Abstract
Study design:
Group comparison and cross-sectional study.
Objectives:
To replicate previous findings regarding electroencephalographic (EEG) pattern differences in a larger sample of patients with spinal cord injury (SCI) and chronic pain than previously studied, and examine associations between pain severity and EEG activity in a sample of patients with SCI and chronic pain.
Setting:
USA.
Methods:
EEG data were collected in an eyes-closed condition from 38 individuals with SCI and chronic pain, 16 individuals with SCI who did not have chronic pain and 28 healthy controls. Pain intensity experienced during the EEG assessment was assessed in the chronic pain group. Absolute and relative power in four frequency bands (delta, theta, alpha, and beta) were compared between the groups, and correlation coefficients between bandwidth activity and pain intensity in the pain group were computed.
Results:
Previously identified activity pattern differences (that is, more theta and less alpha) in those with SCI and chronic pain versus individuals with SCI and no pain and healthy controls were largely replicated. However, few significant associations between pain severity and EEG activity measures activity were found, and those that were found (more alpha activity associated with more pain as measured from frontal electrode sites) was in a direction opposite than predicted.
Conclusion:
The findings indicate that certain EEG activity patterns may be associated with more pain or a vulnerability to experience chronic pain in persons with SCI. Research examining the extent to which changes in this EEG activity may result in pain relief is warranted.
Similar content being viewed by others
Introduction
Many individuals with spinal cord injury (SCI) experience chronic pain that is refractory to treatment.1, 2 Research suggests that SCI-related chronic pain may be related to changes in brain activity reflected in electroencephalogram (EEG). For example, Sarnthein et al.3 compared EEG measures between 15 patients with neuropathic pain and 15 health controls. They found higher EEG activity in the patient group in the delta (2–3.5 Hz), theta (4–7.5 Hz) and beta (13–21 Hz) bandwidths. Following a neurosurgical intervention resulting in pain relief, these brain activity patterns became more like those of the healthy controls. However, in this study, the improvement in pain was frequently immediate, whereas the changes in EEG were assessed 1 year later; it is therefore not known from this study whether EEG and pain relief were closely linked.
Boord et al.4 obtained similar results in a study comparing brain EEG activity in 16 individuals with SCI (8 with neuropathic pain and 8 without pain) and 16 matched healthy controls. The patients with SCI had a lower (that is, slower) peak band frequency than the healthy controls, but this difference was only statistically significant (in 12 of 14 electrode sites) for the SCI group with pain (see also Wydenkeller et al.5). The participants with pain also had lower levels of alpha activity (when their eyes were closed), relative to those with no pain.
These studies suggest that patients with SCI and chronic pain evidence more slow wave (delta and theta) and beta activity, and less alpha activity. To the extent that these EEG differences reflect the experience of pain, then cortically directed interventions that affect EEG—including transcranial direct current stimulation and neurofeedback—may help alleviate these patients’ suffering.6
In order to know which EEG parameters to target with such treatments, more knowledge of the associations between cortical activity and pain is essential. The current study sought to replicate and increase our understanding of these associations. We expected to replicate previous findings of higher activity in EEG delta, theta and beta bandwidths, and lower activity in the alpha bandwidth, in patients with chronic pain from SCI, relative to healthy controls and relative to patients with SCI without pain. In addition, we explored the associations between EEG bandwidth activity and pain severity within a sample of patients with SCI and chronic pain.
Materials and methods
Participants
The study used three groups of patients: (1) SCI patients with pain; (2) SCI patients without pain and (3) healthy controls. Inclusion criteria for all participants were:⩾18 years old, ability to read, speak and understand English, and being free of any significant acute health conditions. SCI participants were required to have had a SCI for at least 12 months. All participants with a SCI and chronic pain must have reported (1) experiencing pain on a daily basis, (2) that their most significant pain problem was due to the SCI, (3)⩾6-month duration for their most significant pain problem and (4) average intensity of pain⩾4 on a 0–10 scale. Potential participants were excluded from participation if they reported a history of seizure activity or significant head injury, or evidenced significant skull defects (all of which could influence EEG measures) during a physical exam.
Measures
Medication use
All participants were asked to list all medications or drugs they had taken in the last 24 h before the EEG assessment. These drugs were coded as ones that might impact the EEG measures (sedatives, antidepressants, muscle relaxants, antiseizure medications, opioids and marijuana) and those that were not likely to impact EEG measures.
Pain intensity
Pain intensity experienced during the EEG recordings was assessed immediately after each session by asking the participants to rate the intensity of pain ‘during the EEG measurement on average’ using a 0–10 numerical scale, with 0=‘no pain sensation’ and 10=‘most intensity pain sensation imaginable’.
EEG recording
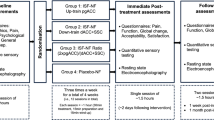
In preparation for recording, the recording sites were prepped with Nuprep (Weaver and Company, Aurora, CO, USA). An electrode cap with premeasured sites with the international 10/20 system of electrode placement was fitted to each subject (see Figure 1). Each electrode site was filled with Electrogel (Electro-Cap International, Eaton, OH, USA), and prepped to measured impedance values between each electrode site and each ear individually, as well as between the ears, to between 3 and 5 Kohms. The EEG was digitally recorded using the WinEEG (Mitsar, St Petersburg, Russia) acquisition software utilizing 19 electrodes referenced to A1 and A2 (linked ear montage).7 The input signals were amplified (bandpass 0.3–70 Hz) and sampled at the rate of 250 Hz. The EEG was recorded continuously in the awake state with eyes closed. A trained researcher monitored each subject during the recording and encouraged the subject to stay awake.
Data analysis
EEG data were exported to the EureKa! software,8 where it was re-montaged to the average reference montage, plotted and carefully inspected using manual artifact-rejection. Entire epochs of data were removed when one or more channels exhibited presence of artifact (for example, eye blinks and movements, body movements). The first 2 min of artifact-free data was used for analysis. EEG spectrum was calculated with fast Fourier transform using 2-second epochs with 1/32 s of overlapping window advancement factor. No time domain tapering for frequency domain smoothing was applied.
To test for hypothesized differences between the three groups in EEG activity within each of the bandwidths (delta, theta, alpha, beta), we performed a series of analysis of variances (ANOVAs), with absolute (reflecting overall activity that does not control for individual differences that can affect power, such as skull thickness) and relative (reflecting the amount of activity within each bandwidth divided by the overall activity measured) power within each bandwidth as the dependent variables, and group (SCI with pain, SCI without pain, healthy control) as the independent variable. We also performed exploratory ANOVAs testing for EEG activity differences at each of the 19 electrode sites to determine whether any differences in EEG activity found were global (that is, were found across all or most sites) or were linked to specific electrode sites. Finally, among the participants with pain, we computed correlation coefficients between pain intensity experienced during the assessment and both absolute and relative EEG bandwidth activity.
Statement of ethics
The study procedures were approved by a University of Washington Institutional Review Board committee, and all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed throughout the course of this research.
Results
Participants
A total of 93 potential participants met the study screening criteria and were given a physical examination. Overall, 82 of these met study inclusion criteria following the physical exam, and participated in the EEG assessment. Of these 64 had an SCI (38 with chronic pain) and 28 were healthy control subjects.
Demographic and pain type (neuropathic, nociceptive, or both) information about the study participants are presented in Table 1. The three groups did not differ significantly in age. As might be expected given spasticity and other problems in this population, many more participants with SCI than healthy controls had taken a centrally acting medication within 24 h before the EEG assessment. Also, we were able to recruit only one woman with SCI who reported no pain, which was fewer than the number of women in the SCI pain and healthy control groups. In order to ensure that any findings in the primary analyses were not influenced by the differences between groups in medication use or sex distribution, we repeated all analyses (1) using only participants with no centrally acting medications in 24 h before their EEG assessment and (2) using only men.
Group differences in absolute and relative bandwidth activity
Table 2 presents the results of the ANOVAs comparing absolute and relative EEG bandwidth activity between the groups as measured over all 19 electrode sites. A nonsignificant trend (P<0.10) emerged for differences in absolute alpha and relative theta, and a significant (P<0.05) group effect for relative alpha emerged, all of which were consistent with the study hypotheses (that is, more theta and less alpha in the SCI pain group, relative to the other groups). No significant or nonsignificant trends emerged for the delta or beta bandwidths. The analyses using only men essentially replicated these findings, with no significant effects for delta, theta or beta, but significant effects for both absolute (F(2,57)=3.50, P=0.037) and relative (F(2,57)=5.14, P=0.009) alpha. No nonsignificant trends or significant effects emerged when the analyses were limited to those not taking any centrally acting medications, although the overall pattern of findings was the same.
Electrode site exploratory analysis found no significant absolute power effects for delta, theta or beta at any site. For absolute alpha band activity, significant effects did emerge for frontal locations (FP1, FP2, F3, FZ and F4), with less alpha in the SCI pain group, relative to the other groups. No significant effects emerged for any electrode site for relative delta or beta. Nonsignificant (P<0.10) trends emerged for a number of sites for relative theta (FP1, FP2, F7, F3, FZ, C3, T5, PZ, P4), and significant (P<0.05) effects emerged for relative theta at P3, 01 and 02, with more relative theta at these sites in participants with SCI and pain, compared with the non-pain groups. Significant effects also emerged for relative alpha for 14 of the 19 electrode sites (all except F7, T3, T6, O1 and O2), with less alpha in the SCI pain group compared with the non-pain groups.
Associations between pain intensity and EEG activity
Neither absolute nor relative bandwidth power activity was associated significantly with pain intensity in the group with SCI and chronic pain (Table 3). However, the pattern of findings with respect to alpha and beta are in a direction opposite from that predicted, with higher relative and absolute alpha and lower relative beta associated with more pain intensity. Examination of the correlation coefficients at each of the 19 sites for each bandwidth yielded only three significant effects for alpha activity, and each was in a direction opposite of that predicted (that is, more alpha was associated with more pain): absolute alpha activity at FP1 (r=0.41) and FP2 (r=0.36) and relative alpha activity at F8 (r=0.39).
Discussion
This study yielded three primary findings. First, the pattern of EEG activity reported by previous investigators in patients with SCI and pain compared with individuals without pain was largely replicated in this new sample. Second, exploratory analyses suggest that the pattern of EEG activity found is not a global effect (similar over all sites), but varies as a function of electrode site. Third, contrary to our predictions, EEG activity within participants with SCI and chronic pain was not significantly associated with pain intensity; in fact, the only significant findings that emerged were for alpha activity, and these associations in the frontal regions were opposite than those predicted.
Consistent with both Sarnthein et al.3 and Boord et al.,4 and relative to individuals with SCI and no pain and healthy controls, individuals in our sample with SCI and chronic pain were found to have less alpha and more theta (although the theta finding was a nonsignificant trend, and was only observed for relative power). These patterns of activity do not appear related to sex or medication effects. Thus, the findings provide additional support that EEG activity patterns differ between individuals with SCI and chronic pain and pain-free individuals. However, the reasons that these differences exist are not yet entirely clear. Sarnthein et al.3 proposed that the differences may reflect thalamocortical dysrhythmia in persons with pain, which could be a secondary effect of SCI or other neurological disorders, and that this dysrhythmia provides a theta pacing mechanism that acts to perpetuate pain. However, the model does not explain why some individuals with SCI develop thalamocortical dysrhythmia and others do not.
A second possibility is that chronic pain affects EEG indirectly, for example by disrupting sleep patterns and/or other homeostatic mechanisms underlying normal EEG activity. If pain disrupts their sleep, then patients with pain likely experience drowsiness during a daytime eyes-closed EEG assessment (such as conducted in this study). Many of the noted EEG changes (appearance of slow theta activities and anterior shift of alpha) are known effects of drowsiness.9 Related to this, it is possible that those with pain may evidence pain behaviors (movement, forehead tension) during periods of more pain until they relax with onset of drowsiness, when they might evidence fewer artifacts. Thus, it is possible artifact-free periods (from which EEG data were computed) may be associated with more EEG activity associated with drowsy states (for example, more theta and alpha, less beta), and the EEG differences found could therefore potentially be associated with the requirement that EEG data are pulled only from artifact-free periods. Future research could examine these possibilities by examining the associations between sleep quality and measures of sleepiness, fatigue and EEG activity, and also determine whether any observed EEG changes are associated with an increased vulnerability to pain.
The correlation of higher frontal alpha frequency activity with severity of pain, which was initially unexpected (and not tested in earlier studies), is intriguing. It is particularly curious as many have suggested targeting prefrontal cortical areas or sensorimotor cortex for neurofeedback training (for example, Jensen et al.,10 Mathew et al.11, McKenzie et al.)12 due to the suspected frontal influences on pain perception (for example, Fregni et al.13). However, as mechanisms underlying and cortical generators of alpha are largely unknown, ascribing physiological significance to its anatomical distribution is speculative. Nevertheless, different anatomical patterns to alpha activity peaks are well recognized. Awake EEG with eyes closed is dominated by alpha activity over the occipital cortex (posterior dominant rhythm), and by a lesser extent central alpha frequencies of the somatosensory/motor cortex (mu rhythm).14 These background resting activities attenuate with excitation, focused attention, arousal or even drowsiness. Frontal alpha patterns are less clearly defined. As already mentioned, a frontal shift (change of the distribution of alpha activity on scalp) occurs during drowsiness at the same time that posterior dominant and central alpha attenuate. An overall alpha attenuation with a relative frontal increase with drowsiness, for example, would then be expected. Although we do not know whether drowsiness is at play in our pain subjects, this simple explanation of overall decrease in alpha with a focal relative frontal increase is at least physiologically plausible and consistent with previous pain research looking at general alpha frequencies in pain subjects.
Whether or not increased alpha is associated with drowsiness, it is also possible that because frontal brain structures may be involved in the suppression of painful sensations, an increase in frontal alpha may reflect less successful efforts in pain suppression. This possibility is consistent with the findings from tDCS studies, which seek to increase activity in the prefrontal motor cortex to facilitate pain suppression.13 This hypothesis could be tested by research examining the potential mediation effects of EEG activity on effective tDCS treatment. Specifically, we would hypothesize that successful prefrontal pain suppression may be associated with decrease in frontal alpha activity.
This study has a number of limitations that should be considered when interpreting the results. First, the sample size was relatively low (even though it was larger than those in previous studies), which can reduce our ability to detect significant effects. Second, we performed a large number of analyses without controlling for multiple tests, which increases the risk of Type I errors. However, had we controlled for alpha inflation, we would have substantially increased the risks of Type II errors. Also, the overall pattern of differences between those participants with and without pain that emerged was consistent with those found by previous researchers—a finding that would be highly unlikely had the effects been truly random.
In summary, the findings suggest that certain EEG activity patterns may be associated with more pain or a vulnerability to experience chronic pain. This finding indicates that treatments which modulate EEG activity could potentially be beneficial to individuals with chronic pain in helping them learn to regulate their experience of pain. Studies examining such interventions, and the extent to which changes in EEG activity may reflect the benefits of these treatments, are warranted.
DATA ARCHIVING
There were no data to deposit.
References
Jensen M, Hoffman AJ, Cardenas DD . Chronic pain in individuals with spinal cord injury: a survey of longitudinal study. Spinal Cord 2005; 43: 704–712.
Cardenas DD, Jensen MP . Treatments for chronic pain in persons with spinal cord injury: a survey study. J Spinal Cord Med 2006; 29: 109–117.
Sarnthein J, Stern J, Aufenberg C, Rousson V, Jeanmonod D . Increased EEG power and slowed dominant frequency in patients with neurogenic pain. Brain 2006; 129 (Part 1): 55–64.
Boord P, Siddall PJ, Tran Y, Herbert D, Middleton J, Craig A . Electroencephalographic slowing and reduced reactivity in neuropathic pain following spinal cord injury. Spinal Cord 2008; 46: 118–123.
Wydenkeller S, Maurizio S, Dietz V, Halder P . Neuropathic pain in spinal cord injury: significance of clinical and electrophysiological measures. Eur J Neurosci 2009; 30: 91–99.
Jensen MP, Hakimian S, Sherlin LH, Fregni F . New insights into neuromodulatory approaches for the treatment of pain. J Pain 2008; 9: 193–199.
Jasper HH . The ten-twenty electrode system of the International Federation. Electroencephalogr Clin Neurophysiol 1958; 10: 371–375.
Congedo M, Sherlin L . EEG source analysis: Methods and clinical implications. In: Coben R, Evans J, eds. Neurofeedback and Neuromodulation Techniques and Applications. Academic Press/Elsevier: New York. 2010, 25–46.
Santamaria J, Chiappa KH . The EEG of drowsiness in normal adults. J Clin Neurophysiol 1987; 4: 327–382.
Jensen M, Grierson C, Tracy-Smith V, Bacigalupi SC, Othermer S . Neurofeedback treatment for pain associated with Complex Regional Pain Syndrome Type I: a case series. J Neurother 2007; 11: 45–53.
Mathew A, Mishra H, Kumaraiah V . Alpha feedback in the treatment of tension headache. J Pers Clin Stud 1987; 3: 17–22.
McKenzie RF, Ehrisman WJ, Montgomery PS, Barnes RH . The treatment of headache by means of electroencephalographic biofeedback. Headache 1974; 13: 164–172.
Fregni F, Boggio PS, Lima MC, Ferreira MJ, Wagner T, Rigonatti SP et al A sham-controlled, phase II trial of transcranial direct current stimulation for the treatment of central pain in traumatic spinal cord injury. Pain 2006; 122: 197–209.
Niedermeyer E, . The Normal EEG of the waking adult. In: Niedermeyer E, Da Silva FL, (eds). Electroencephalography: Basic Principles, Clinical Applications, and Related Fields, 2005, 5th edn, Lippincott Williams and Wilkins: Philadelphia, 167–192.
Acknowledgements
This study was supported by a research grant from the Craig H Neilsen Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Jensen, M., Sherlin, L., Gertz, K. et al. Brain EEG activity correlates of chronic pain in persons with spinal cord injury: clinical implications. Spinal Cord 51, 55–58 (2013). https://doi.org/10.1038/sc.2012.84
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2012.84
Keywords
This article is cited by
-
Effects of transcranial direct current stimulation followed by exercise on neuropathic pain in chronic spinal cord injury: a double-blinded randomized controlled pilot trial
Spinal Cord (2021)
-
Spectral Power Density analysis of the resting-state as a marker of the central effects of opioid use in fibromyalgia
Scientific Reports (2021)
-
Home used, patient self-managed, brain-computer interface for the management of central neuropathic pain post spinal cord injury: usability study
Journal of NeuroEngineering and Rehabilitation (2019)
-
Spinal cord stimulation in chronic pain: evidence and theory for mechanisms of action
Bioelectronic Medicine (2019)
-
Electroencephalographic, physiologic and behavioural responses during cervical dislocation euthanasia in turkeys
BMC Veterinary Research (2019)