Abstract
Background context:
Spondyloarthropathy has been described radiographically in patients following paralysis from spinal cord trauma. Onset of these findings after cauda equina syndrome have not been reported previously. Furthermore, the magnetic resonance documentation of its early evolution has not been recorded.
Purpose:
We report a case of early-onset spondyloarthropathy shown by magnetic resonance imaging (MRI) in a patient with cauda equina syndrome due to bilateral sacral insufficiency fractures.
Study design:
Unique case study review, one case.
Methods:
Review of the clinical case notes and imaging including initial and subsequent MR imaging.
Results:
The initial MRI of the lumbosacral spine showed bilateral sacral insufficiency fractures with a kyphotic deformity. The vertebral bodies were normal on the initial computed tomography and MRI studies, which did not reveal pre-existing features of sacroiliitis. The second MRI performed 5 months later clearly showed spondylitis at multiple vertebral levels with partial resolution 18 months post injury.
Conclusion:
Spondyloarthropathy in patients with paralysis due to spinal cord injury is well documented in the English language literature, but until now this has not been demonstrated by MRI. It is a rare complication of traumatic cauda equina syndrome that commences soon after the traumatic event and can resolve spontaneously.
Similar content being viewed by others
Introduction
Spondyloarthropathy has been reported in the literature to be associated with paralysis induced by spinal cord injury.1, 2 Although the association is accepted, its aetiology is uncertain. There have been no reported cases in the literature of traumatic sacral cauda equina syndrome causing these findings. Furthermore, the role of magnetic resonance imaging (MRI) in its detection is undefined.
Case report
A 74 year old presented with a history of urinary and faecal incontinence following a trivial fall from standing. Clinically, the sacrum was painful. No loss of sensation, power or motor function was demonstrated in the lower limbs, the patient was mobilising with crutches. There was loss of sensation demonstrated in the S2–5 dermatomes.
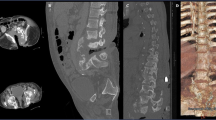
Radiographs (Figure 1), computed tomography (CT; Figure 2) and MRI (Figure 3) showed displaced insufficiency fractures of the sacrum with bilateral pubic rami fractures suspected to be due to metabolic bone disease. In the sacrum, this was accompanied by compromise of the spinal canal and cauda equina at the S2 level. The marrow MRI signal of the vertebral bodies was normal. The initial cross-sectional imaging did not show pre-existing sacroiliitis. The pelvic fractures were treated conservatively. The neurological findings were persistent and the patient subsequently underwent suprapubic catheter insertion due to a neurogenic bladder. Initial and subsequent blood tests demonstrated a raised C-reactive protein and erythrocyte sedimentation rate.
MRI 5 months after the initial investigation demonstrated new low T1, high T2 and short tau inversion recovery (STIR) signal along the anterior corners and borders of the lumbar vertebral bodies consistent with Romanus lesions of spondyloarthropathy. High STIR signal was observed in the posterior ligamentous complex in keeping with enthesitis (Figures 4a–c). MRI performed 18 months after the initial event demonstrated vertebral body enthesitis resolution but persistence in the posterior ligamentous complex (Figures 5a–c). At this stage, the original neurological findings, including neurogenic bladder, was persistent. Management remained conservative with spinal rehabilitation support.
Sagittal MRI of the lumbosacral region 5 months after injury. (a) T1, (b) T2 and (c) STIR weightings, showing a displaced sacral fracture with compromise of the spinal canal. The vertebral bodies demonstrate low T1 (a), high T2 (b) and STIR (c) signal in the anterior aspects of the vertebral bodies (open arrows) and the posterior ligamentous complex in keeping with enthesopathy (closed arrows).
Discussion
Paralysis-associated spondyloarthropathy is a described but not well-known complication of spinal injury. The literature reports a variety of radiological appearances. In 1995, Fiske et al.1 reported these changes as a mimic of ankylosing spondylitis with findings of sacroiliac joint (SIJ) fusion, vertebral disc calcification and syndesmophytes on radiographs. A study of a series of 200 patients2 reported a wide range of radiographic appearances developing subsequent to paralysis including paravertebral ossification, syndesmophytes and SIJ fusion. None of these reports benefited from the sensitivity of MRI.
The Romanus lesion, originally described by Romanus in 1952, on radiographs shows characteristic vertebral body endplate erosions with associated osteitis producing the so called ‘shiny corner sign’. MRI has been shown to be highly specific in the identification of early Romanus lesions3 and in differentiating them from other discovertebral lesions.4 This is demonstrated on MRI classically as a sharply marginated, triangular area of high marrow signal on fluid-sensitive sequences primarily at the anterior corners of the vertebral bodies.
When comparing the index case with previous studies based on radiographs, the common factors are evidence of new onset of axial spondyloarthropathy with prior onset of permanent neurological compromise. There was no evidence of pre-existing inflammatory spondylitis on the initial CT and MR of the spine and SIJs. Our patient had relatively preserved mobility, therefore inactivity is unlikely to be a causative factor. What triggers the post-paralysis spondyloarthropathy process is unknown. Martinez et al.5 examined the relationship between the disease activity and infection in patients demonstrating spondyloarthropathy in 2004. Martinez concluded that there was a statistically significant correlation between enteric and to a lesser extent urinary tract infections (UTIs) and spondyloarthropathy in a non-traumatic population. Given the established relationship between neurogenic bladder and chronic UTI, this could potentially be an instigating trigger for the findings in a spinal injury population.
On the basis of the radiographic findings, axial spondyloarthropathy complicating spinal paralysis was assumed to be a long-term complication.1 The MRI features of spondyloarthropathy seen in our case show that these changes can occur in a short period following injury and can also resolve.
Conclusion
This case report underlines the appearance of axial spondyloarthropathy associated with traumatic injury. Previously, this has been demonstrated by radiographs. In this case, it is identifiable early on MRI. In addition to this, our case shows that this can occur in the absence of limb paralysis. The aetiology of the development of spondyloarthropathy following spinal injury cannot be adequately established from this or previous data; however, given the prevalence of infection in the spinal injury population, we postulate that this adds some weight to a potential relationship between the inflammatory response observed and coexisting infection.
Data Archiving
There were no data to deposit.
References
Fiske DN, Bush CH, Edwards NL . Axial skeletal changes in paralysed patients may mimic ankylosing spondylitis. Br J Rheumatol 1995; 34: 174–177.
Park YH, Huang GS, Taylor JA, Marcelis S, Kramer J, Pathria MN et al. Patterns of vertebral ossification and pelvic abnormalities in paralysis: a study of 200 patients. Radiology 1993; 188: 561–565
Jevtic V, Kos-Golija M, Rozman B, McCall I . Marginal erosive discovertebral ‘Romanus’ lesions in ankylosing spondylitis demonstrated by contrast enhanced Gd-DTPA magnetic resonance imaging. Skeletal Radiol 2000; 29: 27–33.
Jevtic V . Magnetic resonance imaging apperences of difficult discovertebral lesions. Eur Radiol 2001; 11: 1123–1135.
Martinez A, Pacheco-Tena C, Vazquez-Mellado J, Burgos-Vargas R . Relationship between disease activity and infection in patients with spondyloarthopathies. Ann Rheum Dis 2004; 63: 1338–1340
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Ginder, L., Porter, N., Subedi, N. et al. MRI of inflammatory spondyloarthropathy following traumatic cauda equina syndrome. Spinal Cord 53 (Suppl 1), S6–S9 (2015). https://doi.org/10.1038/sc.2014.190
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2014.190