Abstract
Study design:
A retrospective study reporting specific complications of certain skin flaps for treating pressure ulcers.
Objectives:
To describe the rate and type of complications after pressure ulcer surgery in patients with spinal cord injury.
Setting:
Germany, Rheinland Pfalz.
Methods:
We collected data from 352 patients treated with 421 skin flaps to determine the rate and type of complications of each skin flap used.
Results:
In this study, we analyzed the results of 421 skin flaps in 352 patients with a total of 657 pressure ulcers from January 2006 to December 2010. Our patients had ischial, pelvic, sacral, trochanteric and lower extremity ulcers. Ischial ulcers were most common, followed by sacral and trochanteric ulcers. There were 87 complications in 421 flaps, which was an overall rate of 21%. Suture line dehiscence was the most common complication with 27 cases (31%), followed by 22 cases of infection (25.2%), 17 cases of hematoma (19.5%), 12 cases of partial necrosis (13.7%) and 9 cases of total flap necrosis (10.3%).
Conclusion:
Pressure ulcers in spinal cord-injured patients are very common and difficult and expensive to treat. The high rate of complications and the associated costs suggest the importance of evaluating the efficacy of treatment options. Conservative procedures have been standardized, but there still has been limited success in establishing guidelines on how to manage complications arising from flap surgery. Our extensive documentation of flap plastics will be useful managing complications after the surgical treatment of pressure ulcers in spinal cord-injured patients.
Similar content being viewed by others
Introduction
Pressure ulcers are one of the most common secondary conditions in spinal cord-injured patients.1 In Central Europe, there are 50 cases of pressure ulcers per 10 000 patients.2, 3 This rate is even higher in Germany where patients suffer from pressure ulcers at a rate of 10%.4 Spinal cord-injured patients are especially at risk shown by a rate of pressure ulcers of 26–60%.5 Treatment requires enormous resources and impacts on patients and care facilities greatly.
In general, the therapy of pressure ulcers is based on the localization, size, depth, age of the patient, previous surgical interventions, scars and history of infections. These variables influence the type, length and costs of a sufficient therapy. Conservative measures include the substitution of electrolytes as well as position changes.6, 7 A regular checkup is also necessary to reduce the occurrence of surface defects and the use of further resources.8
Poor management after the appearance of pressure ulcers as well as waiting too long can limit the success of conservative therapy, leading to the necessity for plastic surgery. A systematic review revealed recurrence and complication rates of 8.9 and 18.6% in musculocutaneous, fasciocutaneous and perforator-based flaps for treatment of pressure sores.9 In an 8-year study, Tavakoli et al. showed a recurrence rate of 41.4% for ischial sores in para- and tetraplegics treated with hamstring flaps.10 In the most extreme cases, such as in arterial hemorrhaging, sepsis and deep abscesses with fever and empyema in joints, emergency care is even needed.11, 12 A recent study showed that improvisation in surgical techniques leads to higher success rate for pressure ulcer healing in patients with spinal cord injury.13
The purpose of this paper was to document the rate and type of complications of skin flaps for the treatment of pressure ulcers in spinal cord-injured patients performed in our care facilities. This extensive documentation of flap plastics will be useful for surgeons in managing complications and doing quality control in the treatment of pressure ulcers in spinal cord-injured patients. Our research group is dealing with professional wound care in spinal cord-injured patients and gained good experience in their treatment.14, 15
Materials and methods
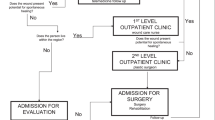
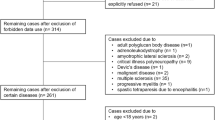
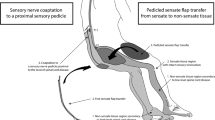
We treated 657 pressure ulcers in 352 patients with 421 flaps from January 2006 to December 2010 in the Insurance Trauma Center Ludwigshafen, Germany. Of the 352 patients involved in the study, 67 were female (19%) and 285 male (81%). All patients were spinal cord injury patients who were paralyzed either by traumatic injury (92.05%) or by other causes, such as spina bifida, multiple sclerosis, spondylodiscitis, tumors, cavernous hemangioma, Coxsackie virus, abscess or Guillan-Barré syndrome (7.95%). Patients were either completely paralyzed (76.14%, American Spinal Injuries Association (ASIA) A) or incompletely paralyzed (23.86%, ASIA B; 3%, ASIA C; Figures 1 and 2). In a follow-up, we examined 280 patients (79.5%) in intervals of 6 weeks, 6 months and 1 year after discharge. Ulcers were classified according to the National Pressure Ulcer Advisory Panel (NPUAP 2007). The size of the ulcer was also calculated and the localization was identified. Treatment involved the following flaps listed according to frequency of use: rotation flap, gluteus maximus flap (GMF), tensor fasciae latae flap (TFL), biceps femoris flap (BFF), posterior thigh flap (PTF), Conway flap, Limberg flap, total thigh flap and transverse back flap (Table 1). The following complications of these skin flaps were documented after surgery: infection, hematoma, suture line dehiscence, partial necrosis or flap failure. Data on patients were gathered retrospectively from patient records and organized regarding the type of flap used. Rates of complications per type of flap were calculated accordingly (Table 2).
Results
In this study, we analyzed the results of 421 skin flaps in 352 patients with a total of 657 pressure ulcers from January 2006 to December 2010. Our patients had ischial, pelvic, sacral, trochanteric and lower extremity ulcers. Ischial ulcers were most common, followed by sacral and trochanteric ulcers (Table 3). Most ulcers were grade IV (Table 4). Hospital stay was variable with an average of 71 days per patient. Treatment with GMFs was associated with the longest hospital stay per flap of 119 days (Table 1). Altogether, the following flaps were used: rotation flaps in 131 cases (31%); GMFs in 82 cases (19.4%); tensor fascia lata flaps (TFFs) in 77 cases (18.3%); BFFs in 55 cases (13%); PTFs in 35 cases (8.4%); Conways in 27 cases (6.4%); Limbergs in 10 cases (2.4%); transverse backs in 1 case (0.3%) and total thigh flaps in 3 cases (0.7%; Table 1).
There were 87 complications in 421 flaps, which was an overall rate of 21%. Suture line dehiscence was the most common complication with 27 cases (31%), followed by 22 cases of infection (25.2%), 17 cases of hematoma (19.5%), 12 cases of partial necrosis (13.7%) and 9 cases of total flap necrosis (10.3%; Table 5).
Suture line dehiscence was most common in PTFs and TFFs; hematoma in Limburgs and BFFs; infection in Conway flaps and PTFs; partial necrosis in TFFs and necrosis in BFFs, GMFs and TFFs. TFFs had the highest rate of complications (48.6%), that is, 17 complications in 35 flaps. Rotation flaps had the lowest rate of complications (11.5%), that is, 15 complications in 131 flaps (Table 5). In 21 patients with IV grade ulcer osteomyelitis with local infiltration was detected. The germ spectrum was very heterogeneous. Intra-operative debridement of the bone was implemented, smear tests were taken from the wound and bone parts were analyzed by the microbiology and pathology. Depending on the clinical report, the patients received a calculated antibiosis for 14 days. Infection parameters were determined on a regular basis. If there had been suspected osteomyelitis, a magnetic resonance imaging was applied. The trochanter was affected in 6 cases and the ischium in 15 cases. The wound status before closure was satisfying.
Discussion
We were able to show in our results that certain skin flaps are associated with particular complications. This is due to a number of different factors involved in the surgical preparation and implantation of skin flaps. The scientific literature points to specific factors in flap surgery that cause complications such as the separation of the flap from primary blood sources, temporary reduction in circulation and expansion of wound areas during surgery.10, 16, 17, 18, 19
The localization of pressure ulcers influences the appearance of complications, probably due to positioning and care of the ulcer following surgery. Researchers have documented the rate of complications according to pressure ulcer reconstruction localizations, and show varying results. In one of the more comprehensive studies over the last years, Schryvers et al. reported on the rate of complications of 421 flaps in 168 patients over 20 years. Authors showed that trochanteric reconstructions had the highest rate of complications (35%), followed by sacral (30%) and ischial (30%).18 However, Foster et al. reported different findings in an earlier study showing that ischial reconstructions had the highest rate of complications (42%), followed by sacral (20%) and trochanteric (15%).19
We chose not to report on the rate of complications according to reconstruction localization, because the focus of our study was on the type of flap used; however, we did show results on the occurrence of pressure ulcer localizations. We had a similar distribution of ulcer localizations in patients as Schryvers et al., who reported that 43% of patients had ischial ulcers, 20% sacral and 19.4% trochanteric.18 Our patients had 44% ischial ulcers, 22% sacral and 19% trochanteric.
Schryvers et al. grouped flaps not according to complexity, rather according to tissue type, that is, cutaneous and myocutaneous flaps.18 This made comparison with our results difficult, but we were able to confirm in our study that the most common complication was suture line dehiscence. Schryvers et al. had a total rate of complications of 31%, which was significantly higher than our rate of 21%. Forester et al. also found suture line dehiscence to be the most common complication and had a higher rate of complications of 28% in 280 skin flaps than in our study.19
Overall, the rate of complications in studies varied heavily. Alhuwalia et al. published a complication rate of 16% in 104 skin flaps.17 Another study from Srivastava et al. observed a rate of complications of 16.6% in 25 patients with 39 pressure ulcers.20 Authors had a much lower number of cases treated than we did, and did not describe how they defined complications.
The rate of complications is reflected in the length of hospital stays.21 The total hospital stay in our study was more than three times shorter as in Schryvers et al., that is, 25 104 days for 352 patients (71.3 days per patient) compared with 41 559 days for 168 patients (247.4 days per patient).18 Shorter hospital stays suggest greater efficacy of treatment and lower ensuing costs.21
There is currently no mention in the scientific literature of complications according to specific flaps. As mentioned above in relation to Schryvers et al., authors grouped complications according to type of tissue, but failed to divide these groups into specific flaps. For example, Wong et al. described the difference in complications between 18 gluteal fasciocutaneus rotational and 20 myocutaneus flaps.22 The 12-month follow-up investigation revealed that complications in the first group was 17% and in the second group 15%.22 Findings were not presented in a useful manner, because the grouping of flaps was too general. It does not account for all factors affecting the appearance of complications as discussed above. The use of specific flaps involves specific surgical procedures, which are associated with differing rates of complications. The current grouping of flaps in the presentation of complications does not provide surgeons with the necessary information for doing quality control after using a specific flap.
In order to improve on the presentation of complications, we grouped specific complications according to certain flaps. This allowed us to show that suture line dehiscence was most common in PTFs and TFFs; hematoma in Limburgs and BFFs; infection in Conway flaps and PTFs; partial necrosis in TFFs and necrosis in BFFs, GMFs and TFFs. We also gave an overall evaluation of the rate of complications for each flap, showing that TFFs had the highest rate of complications (48.6%) and rotation flaps the lowest rate of complications (11.5%; Table 5). In addition, we showed hospital stay according to flap (Table 1). The gluteus maximus flap had the longest hospital stay. Limburg and PTFs were associated with shorter stays. This form of presentation allows surgeons managing complications or doing quality control after flap surgery to compare their results easily with ours.
Our overall shorter hospital stays suggest that our treatment of complications was particularly effective in handling complications and limiting costs. We believe this can be attributed to the algorithms that we developed to treat complications of skin flaps (Figure 3). We targeted each complication with specific measures. Hematoma was drained, cleaned, samples were taken for the laboratory and then the site was closed. Necrosis was removed and later closed, but necrotic flaps were never closed directly following debridement. In cases of wound margin dehiscence, surfaces were treated conservatively and deeper defects were managed with debridement and secondary suture. Other complications such as partial flap necrosis involved necrosis removal and conservative procedures (negative pressure wound therapy). If total necrosis of the flap occurred, we removed all necrotic areas and used an alternative flap to close the wound. We have found that treatment algorithms minimize complications, improve the management of complications and overall make therapy easier, more successful and cost effective. We suggest that surgeons working with skin flaps adopt or develop consequential, standardized procedures before treating patients.
Conclusion
Because of the high rate of complications and costs of treating pressure ulcers, it is important that surgeons move forward in establishing guidelines for managing complications after flap surgery. Our evaluation of the success of specific skin flaps for treating pressure ulcers will help advance knowledge on this subject. We found that some flaps showed higher rates of overall complications than others. In addition, certain complications arose more frequently than others and were associated with certain types of flaps. The low rates of complications in comparison to other studies lead us to include our treatment algorithms as suggested therapy options. The extensive documentation of flap plastics in this study will help surgeons manage complications and do quality control after the treatment of pressure ulcers in spinal cord-injured patients.
Data Archiving
There were no data to deposit.
References
Byrne DW, Salzberg CA . Major risk factors for pressure ulcers in the spinal cord disabled: a literature review. Spinal Cord 1996; 34: 255–263.
Pelka RB . Ökonomie und Ethik—Ein Widerspruch bei chronischen Wunden. Phlebologie 1998; 27: 147–151.
Werner KG . Die Wundbehandlung in den Budgets der gesetzlichen Krankenversicherung. Aktuelle Dermatologie 1994; 20: 196–197.
Zellner PR, Meinecke F-W . Anzeigestellung und Technik verschiedener plastischer Operationsverfahren bei Druckgeschwüren. Chir Plast Reconstr 1966; 2: 16–26.
Freeman BS . The treatment of bedsores in paraplegic patients. Surgery 1947; 21: 668–674.
Kierney PC, Engrav LH, Isik FF, Esselman PC, Cardenas DD, Rand RP . Results of 268 pressure sores in 158 patients managed jointly by plastic surgery and rehabilitation medicine. Plast Reconstr Surg 1998; 102: 765–772.
Kierney PC, Cardenas DD, Engrav LH, Grant JH, Rand RP . Limb-salvage in reconstruction of recalcitrant pressure sores using the inferiorly based rectus abdominis myocutaneous flap. Plast Reconstr Surg 1998; 102: 111–116.
Farhadi J, Pierer G . Plastisch-chirurgische Konzepte zur Deckung von Dekubitalulzera (II). WundForum 2005; 1: 8–11.
Sameem M, Au M, Wood T, Farrokhyar F, Mahoney J . A systematic review of complication and recurrence rates of musculocutaneous, fasciocutaneous, and perforator-based flaps for treatment of pressure sores. Plast Reconstr Surg 2012; 130: 67e–77e.
Tavakoli K, Rutkowski S, Cope C, Hassall M, Barnett R, Richards M et al. Recurrence rates of ischial sores in para- and tetraplegics treated with hamstring flaps: an 8-year study. Br J Plast Surg 1999; 52: 476–479.
Lüscher NJ . [Decubitus ulcers of the pelvic area. Diagnosis and surgical therapy]. Aktuelle Probl Chir Orthop 1989; 33: 3–152.
Gerner HJ . Die Querschnittlähmung. Blackwell Wissenschaft: Berlin. 1992 ISBN 3-89412-070-3.
Singh R, Rohilla RK, Magu NK, Goel R, Kaur K . Improvisations in classic and modified techniques of flap surgery to improve the success rate for pressure ulcer healing in patients with spinal cord injury. Int Wound J 2012; 10: 455–460.
Biglari B, Moghaddam A, Santos K, Blaser G, Büchler A, Jansen G et al. Multicentre prospective observational study on professional wound care using honey (Medihoney). Int Wound J 2012; 10: 252–259.
Biglari B, vd Linden PH, Simon A, Aytac S, Gerner HJ, Moghaddam A . Use of Medihoney as a non-surgical therapy for chronic pressure ulcers in patients with spinal cord injury. Spinal Cord 2012; 50: 165–169.
Disa JJ, Carlton JM, Goldberg NH . Efficacy of operative cure in pressure sore patients. Plast Reconstr Surg 1992; 89: 272–278.
Ahluwalia R, Martin D, Mahoney JL . The operative treatment of pressure wounds: a 10-year experience in flap selection. Int Wound J 2010; 7: 103–106.
Schryvers OI, Stranc MF, Nance PW . Surgical treatment of pressure ulcers: 20-year experience. Arch Phys Med Rehabil 2000; 81: 1556–1562.
Foster RD, Anthony JP, Mathes SJ, Hoffman WY, Young D, Eshima I . Flap selection as a determinant of success in pressure sore coverage. Arch Surg 1997; 132: 868–873.
Srivastava A, Gupta A, Taly AB, Murali T . Surgical management of pressure ulcers during inpatient neurologic rehabilitation: outcomes for patients with spinal cord disease. J Spinal Cord Med 2009; 32: 125–131.
Assadian O, Oswald JS, Leisten R, Hinz P, Daeschlein G, Kramer A . Management of leg and pressure ulcer in hospitalized patients: direct costs are lower than expected. GMS Krankenhhyg Interdiszip 2012; 6: Doc07.
Wong TC, Ip FK . Comparison of gluteal fasciocutaneous rotational flaps and myocutaneous flaps for the treatment of sacral sores. Int Orthop 2006; 30: 64–67.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Biglari, B., Büchler, A., Reitzel, T. et al. A retrospective study on flap complications after pressure ulcer surgery in spinal cord-injured patients. Spinal Cord 52, 80–83 (2014). https://doi.org/10.1038/sc.2013.130
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2013.130
Keywords
This article is cited by
-
Standardized Pre-clinical Surgical Animal Model Protocol to Investigate the Cellular and Molecular Mechanisms of Ischemic Flap Healing
Biological Procedures Online (2024)
-
Minor microbial alterations after faecal diversion do not affect the healing process of anus-near pressure injuries in patients with spinal cord injury - results of a matched case-control study
Spinal Cord (2023)
-
Multidisciplinary treatment protocol for ischiatic, sacral, trochanteric or other pressure injuries in people with spinal cord injury: a retrospective cohort study
Spinal Cord (2023)
-
CCL-2 as a possible early marker for remission after traumatic spinal cord injury
Spinal Cord (2017)
-
Lifestyle risk factors for pressure ulcers in community-based patients with spinal cord injuries in Japan
Spinal Cord (2015)