Abstract
Study design:
Single-blind randomized controlled trial of 6 months’ duration.
Objectives:
To evaluate the efficacy of a novel telehealth intervention, ‘CareCall’, on reducing pressure ulcers and depression and enhancing the use of appropriate health care.
Setting:
General community, Massachusetts and Connecticut, United States
Methods:
‘CareCall’ is an automated, interactive voice response system that combines patient education, cognitive behavioral interventions, screening and referrals, with alerts to a nurse telerehabilitation coordinator for direct non-emergent phone follow up. Participants consisted of a convenience sample of 142 persons with multiple sclerosis or spinal cord injury using a wheelchair >6 h per day. The intervention group received CareCall (n=71) The control group received usual care (n=71). The main outcome measures were: The pressure ulcer scale for healing tool, Patient Health Questionnaire—9 depression scale, Cornell Services Index and Craig Hospital Inventory of Environmental Factors-Short Form Question 5.
Results:
CareCall achieved a reduction in presence of pressure ulcers at 6 months in women (P<0.0001). Among those with baseline depression, CareCall reduced 6-month severity of depression, adjusting for age and gender (P<0.047). CareCall did not have a significant impact on health-care utilization (OR=1.8, P=0.07), but did significantly improve participants’ report of health-care availability (OR=2.03, P<0.04).
Conclusion:
This is the first study to demonstrate the efficacy of a largely automated telehealth intervention for adults with spinal cord dysfunction. Future research needs to replicate this study in a larger, multisite trial.
Similar content being viewed by others
Introduction
Secondary conditions that develop in adults with spinal cord dysfunction (SCD) can have severe consequences. Of note, pressure ulcer prevalence has increased in recent years for people with spinal cord injury (SCI), with diagnosed pressure ulcer prevalence in persons with SCI at 27%.1 Multiple sclerosis (MS), paralysis and several other diseases have been reported more often in pressure ulcer-associated deaths than in matched controls.2
Depression is another common secondary condition for persons with SCD. Approximately 1 in 5 persons with SCI have major depression, about three times the general population rate, with prevalence for most studies between 15–23%.3 People with MS also have a higher prevalence of depression than the general population.4
For persons with severe mobility impairments due to SCD, telehealth interventions have focused mostly on the prevention and management of secondary conditions, including pressure ulcers5 and depression,6 or on improving health behaviors.7 An emerging trend in creating telehealth programs is the use of interactive voice response (IVR) telephony that allows for virtual health care to monitor and assess patients' health and disease status, promote healthy behaviors and improve health outcomes. The advantages of the virtual health-care approach compared with human telehealth interventions include its relative low cost, convenience for the patient, potential for widespread use, anonymity and user acceptability.8 Despite their growing popularity, very few have been thoroughly evaluated.9
The CareCall system involves an IVR system to generate digitized speech over the telephone, speech recognition software, a conversation control system that directs the content and flow of individual conversations with users and a database management system for storing user information and call logs.10 We conducted a single-blind, randomized controlled trial to evaluate the efficacy of CareCall on several important secondary conditions for persons with SCD. Our primary hypotheses were that over a 6-month period, CareCall would: (1) decrease the prevalence of pressure ulcers, (2) decrease the severity of depression, (3) increase appropriate use of preventative outpatient health care and (4) reduce emergency room visits and hospitalizations.
Materials and methods
Study design
The intervention group received CareCall for 6 months, whereas the control group received usual care. We allocated participants to study groups using a stratified block randomization method to ensure balance by recruitment site (Boston Medical Center and Gaylord Hospital in Wallingford, CT, USA), diagnosis (MS and SCI) and acute vs chronic condition (SCI subsample only). All study staff collecting data were masked as to study group assignment.
Participants
The study’s target population consisted of persons with SCD (SCI or MS) recruited from community disability organizations, or rehabilitation medicine outpatient clinics and inpatient services, who typically used a wheelchair at least 6 h a day during normal waking hours. (See Table 1)
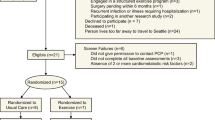
Of the 709 recruited participants (see Figure 1), 567 were excluded during the initial screen (before randomization). In total, 142 subjects were randomized into the study, with specific diagnosis breakdown of 106 with SCI and 36 with MS, of whom 133 (93.7%) completed the study. In the intervention group, 4 were lost to follow up and 2 discontinued participation, while in the control group, 3 were lost to follow up. See Figure 1 for further details.
Study measures
The project coordinator collected demographic measures from the participants by phone, as part of an initial eligibility screening, while additional background items were collected at the baseline home visit.
Pressure ulcer prevalence was measured by data collector observation using the pressure ulcer scale for healing (PUSH) tool version 3.0.11
The Patient Health Questionnaire—9 depression screener was employed to measure the severity of depression.12
Health-care utilization was measured by self-report using the Cornell Services Index.13
Health-care utilization was also measured by self-report using question 5 of the Craig Hospital Inventory of Environmental Factors-Short Form version 3.0.14
We collected information on hospital visit (yes/no) and emergency room visit (yes/no) from the Cornell Services Index, as well as the Craig Hospital Inventory of Environmental Factors-Short Form health-care availability item (never has problem/has problem) at four time points (baseline, 2-month, 4-month and 6-month).
We assessed usage of the CareCall intervention using the data collected by the IVR system. We defined nonadherence to the intervention as missing three consecutive weekly calls. The CareCall telerehabilitation coordinator kept a log of all the calls she made to and received from intervention subjects.
Data collection procedures
Data collectors administered all the outcomes assessments at baseline and 6-month visits in participants’ homes; health-care utilization data were collected by the project coordinator during 2- and 4-month follow-up calls. Each potentially eligible participant completed a CareCall training telephone call to train and confirm their ability to use CareCall at baseline. Randomization was done after the baseline visit.
Control group
The control group interacted with their health-care professionals in their usual manner per current standard of care. Control subjects received a CareCall resource book developed by clinical experts, containing information and local resources.
Intervention group
Intervention group subjects received weekly automated calls from the CareCall for 6 months and could call into CareCall any time. The CareCall scripts were organized into modules, integrating content relevant to: skin care, depression and wellness, and health-care utilization. The system also included relevant prerecorded vignettes from people with SCD, and relevant recorded comments from health-care professionals. These modules used branching logic based on personalized information and subjects’ responses during calls to tailor content throughout.
CareCall’s content was developed based on the Transtheoretical model,15 and the social cognitive theory,16 as well as the heuristics of experienced counselors and evidence-based practice as described elsewhere.10
Statistical analysis
We calculated the mean, s.d. and range for each continuous variable, and frequency distributions for categorical variables. Because of the small sample size, we dichotomized some categorical variables (for example, in the past 6 months, how often has the availability of health-care services and medical care been a problem for you? (0: never, 1–4: have some problems)). For categorical variables, the χ2 test was used to compare the proportional difference between study groups. For continuous variables, a two-group t-test was used to test the mean difference between study groups.
We used logistic regression to test for study group effects in predicting the presence of one or more pressure ulcers at 6-month assessment, adjusting for the presence of pressure ulcers at baseline, age and gender. The general linear model was used to test the study group effect in 6-month severity of depression, adjusting for baseline depression, age and gender. We tested whether there was an interaction effect between severity of baseline depression and study group assignment on the severity of depression at 6 months.
We applied the generalized estimating equation to test the group study effect on hospital visit/emergency room visit/health-care availability at 2-month, 4-month and 6-month time points, adjusting for each baseline health-care utilization variable, age and gender. We used an unstructured working correlation matrix in the generalized estimating equations model estimation. Subjects’ data were included in the health-care utilization and health-care availability analyses when at least one data point was present at baseline, 2 months, 4 months or 6 months.
The primary analysis was the intention to treat; all analyses were conducted using Statistical Analysis System software version 9.1.
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Results
Sample characteristics
The study sample (Tables 2 and 3) consisted of 106 community participants with SCI (75%) and 36 with MS (25%). Many subjects had a history of pressure ulcers (46.5%), with 7% having ulcers at baseline. Of the total sample, 38.7% had a past diagnosis of depression. At baseline, there were no statistically significant study group differences in the prevalence of pressure ulcers, mean severity of depression or the percentage reporting issues with health-care availability. However, the intervention group reported more emergency room visits and hospitalizations compared with control group subjects.
Pressure ulcers
The CareCall intervention did not have an overall positive impact on reducing the number of pressure ulcers at 6 months, controlling for baseline number of pressure ulcers, age and gender. However, among women in the intervention arm, there were no pressure ulcers at the 6-month visit (Figures 2a and b). A one side test (P=0.04) indicated that among women, there was a significant study group difference in the percentage with one or more pressure ulcers. No positive CareCall effect was seen for men (P>0.05).
Depression
The linear model analyses, controlling for age and gender, revealed a significant interaction between baseline depressive symptoms and CareCall (P<0.0006) (Table 4). Among those who reported having depressive symptoms at baseline, we observed a statistically significant difference in 6-month severity of depression between the intervention and control groups (effect size=−0.56;17 t=−2.18; P=0.038) (Figure 3). The nonparametric test (Wilcoxon two-sample test) confirmed the above finding (P=0.0495).
Health-care utilization
At the 2-, 4- and 6-month follow up periods, there were no statistically significant study group differences in the percentage of subjects who reported having an issue with health-care availability, reported emergency room visits, or hospital stays. CareCall did significantly improve subjects’ self-report of health-care availability (Table 5).
CareCall usage
CareCall calls were 13.3 min on average (range: 5–30) and subjects completed, on average, 12.4 total calls over 6 months. There were 37 intervention group subjects (22%) who were nonadherent, missing on average three calls in a row three separate times over the 6-month period. All 71 intervention participants received, on average, 11 calls from the telerehabilitation coordinator (median: 9; range: 1–39), lasting an average of 4.12 min each (median: 3.67; range: 1–14).
Discussion
This study revealed promising evidence of CareCall’s 6-month efficacy in reducing the prevalence of pressure ulcers among women and reducing the severity of depression. CareCall did not increase the use of preventative outpatient health care, nor reduce emergency room visits and hospitalizations. The study sample did, however, report increased levels of health-care availability. The impact on our hypotheses is particularly encouraging given the relatively short follow-up.
This investigation provides important new information on a promising strategy for preventing secondary conditions among adults with SCD. Two systematic reviews of follow-up care and of telerehabilitation interventions for people with SCI noted a lack of rigor in reviewed studies, and no significant differences reported in pressure ulcer development.18, 19 In this context, it is particularly notable that CareCall demonstrated efficacy on both pressure ulcer prevalence and severity of depression.
Analyses revealed that the CareCall intervention reduced the number of pressure ulcers among women but not for men. Of note, in previous research, IVR user acceptability studies have not revealed similar gender differences.8, 20 However, previous research has not included individuals with SCI.
Additional gender analysis of CareCall usage reveals some useful insights. Men in the CareCall group made a similar number of calls as women, and the average call length was similar. However, there was a borderline significant trend of more calls by women to the telerehabilitation coordinator (17.8± 15.2) than men (11.4± 7.5) (P=0.08). Moreover, within the intervention group, we observed a rather counterintuitive finding: the odds of men reporting turning in bed every 2–4 h were 4.5 times higher than for women (P=0.008), even though it was women who demonstrated reduced pressure ulcer prevalence. Other reported skin care behaviors, such as pressure relief while seated, demonstrated no significant difference by gender in the intervention group. The lack of an effect on pressure ulcers among men suggests that the basic strategies employed by CareCall to provide ongoing feedback to improve skin care behaviors, and support to overcome barriers, ultimately may not be effective for men. Future qualitative research may be useful to help understand this surprising result.
CareCall achieved improvement in depression scores over the course of the study for those with the greatest depression at baseline. We know of only one other IVR intervention study meant to reduce depression;21 as with CareCall’s depression module, it combined assessment with education and referral. CareCall, however, is the first to target persons with SCD to reduce depression, and the first to show a significant improvement at 6 months.
Despite no evidence that health-care utilization was directly affected by CareCall, intervention group participants reported that health care was more available to them post-intervention. Possibly, subjects viewed receipt of CareCall itself as increasing their access to services, particularly given CareCall’s provision of telerehabilitation coordinator telephone follow up.
A major strength of telehealth interventions is the ability to fill service gaps in the community by identifying health-related problems as they arise and offering relevant counseling and resources at point-of-need. Live telephone interventions could therefore be more tailored to an individual’s readiness to change compared with traditional rehabilitation. By contacting people within the context of their lived environment, intervention is often more relevant without relying on the person’s willingness and ability to seek out assistance. These same arguments can be extended to automated telephone interventions such as CareCall as a supplemental method to traditional rehabilitation, especially given the evidence that users do indeed form relationships with the IVR system as they would with a ‘live’ person.8
A major strength of automated interventions similar to CareCall is their potential for substantial health-care cost-savings,22 given that most traditional telephone follow up occurs at specialty medical facilities requiring dedicated staff and resources. Importantly, Xu et al.22 demonstrates savings may be achieved with little loss in efficacy. A further strength over traditional telephone follow up is CareCall’s ability to identify unmet needs even many years post diagnosis. Because CareCall is designed to work across multiple settings, it can provide a wider outreach to persons who may not be medically connected, and who, in turn, may be more likely to have unmet needs.
Study limitations
These findings must be viewed as preliminary due to the small sample in this study implemented in one region of the country across two facilities. Also, limited sample size did not allow for an analysis of differential efficacy across MS and SCI subsamples. Another limitation of the study was the need to require that participants have insurance or pending insurance and live in a private residence by virtue of the pilot nature of this study. People motivated enough to opt-in to a study may have more motivation than their peers, and perform better with CareCall. Lastly, we did not control for, nor collect data on, other treatments subjects may have been receiving.
Conclusion
CareCall offers an innovative approach to providing ongoing care aimed at preventing secondary conditions and maximizing health. This is the first study to report positive preliminary efficacy results for an automated telehealth intervention for adults with SCD. Future research needs to replicate this study in a larger sample across multiple settings in more regions of the country.
Data archiving
There were no data to deposit.
References
Chen Y, DeVivo MJ, Jackson AB . Pressure ulcer prevalence in people with spinal cord injury: age-period-duration effects. Arch Phys Med Rehabil 2005; 86: 1208–1213.
Redelings MD, Lee NE, Sorvillo F . Pressure ulcers: more lethal than we thought? Adv Skin Wound Care 2005; 18: 367–372.
Hoffman JM, Bombardier CH, Graves DE, Kalpakjian CZ, Krause JS . A longitudinal study of depression from 1 to 5 years after spinal cord injury. Arch Phys Med Rehabil 2011; 92: 411–418.
Dalton EJ, Heinrichs RW . Depression in multiple sclerosis: a quantitative review of the evidence. Neuropsychology 2005; 19: 152–158.
Regan M, Teasell RW, Keast D, Aubut JL, Foulon BL, Mehta S . Pressure Ulcers Following Spinal Cord Injury. In: Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, et al (eds). Spinal Cord Injury Rehabilitation Evidence (SCIRE), Version 4.0 (http://www.scireproject.com/rehabilitation-evidence/pressure-ulcers/prevention/pressure-ulcer-prevention-education-post-sci).
Mohr DC, Hart S, Vella L . Reduction in disability in a randomized controlled trial of telephone-administered cognitive-behavioral therapy. Health Psychol 2007; 26: 554–563.
Bombardier CH, Cunniffe M, Wadhwani R, Gibbons LE, Blake KD, Kraft GH . The efficacy of telephone counseling for health promotion in people with multiple sclerosis: a randomized controlled trial. Arch Phys Med Rehabil 2008; 89: 1849–1856.
Kaplan B, Farzanfar R, Friedman RH . Personal relationships with an intelligent interactive telephone health behavior advisor system: a multimethod study using surveys and ethnographic interviews. Int J Med Inform 2003; 71: 33–41.
Dallolio L, Menarini M, China S, Ventura M, Stainthorpe A, Soopramanien A et al. Functional and clinical outcomes of telemedicine in patients with spinal cord injury. Arch Phys Med Rehabil 2008; 89: 2332–2341.
Houlihan BV, Jette A, Paasche-Orlow M, Wierbicky J, Ducharme S, Zazula J et al. A telerehabilitation intervention for persons with spinal cord dysfunction. Am J Phys Med Rehabil 2011; 90: 756–764.
Stotts NA, Rodeheaver GT, Thomas DR, Frantz RA, Bartolucci AA, Sussman C et al. An instrument to measure healing in pressure ulcers: development and validation of the pressure ulcer scale for healing (PUSH). J Gerontol A Biol Sci Med Sci 2001; 56: M795–M799.
Kroenke K, Spitzer RL, Williams JB . The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001; 16: 606–613.
Sirey JA, Meyers BS, Teresi JA, Bruce ML, Ramirez M, Raue PJ et al. The Cornell Service Index as a measure of health service use. Psychiatr Serv 2005; 56: 1564–1569.
Whiteneck GG, Harrison-Felix CL, Mellick DC, Brooks CA, Charlifue SB, Gerhart KA . Quantifying environmental factors: a measure of physical, attitudinal, service, productivity, and policy barriers. Arch Phys Med Rehabil 2004; 85: 1324–1335.
Prochaska JO, Velicer WF . The transtheoretical model of health behavior change. Am J Health Promot 1997; 12: 38–48.
Bandura A . Health promotion by social cognitive means. Health Educ Behav 2004; 31: 143–164.
Hedges LV, Olkin I (eds). Statistical Methods for Meta-Analysis. Academic Press: Orlando, FL, USA. 1985.
Bloemen-Vrencken JH, de Witte LP, Post MW . Follow-up care for persons with spinal cord injury living in the community: a systematic review of interventions and their evaluation. Spinal Cord 2005; 43: 462–475.
Kairy D, Lehoux P, Vincent C, Visintin M . A systematic review of clinical outcomes, clinical process, healthcare utilization and costs associated with telerehabilitation. Disabil Rehabil 2009; 31: 427–447.
Glanz K, Shigaki D, Farzanfar R, Pinto B, Kaplan B, Friedman RH . Participant reactions to a computerized telephone system for nutrition and exercise counseling. Patient Educ Couns 2003; 49: 157–163.
Farzanfar R, Locke SE, Heeren TC, Stevens A, Vachon L, Thi Nguyen MK et al. Workplace telecommunications technology to identify mental health disorders and facilitate self-help or professional referrals. Am J Health Promot 2011; 25: 207–216.
Xu C, Jackson M, Scuffham PA, Wootton R, Simpson P, Whitty J et al. A randomized controlled trial of an interactive voice response telephone system and specialist nurse support for childhood asthma management. J Asthma 2010; 47: 768–773.
Acknowledgements
We thank Diana Pernigotti from the Gaylord Hospital in Wallingford, CT, for her enthusiastic commitment to the successful implementation of this project throughout New England; and Andrew Rossi from the Medical Information Systems Unit at Boston Medical Center for providing ongoing, reliable technical assistance. This project was made possible by funding from the Centers for Disease Control and Prevention, Grant no. 5R01DD000155, the Department of Health and Human Services; and the National Institute of Disability and Rehabilitation Research, Grant nos. H133N060024, H133N110019, and H133N120002, the Department of Education.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Dr Friedman’s work has been funded by the National Institute of Disability and Rehabilitation Research (NIDRR). Dr Friedman has stock ownership and a consulting agreement with Infomedics, the company that owns commercial rights to the TLC technology used in the computerized intervention. He is also a member of its Board of Directors. The remaining authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Houlihan, B., Jette, A., Friedman, R. et al. A pilot study of a telehealth intervention for persons with spinal cord dysfunction. Spinal Cord 51, 715–720 (2013). https://doi.org/10.1038/sc.2013.45
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2013.45
Keywords
This article is cited by
-
Barriers and facilitators to changing bowel care practices after spinal cord injury: a Theoretical Domains Framework approach
Spinal Cord (2022)
-
Self-management interventions for skin care in people with a spinal cord injury: part 2—a systematic review of use of theory and quality of intervention reporting
Spinal Cord (2018)
-
Self-management interventions for skin care in people with a spinal cord injury: part 1—a systematic review of intervention content and effectiveness
Spinal Cord (2018)
-
A feasibility pilot using telehealth videoconference monitoring of home-based NMES resistance training in persons with spinal cord injury
Spinal Cord Series and Cases (2017)
-
A Systematic Review of Telerehabilitation and mHealth Interventions for Spinal Cord Injury
Current Physical Medicine and Rehabilitation Reports (2016)