated hypointensity in the same level of cord on sagittal T1W images (Figure 3), which indicate a spinal cord infarction at the thoracic segment.
Discussion
The upper spinal cord is supplied by two posterior spinal arteries and one anterior spinal artery, which arise from vertebral arteries. The lower spinal cord is supplied by radicular branches of intercostal and lumber arteries. The major anterior radicular artery originating from any level between T5 and L2 is named the Adamkiewicz artery.5 Our patient’s MRI images showed infarction of the spine from T6 to T10, which corresponds to the supply region of the Adamkiewicz artery. Therefore, an embolus of the Adamkiewicz artery during the cardiac intervention through aorta is the most likely cause.
Autonomic dysfunction, the loss of ability of sensation, motor deficit and areflexia are the main neurological findings of anterior spinal cord syndrome. Neurological examination of our case revealed normal mental functions, normal upper extremity reflexes and muscle strength, while deep tendon reflexes and motor functions were absent in the lower extremities. Light touch and pin prick sensation is absent at level T6, and the lower, vibrational and positional senses were preserved. As a consequence of neurological examination findings the patient was thought to have an acute anterior spinal cord ischemia syndrome due to the intervention. The level of neurological findings suggests strongly ischemia of the anterior spinal cord below T5 and embolus of the Adamkiewicz artery was confirmed. MRI helped us to make correct diagnosis by showing a hyperintensity of between T6 to T10 on T2W images and a bulky cord and hypointensity on T1W images.
The rehabilitation program started immediately and the patient was transferred to the physiotherapy and rehabilitation unit of another hospital. The patient was followed for 3 months in hospital under the surveillance of cardiology, psychiatry, neurology and physiotherapy. Unfortunately, the patient never regained ambulation.
Conclusion
Acute spinal cord ischemia syndrome secondary to vascular invasive intervention, especially coronary intervention, is a very rare complication. If spinal cord injury occurs despite all the security measurements being protective, it is crucial to work as a team and start early rehabilitation.
Limitations
We would like to thank reviewer 2 for his/her attention to the CT angiogram for the Adamkiewicz artery, which is crucial for diagnosis. In our case a control CT angiogram for Adamkiewicz artery was not done because the possible harm of contrast to the kidney and radiation (the patient was exposed to the radiation four times and to the contrast two times). This could be a limitation of our case report.
References
Sandson TA, Friedman JH . Spinal cord infarction: report of 8 cases and review of the literature. Medicine (Baltimore) 1989; 68: 282–292.
Nedeltchev K, Loher TJ, Stepper F, Arnold M, Schroth G, Mattle HP et al. Long-term outcome of acute spinal cord ischemia syndrome. Stroke 2004; 35: 560–565.
Blankenship JC, Mickel S . Spinal cord infarction resulting from cardiac catheterization. Am J Med 1989; 87: 239–240.
Vatankulu MA, Kayrak M, Alihanoglu Y, Salli A, Ulgen MS . A rare but serious complication of percutaneous coronary intervention: spinal cord embolism. J Spinal Cord Med. 2010; 33: 85–89.
Cheshire WP, Santos CC, Massey EW, Howard JF Jr . Spinal cord infarction: etiology and outcome. Neurology 1996; 47: 321–330.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kaya, A., Yıldız, Z. & Nurkalem, Z. Spinal cord infarction as a complication of percutaneous coronary intervention. Spinal Cord 52 (Suppl 2), S5–S7 (2014). https://doi.org/10.1038/sc.2014.80
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2014.80