Abstract
Study design:
We came across two patients with holocord tuberculosis exhibiting similar radiological picture, which may aid in early diagnosis.
Objectives:
We have described a new radiological sign for early diagnosis of intramedullary tubercular abscess.
Setting:
Observations from an endemic zone for tuberculosis (India).
Methods:
Surgical excision followed by histological and microbiological examination and retrospective correlation of clinical–radiological–surgical and pathological picture.
Results:
‘Precipitation sign’ can be helpful in the diagnosis of intramedullary tuberculosis.
Conclusion:
Presence of an intradural extramedullary mass at the lower end of the spinal cord associated with holocord T2 hyperintensities of the spinal cord can be called as precipitation sign and should raise the suspicion of intramedullary tubercular abscess.
Similar content being viewed by others
Introduction
Intramedullary tubercular abscesses have nonspecific clinicoradiological features and are relatively rare, and quite often there is a considerable delay in diagnosis that results in poor outcome.1, 2 Within a period of 1 year, we have come across two patients with holocord intramedullary tubercular abscesses mimicking transverse myelitis. Case 1 was reported by us earlier.1 Retrospectively, we identified a radiological sign called ‘precipitation sign’ that can help in diagnosing intramedullary tubercular abscess.
Case 1
A 33–year-old man presented with fever, rapidly progressive weakness of lower limbs and urinary retention for 5 days with sensory level at D4 suggestive of acute transverse myelitis. Magnetic resonance imaging (MRI) of dorsolumbar spine revealed widening of the spinal cord with T1 hypointensities and T2 hyperintensities extending from D2 to conus with patchy enhancement on contrast. There was a well-defined intradural extramedullary mass at the conus hypointense on T1 and iso to hypointense on T2-weighted images without contrast enhancement. Diagnostic lumbar puncture revealed preponderance of neutrophils with decreased sugars and elevated proteins. We proceeded for surgery with the aim of histological diagnosis and found yellowish, cheesy, fluffy material loosely attached to conus that was sent for bacterial, fungal, AFB stains, and culture and sensitivity. Preliminary cultures did not yield any organism. We started empirical intravenous antibiotics but weakness extended to upper limbs. Repeat MRI showed rostral extension of abscess to cervical cord. Surgical exploration revealed similar findings in the cervical cord. After 6 weeks, the sample had grown Mycobacterium tuberculosis and was started on anti-tubercular therapy (ATT). Patient did not improve at 6 months follow-up.
Case 2
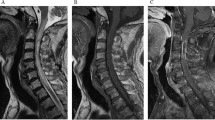
A 40-year-old, immunocompetent female patient presented with progressive paresthesia of lower limbs for 4 days. It was interpreted as L4/L5 prolapsed disc (Figure 1a), and L4/L5 discectomy was done by the attending surgeon. Following surgery, her symptoms continued to worsen and she deteriorated over 4 weeks with paraparesis and complete loss of sensations below groin. A repeat MRI revealed enlargement and hyperintensity of cord from D8-L1 on T2-weighted images (Figure 1b). A diagnostic lumbar puncture revealed lymphocytic pleocytosis and elevated protein levels. Empirical ATT was started but she continued to worsen and presented to us with paraplegia and sensory level at the level of nipples. Repeat MRI revealed holocord involvement (Figure 1c). There was a well-defined intradural extramedullary mass at conus (Figure 1d) that was hypointense on T1 and iso to hypointense on T2-weighted images without contrast enhancement. We operated the patient by L1-L2 laminectomy with the aim of histological diagnosis. A creamy, fluffy, avascular, organized material loosely attached to the conus was noted. With each Valsalva maneuver, the fluffy material was coming out from the lower end of the central canal. Histopathological examination of the specimen revealed granulomatous inflammation. Mycobacterial cultures showed growth of M. tuberculosis at 6 weeks with resistance to all primary anti-tubercular drugs. She was started on a newer ATT; however, the patient did not show any improvement after 6 months.
Imageological progression in case 2. (a) MRI of lumbo sacral spine shows no evidence of significant abnormality; (b) repeat MRI indicated by clinical worsening revealed cord enlargement (arrow) with hyperintensities involving the D8-10 level; (c) repeat MRI T2-weighted image revealed holocord hyperintensities (arrow); (d) at the lower end of cord there is a iso intense mass (arrow) probably due to precipittation of pus along the central canal.
Discussion
Intramedullary tuberculosis present acutely or subacutely with progressive neurological deficits. Tuberculosis should be differentiated from tumors, nonneoplastic lesions. MRI is the investigation of choice; however, radiological features are nonspecific. Tubercular abscesses are described as ring-enhancing lesions in the brain parenchyma but the enhancement may be absent or can be minimal in the spinal cord.1, 2 Hyperintensity on T2-weighted images spanning vertically over few segments with minimal, patchy enhancement on contrast images can mimic demyelinating or inflammatory disorders.2, 3 Demyelination is more common in the developed countries, whereas infections such as tuberculosis are more common in the tropical countries.3
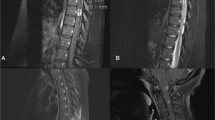
Both our patients had rapidly progressive weakness of limbs with extensive T2 hyperintensities of the whole spinal cord (Figure 2a). MRI in both the patients showed a well-defined intradural mass at conus that was hypointense on T1, iso to hypointense on T2-weighted images (Figures 2b and c) and was not enhancing on contrast. There are a number of case reports written about tuberculosis mimicking conus tumors although these all appear to be intramedullary collections within the conus, whereas our patients had extramedullary, intradural hypointense collection that pooled below the tip of the conus.4, 5, 6 We initially hypothesized that this was a collection of fluffy tubercular pus that has precipitated along the central canal with gravity. Intraoperatively, the mass was an abscess (Figure 2d) and flakes were coming out of central canal with Valsalva maneuver and this finding confirms our hypothesis. We named this radiological sign as ‘precipitation sign’ or ‘drop sign’ indicating that the mass is precipitated pus. Drop sign or precipitation sign, in the presence of T2 hyperintensity of the cord is highly suggestive of intramedullary tubercular abscess and helps in the early diagnosis of tuberculosis and early institution of therapy.
(a) MRI T2 sagittal view whole of cord showing holocord hyperintensities; MRI T2-weighted sagittal view of the dorsolumbar spine of the two patients. (b, c) Intradural extramedullary mass at the lower end of the spinal cord (arrow), which we call as precipitation sign; (d) intraoperative picture showing fluffy mass at the lower end of the cord.
The lack of neurological improvement may be due to delay in diagnosis as in the first case, resistance to primary ATT as in the second case or may be due to associated vasculitis. Advancements in the diagnostic modalities and early detection of M. tuberculosis in in vitro culture can aid in early diagnosis.
Conclusion
Presence of an intradural extramedullary mass at the lower end of the spinal cord associated with long segment T2 hyperintensities of the spinal cord can be called as precipitation sign and should raise the suspicion of intramedullary tubercular abscess.
References
Bommakanti K, Alugolu R, Chittem LR, Patil M, Purohit AK . Fulminant holocord intramedullary tubercular abscess with enigmatic presentation. Surg Neurol Int 2013; 4: 32.
Misra UK, Kalita J . Role of MRI in acute transverse myelitis. Neurol India 1999; 47: 253–254.
Murthy JM, Reddy JJ, Meena AK, Kaul S . Acute transverse myelitis: MR characteristics. Neurol India 1999; 47: 290–293.
Süzer T, Coşkun E, Tahta K, Bayramoğlu H, Düzcan E . Intramedullary spinal tuberculoma presenting as a conus tumor: a case report and review of the literature. Eur Spine J 1998; 7: 168–171.
Malik N, Behari S, Ansari MS, Jaiswal AK, Gupta P, Jain M . An intramedullary tuberculous abscess of the conus in a 5-year-old child presenting with urinary dysfunction. World Neurosurg 2011; 76: 592.
Barbier O, Tine I, Blondet E, Goasgen O, De Soultrait F . [Intramedullary tuberculoma of the conus: a case report]. Neurochirurgie 2009; 55: 561–564.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Chittem, L., Bommanakanti, K. & Alugolu, R. ‘Precipitation sign’: a new radiological sign for spinal intramedullary tubercular abscess. Spinal Cord 52 (Suppl 1), S1–S2 (2014). https://doi.org/10.1038/sc.2014.31
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2014.31
Keywords
This article is cited by
-
Spontaneous intramedullary abscesses caused by Streptococcus anginosus: two case reports and review of the literature
BMC Infectious Diseases (2022)
-
Streptococcus pneumoniae meningitis complicated by an intramedullary abscess: a case report and review of the literature
Journal of Medical Case Reports (2016)