Abstract
Study design:
Retrospective study.
Objectives:
Spinal cord injuries are usually associated with anejaculation, but few premature ejaculations (PE) are described in lumbosacral lesions. The objective of the study is to analyze the retrospective files of patients with lumbosacral lesions to explore whether PE is systematic, and which type of lesions (conus teminalis, epiconal, cauda equina) is associated with these PE.
Methods:
Standard sexological consultations from 34 men with L5-S4 lesions were analyzed including questions on psychogenic and reflexogenic erection, and ejaculation. Medical assessment included bulbocavernosus, anal, and cremasteric reflexes and urodynamics.
Results:
Thirty one (31/33) patients maintained natural ejaculations, but 18 complained of PE and five of spontaneous ejaculations. Fourteen patients complained of dribbling ejaculation, and 27 of non-climactic ejaculation (13 no sensation, 10 some sensation, 4 painful sensation). Medical assessments showed absent or diminished anal sensation in 28 patients, absent or diminished anal reflexes in 21, absent or diminished bulbocavernosus reflexes in 20, but 12/13 positive cremasteric reflex. Urodynamics showed 12/20 areflex and 2/20 hyperactive bladders.
Conclusions:
Most men with lower lumbosacral lesions maintain natural ejaculation, but often complain of PE following injury. The PE is such that a mere sexual thought can trigger the response, or appear spontaneously as daytime (‘sticky paints’) or nighttime (‘sticky sheets’) emissions. PE appears to be a direct consequence of the lesion as it is reported from the very first ejaculation post injury, in men who otherwise controlled their ejaculation prior to injury. Underlying mechanisms may involve sacral inhibition on ejaculation, or simultaneous activation of psychogenic erection and emission. Clinical implications are discussed.
Similar content being viewed by others
Introduction
Spinal cord injuries (SCI) are most often associated with a loss of ejaculation,1 at least with natural stimulation.2 Although most authors have emphasized this loss of ejaculation following injury, a few authors have described the occurrence of premature ejaculations (PE),3, 4, 5, 6, 7, 8 arising after the injury and related to lower lesions to lumbar or lumbosacral segments of the spinal cord (that is, conus terminalis, epiconal or cauda equina).
These PEs, described by a few authors and a few patients, appear to be triggered by psychogenic stimulation,3, 4, 5, 6, 7 or to occur spontaneously without sexual arousal, or during the night but in the absence of erotic dream or feeling of orgasm. The ejaculations are most often described as dribbling,5,9 and while they are generally triggered by psychogenic stimulation, they often remain anhedonic.3, 6 This phenomenon is in marked contrast with the reflex expulsive ejaculations that are observed in men with higher spinal lesions (for example, cervical or thoracic lesions).10, 11, 12, 13, 14
This study was designed to analyze the retrospective data from patients with lower lumbosacral lesions who have consulted our sexual dysfunction clinic in rehabilitation over the past 20 years. The goal was to explore to what extent these PEs are systematic in men with lower lumbosacral lesions (that is, L5 and below), and if so which specific type of lumbosacral lesions (that is, conus terminalis, epiconus, cauda equina) appear to be associated with this phenomenon. The findings are discussed in terms of our current knowledge on the neurophysiology of ejaculation.
Materials and methods
Patients
The data were collected from the clinical files of 34 patients whose lesions varied from L5-S1 to S4-S5 and who have consulted for sexual dysfunctions over the past 20 years. The average age of the patient was 41 years (range 19–65 year old) and the average delay since injury 10 years (range 3 months from 53 years). Inclusion criteria involved having a stable lesion for at least 3 months at the time of sexological consultation, with no other medical conditions than the spinal lesion that could affect sexual function (for example, diabetic patients were excluded). Degenerative conditions (for example, amyotrophic lateral sclerosis) or congenital spinal defects (for example, spina bifida) were excluded from analysis.
Procedure
The data were gathered from the patients’ clinical files. The standard American International system of classification of spinal lesions was not always provided given the retrospective nature of the study, which included patients admitted in the center from 1991 to 2012. However, the neurological examination, the sexological assessment and the urological data (involving perineal testing) allowed to reconstruct the patients’ American International system level.
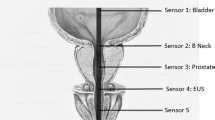
Standard sexological consultations in our centers involve a systematic interview (based on a clinical form which we developed) covering questions on urinary function and bowel regulation (as related to sexual intimacy) and sexual function, in particular the occurrence of psychogenic and reflexogenic erections and the occurrence of ejaculation since the injury. The questions are usually followed by an open interview allowing the patients to further discuss particular issues concerning their sexual function. These interviews are complemented with a medical exam, which includes testing of perineal reflexes, namely the bulbocavernosus reflex, the anal reflex and the cremasteric reflex. In the first case, the reflex is triggered by applying pressure on the glans penis, while visually observing or palpating the resulting contraction of the bulbospongiosus muscle located under the scrotum, based on a 3-point scale (absent=0, doubtful=1, present=2). In the second case, the anal reflex is triggered by pinprick stimulation applied on the left and right margin of the anus, whereas visually observing the resulting anal contraction, again based on a 3-point scale. In the third case, the cremasteric reflex is triggered by gentle stroking of the left and right inner thigh while visually observing testicle elevation ipsilateral to the stimulation site. The neurological examination also involves the assessment of anal sensation and anal contraction. In the first case, anal sensation was assessed on the left and right margin for both touch and pinprick sensation, and scored from 0 to 2 (0=no sensation, 1=poor sensation, 2=normal sensation). The data were summarized in the patients’ clinical file as an overall lack, poor or normal anal sensation (Table 1). In the second case, anal contractions were tested through voluntary contraction of the anal sphincter during rectal touch and clinically scored on a 5-point scale as for other muscle groups. However, as the American International system classification system uses a Yes/No response for voluntary anal contraction, any score above 0 was transformed as a positive anal contraction (Table 1). Available data from urodynamics were further collected to identify whenever possible the type of bladder (for example, areflexive, hyperactive or normal) associated with the patient’s lesion. The responses of all patients to these various tests are reported in Table 1.
All patients were informed that their clinical data could be used for scientific publications or communications, and verbally accepted their use for scientific purposes, in accordance with the declaration of Helsinki on human rights and ethical standards of research. Since 2005 all patients sign an informed consent approved by the Institutional Ethics Committee.
Results
The patients’ neurological and other medical variables are summarized in Table 1. The data (see bottom of variable columns) reveal that 15 patients had a complete absence of anal sensation, 13 had diminished or paraesthetic sensation and six had normal sensation. The anal reflex was lost or diminished in 21 patients and normal in eight. The bulbocavernosus reflex was similarly lost or diminished in 20 patients, and normal in 10. In contrast, the cremasteric reflex (when tested) was present in most patients, only one showing an absence of response. Available data from urodynamics showed that neurogenic bladders were generally areflex and acontractile. Only two patients showed a central hyperactive bladder.
The results from the sexological interview are illustrated in Table 2. The data (see bottom of variable columns) reveal that 31 out of the 33 patients (94%) were capable of natural ejaculation (that is, upon sexual arousal, masturbation or intercourse) despite their spinal lesion. Only two patients complained of anejaculation. The clinical interview further revealed that 18 patients complained of PE, a condition they described as having appeared after the injury in men who otherwise controlled their ejaculation prior to injury. In many cases, the PE was described as occurring following a mere sexual thought or a vague sexual desire. Three patients further reported spontaneous ejaculations, which they observed as ‘wet and sticky pants’ without having been consciously aware of any sexual stimulation. Two additional patients reported nocturnal emissions, described as ‘wet and sticky sheets’ again without having been aware of sexual dreams or feeling of orgasm.
Fourteen patients mentioned that their ejaculation was dribbling, 15 gave no information on this aspect of ejaculation and five indicated that the stream was normal or of no concern. Most patients described the ejaculation as non-climactic, 13 reporting a complete absence of sensation (for example, did not feel the ejaculation or perceived it as a feeling of seminal incontinence), 10 reported some sensation but emphasized that they were markedly diminished since the lesion (for example, feeling ‘shivering in the lower back’, feeling ‘some but non-climactic sensations’, reporting ‘a few’ or ‘very little sensation’, reporting a ‘marked decrease in sensations’), and four reported painful sensations (for example, electric discharge in the feet or painful sensation in the legs and abdomen). Some patients described changes in penile aspects (for example, more intense erection preceding ejaculation) but most referred to other peripheral events to characterize climax. Only two men reported orgasm with both genital and autonomic perceptions, one however described the experience as less intense than before the injury.
In terms of erectile function, 18 patients reported maintaining both psychogenic and reflexogenic erections, and six only psychogenic erections. Eight patients reported a complete absence of erection, or erections of such poor quality that sexual activities (including intercourse) were impossible. One patient described only morning erections, and one described painful erections (pin-and-needle sensations).
In an attempt to assess the predictors of PE, a correlation matrix was further performed between all variables (Table 3). Surprisingly, few significant correlations were found as predictors of PE, the only significant association being between PE and dribbling ejaculation (r=0.37, P<0.05). Other medical variables were significantly correlated with each other. As such, the completeness of the lesion was significantly correlated with anal sensation (r=0.84, P<0.01), anal testing (r=0.81, P<0.01), anal reflex (r=0.55, P<0.01) and bulbocavernosus reflex (r=0.43, P<0.05). Other correlations were found between anal sensation and reflex erection (r=0.40, P<0.05), anal testing and reflex erection (r=0.38, P<0.05), and psychogenic and reflexogenic erections (r=0.55, P<0.01).
Discussion
The data based on the retrospective analysis of 34 clinical files confirm that most men with lower lumbosacral lesions (up to 94%) are capable of natural ejaculations (that is, upon sexual arousal, masturbation or intercourse), but that most of these ejaculations have become premature since the injury. The premature nature of the ejaculation is such that a mere sexual thought can trigger the response, or the response can occur spontaneously (‘sticky pants’) without obvious genital stimulation or conscious awareness of sexual arousal, or at the night during nocturnal emissions (‘sticky sheets’) but again without conscious awareness of erotic dream or nocturnal orgasm. The premature nature of the ejaculation appears to be a direct consequence of the spinal lesion, since it is reported from the very first experience of ejaculation following injury, and in men who otherwise reported controlling their ejaculation prior to injury.
A few authors in the literature have described these PEs in men with lower SCI. As early as 1950, Meirowsky and Shcheibert8 mentioned that some patient with sacral lesions (S3-S4) experienced ejaculation that ‘could not be voluntarily delayed’. Bors and Comarr3 in 1960 later described a few cases of premature ejaculators among their 529 patients with SCI, but described the phenomenon as a rare event, and linked it to complete lower motor neuron lesions. Comarr4 in his extensive series of men with SCI confirmed that ‘quicker ejaculators’ were found among men with complete or incomplete upper motor neuron lesions and lower motor neuron to the lumbar segments, and Larsen and Heijgaard7 described 13 cases of premature ejaculators among men with incomplete lesions, but without further developing on the issue or on the lesion level associated with such ejaculations. Kuhr et al.6 (1995) as far as we know are the only authors who specifically described six cases of PE following SCI and who specifically linked them to lumbosacral lesions, and associated with poor or absent sacral reflexes and flaccid bladders.
In contrast to these reports on men with lumbosacral lesions, many authors have reported the poor ejaculation potential of men with higher spinal lesions, at least with natural stimulation (masturbation, intercourse). First, Bors and Comarr,3 then Comarr,4 and more recently Hubscher15 and Chéhensse et al.,1 reported that only 5–10% of men with SCI maintain a natural potential for ejaculation despite their lesion. Although these figures increase drastically when vibrostimulation is used,11, 12, 15, 16 and even more so when midodrine is added to vibrostimulation,12, 14 studies generally emphasize the difficulty in obtaining ejaculation in men with SCI. In this context, report of PE with psychogenic arousal is extremely unusual, especially as these men report that prematurity appeared following the injury.
Attempts to explain this phenomenon are not easy. Although previous reports variably linked the phenomenon to complete or incomplete lower motor neuron lesions3, 4 or to lumbar and lumbosacral lesions,4, 6 the current data suggest that they may be more specifically linked to lesions to the conus terminalis. Although many patients had incomplete lesions (making definite conclusions difficult), the neurological examination revealed that the sacral reflexes were generally impaired, and the urodynamics that most patients had an acontractile and areflex bladder. These two findings suggest that the sacral segments (S2–S4) of the spinal cord were damaged, resulting in conus terminalis lesions (or damage to the sacral fibers of the cauda equina) rather than epiconal lesions (that is, damage to L4–L5 segments). Further data from the cremasteric reflex, indicating positive tests in 92% of the patients tested, support the hypothesis of conus terminalis lesions rather than higher cauda equina lesions damaging the lumbar together with the sacral nerves.
As mentioned before, few authors described these PEs in men with lower SCI. They generally described them as triggered by psychogenic stimulation.3, 5, 6 Consistent with the literature, the current findings showed that the PEs were often triggered by psychogenic stimulation, described by sexual thoughts, or occurred spontaneously. Furthermore, 71% of the patients reported psychogenic erections (alone or in combination with reflexogenic erections), supporting psychogenic mediation of sexual responses.
The underlying mechanism for such PEs in men with lower SCI remains a mystery. Observation of dribbling ejaculation in men with lumbosacral lesions is not surprising, given the impaired innervation of the perineal muscles responsible for expulsive ejaculation, which has been described by authors in the early literature.3, 4, 9 Complaints of anhedonic or non-climatic ejaculation, or lack of orgasm in men with lower motor neuron lesions has been described elsewhere17 and is unsurprising given that these patients have lost sensation caudal to the lesion, in particular from their genitals. Lost climactic sensation during ejaculation might also be explained by the fact that these men with lumbosacral lesions cannot experience even mild autonomic hyperreflexia which has been associated with climactic responses in men with SCI.12, 13, 18 Yet, the premature nature of ejaculation following lower SCI remains a mystery.
Possible interpretations involve the removal of inhibition on ejaculation, an interpretation that is consistent with descending pathways innervating the genitals.15 As these men with lumbosacral lesions preserve psychogenic erection but have impaired neurological transmission, it may also be that they have lost the ability to control psychogenic arousal and can no longer inhibit ejaculation. It may also be that sensory inputs from the genitals normally exert some inhibition on ejaculation, and that this inhibition is necessary to delay ejaculation (possibly to build up sexual tension). Damage to the sacral segments in lumbosacral lesions would prevent such early inhibition8 and possibly explain the PE. As seminal emission in men with lower spinal lesions are reported to be triggered primarily with psychogenic stimulation, stimulation may simultaneously trigger psychogenic erection and emission, which would explain how ejaculation occurs prematurely and concurrently during the phase of sexual arousal (rather than the phase of emission-ejaculation).
These interpretations appear consistent with findings and assumptions from the literature. A recent distinction between parasympathetic secretion of the internal reproductive organs that occurs during sexual arousal and sympathetic contraction of their smooth muscle envelope that occurs during emission has been highlighted.19 This distinction may explain the possible differentiation between parasympathetic dribbling ejaculation, observed in lower lesions and upon psychogenic stimulation and expulsive sympathetic (and somatic) ejaculation, observed in able-bodied men or men with higher spinal lesions.
Studies on men with SCI have also introduced a distinction between psychogenic and reflexogenic erections.3, 20, 21 Sipksi et al.,22 in particular demonstrated the usefulness of assessing the integrity of pinprick sensation in the T11-L2 dermatomes to predict psychogenic arousal in men with SCI. Animal studies further confirmed the existence of two functional pathways mediating erection: one mediated through the sacral segments of the spinal cord and one through the thoracolumbar (TL) segments.23 Later studies further differentiated TL fibers mediating erection and running through the paravertebral sympathetic chain feeding into the pelvic plexus24 and TL fibers mediating emission and running through the peripheral hypogastric nerves innervating the internal reproductive organs. It may be that the TL fibers mediating psychogenic erection and psychogenic emission are activated simultaneously in men with lower SCI when they are sexually aroused (again suggesting some inhibition from lower spinal pathways).
These interpretations are speculative. They attempt to explain the observed data on PEs that appear to arise as a direct consequence of lower lumbosacral lesions. The interpretations are necessarily limited by the retrospective nature of the study (despite our attempts to systematically include all patients interviewed in sexual rehabilitation and our attempts to standardize the sexological interviews with a clinical form). The interpretations are also limited given the incompleteness of many spinal lesions, a common finding in human studies (of which patients are grateful), and by the selected levels of the lesions, which specifically aimed L5 and below (as suggested by the literature and clinical experience). The findings (and future research) would benefit from a comparison with a larger sample, including men with higher cauda equina lesions (expected to present anejaculations) and higher spinal lesions (also expected to present anejaculations) to further support the evidence of PEs arising specifically from lower lumbosacral lesions, and in particular conus terminalis lesions.
Despite these further confirmations, clinical consultations from patients with lower spinal lesions are not uncommon in sexual rehabilitation, and pose a number of questions for treatment. Given the lower lumbosacral lesions, these patients typically walk (with or without a foot orthesis, and with or without crutches) and show little overt disability, but generally suffer from gas, urinary and fecal incontinence, and as shown in this study, a form of seminal incontinence. These patients also suffer from severe erectile dysfunction, which is seldom treated successfully with phosphodiesterase inhibitors (sidelnafil, tadalafil, vardenafil), and which usually requires intracavernous injections (papaverine, prostaglandins or trimix) or a combination of treatments. Their PEs may be treated with antidepressive drugs such as selective serotonin reuptake inhibitors (for example, sertraline, fluoxetine, paroxetine),13 which are known for their side effects on ejaculation, but follow ups would be required to explore the patients’ satisfaction with these treatments (for example, the treatments may not help for the already poor sensations felt during ejaculation). Upon satisfaction with selective serotonine reuptake inhibitors (SSRIs), the new Dapoxetine treatment (a short acting SSRI) would be promising, although the drug is not universally available (in particular in North America where it has not received Food and Drug Administation approval). Erectile dysfunction treatments may also be considered in cases of these extremely PEs in order to maintain erection and intercourse. As most patients have incomplete lesions, they may be encouraged to use cognitive modulation to reduce the intensity of erotic stimulation, and to use genital stimulation in an attempt to increase the inhibition arising from sacral stimulation in order to provide a build up of sexual tension prior to ejaculation.
Conclusion
Lesions to the lower lumbosacral segments, and more specifically to the conus terminalis, appear to result in PE in men with SCI. The severity of the PE is such that it is often triggered by a mere sexual thought. The underlying mechanism responsible for this neurologically acquired PE remains to be demonstrated. Data from human studies on men with SCI and from animal studies suggest that the sacral pathway exerts some inhibition over the TL pathway, or that psychogenic erection and emission are triggered simultaneously in these lower lesions. More research is required to define which specific neural conditions give rise to this form of PEs and which underlying mechanism may be responsible for the dysfunctional response acquired post injury.
Data archiving
There were no data to deposit.
References
Chéhensse C, Bahrami S, Denys P, Clément P, Bernabé J, Giuliano F . The spinal control of ejaculation revisited: a systematic review and meta-analysis of anejaculation in spinal cord injured patients. Hum Reprod Update 2013; 19: 507–526
Courtois F, Charvier K, Carrier S, Vézina J-G, Côté I, Dahan V et al. Sexual function and treatment options for men with spinal cord injury. Funct Neurol Rehabil Ergon 2013; 3: 29–58
Bors E, Comarr AE . Neurological disturbances of sexual function with special reference to 529 patients with spinal cord injury. Urol Surv 1960; 10: 191–222.
Comarr AE . Sexual function among patients with spinal cord injury. Urol Int 1970; 25: 134–168.
Comarr AE . Sex classification and experctations among quadriplegics and paraplegics. Sexuality & Disability 1978; 1: 252–259.
Kuhr CS, Heiman J, Cardenas D, Bradley W, Berger RE . Premature emission after spinal cord injury. J Urol 1995; 153: 429–431.
Larsen E, Hejgaard N . Sexual dysfunction after spinal cor or cauda equina lesions. Paraplegia 1984; 22: 66–74.
Meirowsky A, Scheibert CD . Studies on the sacral reflex ar in paraplegia. III Clinical observations on inhibitory impulses within the sacral reflex arc. Exp Med Surg 1950; 8: 437–448.
Tarabulcy E . Sexual function in the normal and in paraplegia. Paraplegia 1972; 10: 201–208.
Biering-Sørensen I, Hansen RB, Biering-Sørensen F . Sexual function in a traumatic spinal cord injured population 10-45 years after injury. J Rehabil Med 2012; 5 44: 926–931.
Brackett NL, Lynne CM, Ibrahim E, Ohl DA, Sønksen J . Treatment of infertility in men with spinal cord injury. Nat Rev Urol 2010; 7: 162–172.
Courtois FJ, Charvier KF, Leriche A, Vézina J-G, Côté M, Raymond D et al. Perceived physiological and orgasmic sensations at ejaculation in spinal cord injured men. J Sex Med 2008; 5: 2419–2430
Courtois F, Carrier S, Charvier K, Guertin P, Morel Journel N . The control of male sexual responses. Curr Pharm Des 2013; 19: 4341–4356
Soler JM, Prévinaire JG, Plante P, Denys P, Chartier-Kastier E . Midodrine improves ejaculation in spinal cord injured men. J Urol 2007; 178: 2082–2086.
Hubscher CH . Ascending spinal pathways from sexual organs: effects of chronic spinal lesions. Prog Brain Res 2006; 152: 401–414.
Sønksen J, Biering-Sørensen F, Kristensen JK . Ejaculation induced by penile vibratory stimulation in men with spinal cord injuries. The importance of the vibratory amplitude. Paraplegia 1994; 32: 651–660.
Sipski M, Alexander CJ, Gómez-Marín O . Effects of level and degree of spinal cord injury on male orgasm. Spinal Cord 2006; 44: 798–804.
Courtois F, Charvier K, Vézina JG, Journel NM, Carrier S, Jacquemin G . Assessing and conceptualizing orgasm after a spinal cord injury. BJU Int 2011; 108: 1624–1633
Giuliano F, Clément P . Neuroanatomy and physiology of ejaculation. Annu Rev Sex Res 2005; 16: 190–216.
Munro D, Horne HW, Paull DP . The effect of injury to the spinal cord and cauda equina on the sexual potency of men. New Eng J Med 1948; 239: 903–911.
Talbot HS . The sexual function in paraplegia. J Urol 1955; 73: 91–100.
Sipski M, Alexander C, Gómez-Marín O, Spalding J . The effects of spinal cord injury on psychogenic sexual arousal in males. J Urol 2007; 177: 247–251.
Courtois FJ, MacDougall JC, Sach BD . Erectile mechanism in paraplegia. Physiol Behav 1993; 53: 721–726.
Giuliano F, Rampin O, Brown K, Courtois F, Jardin A, Benoit G . Stimulation of the medial preoptic area of the hypothalamus in the rat elicits increases in intracavernous pressure. Neurosci Lett 1996; 209: 1–4.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Courtois, F., Charvier, K. Premature ejaculation associated with lumbosacral lesions. Spinal Cord 52, 905–910 (2014). https://doi.org/10.1038/sc.2014.175
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2014.175