Abstract
Study design:
This is a case report.
Objectives:
The objective of this study was to report on a brain–computer interface (BCI) paradigm that is successfully used with an inpatient spinal cord injury patient.
Setting:
This study was conducted in an inpatient rehabilitation hospital.
Methods:
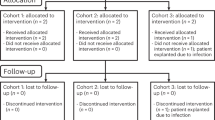
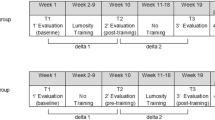
A 25-year-old man with a C5 burst fracture and subsequent tetraplegia (The American Spinal Injury Association) participated in this case study. He completed a brief battery of psychological, pain, cognitive and other screening measures at points before and after the BCI paradigm during his rehabilitation hospitalization.
Results:
The paradigm was easily learned and well tolerated with no adverse effects.
Conclusions:
This case is reflective of the trends in our ongoing feasibility study evaluating BCI technology in the inpatient rehabilitation setting. Clinical implications and challenges of using this technology in a busy hospital unit are reviewed.
Similar content being viewed by others
Introduction
In an attempt to widen the utility of computer-assisted devices and to increase independence among spinal cord injury (SCI) populations, brain–computer interface (BCI) technology has generated great interest.1 BCIs do not depend on the central nervous systems normal output pathways that have been compromised following injury. Instead, participants overtly manipulate their brain activity as compared with using motor movements to produce signals that can be used to control devices and/or virtual environments.2 To date, the majority of BCI studies in persons with SCI have revolved around motor-based activity and communication with case examples and small studies.
The potential of BCI in neuropsychological facets of SCI recovery is our group’s focus. Specifically, we foresee BCI technology as a possible tool for pain and stress management, leisure activity exploration and cognitive assessment/ intervention for patients with more severe motor impairment such as tetraplegia. This interest is further fueled by increasing support for psychological, social and non-motor-based factors as key aspects in perceived quality of life following SCI.3 Introduction of BCI during inpatient rehabilitation allows for extensive training and modification of the technology, which would be less feasible on an outpatient basis.
To our knowledge, BCI technology has not been used with inpatient SCI patients in a systematic manner as part of inpatient rehabilitation treatment. This case study is a part of our larger feasibility study including standard screens of mood, pain and cognition on our inpatient unit to evaluate whether BCI technology is tolerated, enjoyed and could be used in future work targeting previously mentioned therapeutic goals.
Case report
A 25-year-old man with a C5 burst fracture and C3 facet joint fracture secondary to a dive into a swimming pool participated in this case study. He had no additional coexisting conditions or significant medical/neurological complications from the event. Upon admission to the inpatient rehabilitation unit 2 months after his injury, he presented with tetraplegia and required maximum assistance to complete all daily activities. Physiatrist examination at admission of his 5-week stay was consistent with a C6 left motor, C5 right motor and C4 sensory The American Spinal Injury Association A grading on the International Classification of Spinal Cord Injury scale.
Measures of mood, pain and cognition were administered pre–post BCI trial. The Emotive EEG gaming system (Emotiv EPOC; http://emotiv.com) yields less sophisticated electroencephalography data than traditional medical devices,4 but the minimal cost and portability made it a preferred system. The ability to manage a virtual environment was assessed with a cube rotation and manipulation paradigm presented on a laptop computer. After a training session for each task (push cube, move left, move right and cube disappearance), the subject performed three trials, lasting 8 s each. This brief paradigm with graduated complexity was chosen to minimize the time of BCI trials in the event of adverse effects, yet still yield data on subject receptiveness and mastery of a basic BCI experience. The subject successfully completed 92% of trials and typically moved the onscreen stimuli in <2 s.
Results and Discussion
This case study suggests that the simulation technology and BCIs may be safely and successfully used with individuals undergoing inpatient SCI rehabilitation. Our subject reported that he enjoyed the experience (80 on 1–100 scale with 100 being maximal enjoyment) and denied adverse effects from the virtual paradigm, which is consistent with preliminary feedback from our larger feasibility study.
The subject demonstrated no specific cognitive strengths or premorbid proclivity for manipulating a virtual environment, yet easily learned the paradigms. Furthermore, rating scales did not suggest any negative effects on mood or pain level during the activity. In fact, the subject anecdotally described this as an enjoyable deviation from his typical therapy regime. The next step is the development of clinically related paradigms targeting our SCI inpatient team goals of pain and stress management. For example, by integrating biofeedback and progressive muscle relaxation principles, a BCI paradigm could be a nonthreatening way to teach psychological techniques for the subgroup of inpatients resistant to traditional psychological intervention after their injury.
It is important to note that this case presented a challenge related to the integration of this activity in the hospital setting. Specifically, environmental factors including finding a quiet area in a busy rehabilitation floor, managing a patient’s schedule with other disciplines and the mental/physical fatigue that can affect engagement in virtual immersion activities mandate careful planning of such patient activities. Ideally, our larger feasibility study will help identify a model amenable to use in inpatient settings with minimal disruption to traditional rehabilitation therapies.
References
Shih JJ, Krusienski DJ, Wolpaw JR . Brain-computer interfaces in medicine. Mayo Clin Proc 2012; 87: 268–279.
Millan JD, Rupp R, Muller-Putz GR, Murray-Smith R, Giugliemma C, Tangermann M et al. Combining brain-computer interfaces and assistive technologies: state-of-the-art and challenges. Front Neurosci 2010; 4: 10.3389/fnins.2010.00161. eCollection 2010.
Tate DG, Boninger ML, Jackson AB . Future directions for spinal cord injury research: recent developments and model systems contributions. Arch Phys Med Rehabil 2011; 92: 509–515.
Duvinage M, Castermans T, Petieau M, Hoellinger T, Cheron G, Dutoit T . Performance of the emotiv epoc headset for P300-based applications. Biomed Eng Online 2013; 12: 56.
Acknowledgements
The authors wish to acknowledge the Baylor Institute for Rehabilitation Spinal Cord Injury team for their support of this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Salisbury, D., Driver, S. & Parsons, T. Brain–computer interface targeting non-motor functions after spinal cord injury: a case report. Spinal Cord 53 (Suppl 1), S25–S26 (2015). https://doi.org/10.1038/sc.2014.230
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2014.230