Abstract
Study design:
Pass-code protected web survey.
Objectives:
Defining exercise participation barrier prevalence and association with exercise participation status in adults with spinal cord injury (SCI).
Setting:
World-wide web.
Methods:
Individuals ≥18 years with ShCI in the United States completed a pass-code protected website survey (N=180). Odds ratios (OR) and OR 95% confidence interval (95% CI) assessed association between barrier presence and exercise participation.
Results:
No differences existed between exercisers and non-exercisers with respect to age, gender, injury level, injury duration, education level, or employment status. A larger percentage of non-exercisers reported household annual incomes <$7,500. The five most prevalent barriers were not associated with participation status (all OR 95% CI included 1). Low prevalence (⩽13%) characterized four of the five barriers most strongly related to being a non-exerciser. Identifying too lazy, too difficult, or no interest as a barrier decreased odds of being an exerciser by 86%, 83%, and 71%, respectively. Not liking exercise decreased the odds of being an exerciser by 90%.
Conclusion:
Highly prevalent barriers were not associated with exercise participation status, whereas low prevalence barriers were strongly related to being a non-exerciser. Internal barriers had the strongest association with exercise participation status. The possible association between socioeconomic factors and exercise participation may be underappreciated. The most effective interventions to increase exercise participation may be multifocal approaches to enhance internal perceptions about and motivation to exercise, increase knowledge of how and where to exercise, while also reducing program and transportation financial costs.
Similar content being viewed by others
Introduction
Low-exercise rates among persons with disabilities1 are partly attributed to both real and perceived barriers2 to exercise participation. Some barriers are common to persons with and without disabilities, including time constraints, lack of internal motivation, and lack of knowledge of what to do.3 However, persons with mobility disabilities experience added challenges, such as locating facilities with accessible exercise equipment, lack of disability aware fitness professionals, and needing accessible facilities to shower post-exercise.
Few studies have attempted to identify perceived barriers to exercise in the spinal cord injury (SCI) population. However, mixed disability focus groups have revealed 10 major groups of exercise participation barriers and facilitators: environmental, cost, equipment, laws and regulations, information, psychosocial, education and training, perceptions and attitudes, policies and procedures, and resource availability. In 72 adults with SCI, Scelza et al.4 narrowed these to three primary categories of perceived exercise barriers: internal (lack of motivation, energy, interest, and so on); resources (cost, knowledge, and so on); and structural (accessibility and so on). Another small SCI study (N=26) utilized semi-structured phone interviews to identify participant’s experiences with exercise as well as barriers and facilitators to being active.5 In that study, the authors emphasized the interdependent relationship between internal motivational triggers/constraints and external socio-environmental resources/barriers in determining exercise participation.
The importance of understanding exercise participation barriers as a precursor to developing effective interventions and limited results of previous research justify a larger study to investigate the issue in more depth. We thus conducted a web-based survey of the United States SCI population. This survey was based on the original B-PED6 and the modified B-PED,3 with additional modifications to increase the amount of information obtained. Our purpose was to describe exercise perceptions, define exercise barrier prevalence, and identify which barriers and perceptions are associated with exercise participation status (exerciser vs non-exerciser) in a large sample of adults dwelling in the United States.
Materials and methods
Survey Design
A questionnaire acquired information about barriers to exercise participation from persons living with SCI in the United States. The questionnaire was divided into three sections: (1) demographics and current health, (2) independence level, and (3) exercise. The exercise section was a modified version of the B-PED (modified in that 11 questions were added to the existing 31 questions, see highlighted questions in Supplementary Material). The B-PED demonstrates inter-rater reliability (Cohen’s κ 0.86) and test–retest stability (κ 0.76)6 and was designed to be administered by telephone or personal interview. Except for the final open ended question, answers were limited to pre-defined choices to standardize responses. All survey questions and answer choices are available in the Supplementary Material.
The study was approved by the University of California, Irvine, Institutional Review Board. We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Participant Recruitment
Eligibility requirements included age of 18 years or older, a permanent SCI of any cause or severity, and living in the United States. Advertisements were placed on multiple SCI websites, online support groups, SCI bulletin boards, and mailing lists. Eligible subjects contacted the principal investigator to receive a randomly generated pass-code for entry into the secure website. Upon completion of the survey, this pass-code was unlinked from survey responses, thereby preserving anonymity. Individuals interested in participating who did not have internet access could request a paper version to complete and return to the principal investigator. Subjects were enrolled during an 18-month period. An exercise program was defined for the participants as, ‘… some type of structured activity that is done on a regular basis such as walking, standing, lifting weights, doing aerobics, resistance training, or riding a stationary bike (for arms or legs).’ This was the exact definition used in the initial B-PED.6
Statistical Analyses
All analyses were performed using SPSS (SPSS, Chicago, IL, USA). To describe the overall exerciser subset and non-exerciser subset, demographics, and questionnaire responses, means, s.d., and percentages were computed as befitted the data type. Exercisers were those answering yes to the B-PED question, ‘Are you currently participating in an exercise program.’ Non-exercisers answered no. Differences between exercisers and non-exercisers for demographics, exercise preferences, and individual and total perceived exercise barriers were identified using χ2, Mann–Whitney U, and independent t-tests as befitted the data. To identify if exercise preferences and barriers were related to exercise status (exerciser vs non-exerciser), we computed odds ratios (OR) and OR 95% Confidence Intervals (95% CI) for each factor that differed between exercisers and non-exercisers. Preferences and barriers with OR 95% CI not containing 1.00 were accepted as related to exercise status. For factors related to exercise status, we computed how strongly that factor decreased the odds of being an exerciser ((1−OR) × 100). This provides a clearer visualization of the association strength between a barrier and current exercise participation status. Significance was set a priori at α<0.05, with trends accepted at α<0.10.
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Results
One hundred eighty five surveys were completed, of which five were discarded as inadvertent duplicate completions, leaving 180 for analysis. Overall, our sample was predominantly middle aged (46±11), white (87%), male (63%), with paraplegia (56%), and had been injured at least a decade (14±11). There were 115 individuals who stated they were currently exercising (exercisers) and 65 individuals who stated they were not currently exercising (non-exercisers). There were no differences between exercisers and non-exercisers for age, gender, injury level, injury duration, education level, employment status, or marital status (Table 1). A trend existed for a greater percentage of non-exercisers to be African-American (P=0.05). The sole income difference between exercisers and non-exercisers was a greater percentage of non-exercisers reporting household annual incomes<$7,500.
Perceived barriers
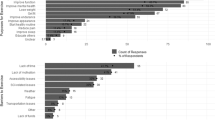
There was no overlap between the five most prevalent barriers and the five barriers most strongly associated with exercise status (Table 2). In the full sample, the five most prevalent perceived barriers were: (1) lack of energy, (2) lack of motivation, (3) lack of time, (4) not knowing where to exercise, and (5) the cost of the program (Table 2). Nine of the 14 barriers were more prevalent among non-exercisers (Table 2). The five most strongly associated barriers were: (1) exercise will make your condition worse, (2) too lazy to exercise, (3) exercise is too difficult, (4) do not know how to exercise, and (5) lack of interest. Finally, the total number of perceived barriers tended to be higher among non-exercisers vs exercisers (mean±s.d. 4.4±2.5 vs 2.5±2.0, P<0.001, Mann–Whitney U).
Exercise perceptions
More than 80% of all participants indicated that exercise was important to them and believed an exercise program could help them (Table 2). However, persons who did not ‘like’ exercise or reported it as ‘not important’, were 84% and 90%, respectively, less likely to be exercisers (Table 2). These findings are similar in magnitude to those of the perceived barriers ‘too lazy to exercise’ and ‘exercise is too difficult’.
Exercise participation
More than half of respondents were currently exercising, but more than two-thirds were exercising less than before their injury. Among the 36% who were not currently exercising (N=65), 86% wanted to start exercising. Thus, 95% were either exercising or interested in starting exercise. However, while more than half reported their physician had advised them to exercise, less than a quarter had received specific instructions from their doctor regarding the kind of exercise to engage in or how often.
Exercise facilities and transportation
Over half of our participants had exercise equipment at home and nearly all reported using it. Not having exercise equipment at home reduced the odds of being an exerciser by 68% (Table 2). Although nearly all had access to transportation, only 57% knew of an accessible fitness center in their area. Lack of transportation did not decrease the odds of being an exerciser, but not knowing of an accessible fitness center did. While 54% felt welcome at a traditional fitness facility, only 12% felt an instructor at such places would know how to help them.
Exercise facility and transportation related financial costs
Most respondents reported being able to pay up to $5 per trip 2–3 times per week for transportation to a fitness facility and most reported being able to pay $25 a month to join a fitness facility. However, the ability to pay these amounts was more commonly reported among exercisers, with the inability to pay decreasing the odds of being an exerciser. Not being able to afford the fitness facility fee more strongly decreased the odds of being an exerciser than not being able to afford transportation.
Discussion
Facilitating an increase in exercise participation rates in the SCI community requires an understanding of not only barrier prevalence, but also how barriers are related to exercise participation status (for example, exerciser or non-exerciser). Our results suggest that barrier prevalence may not be indicative of whether a barrier is associated with exercise status. Highly prevalent barriers may not decrease the odds of being an exerciser, while very uncommon barriers may strongly decrease the odds of being an exerciser. Our results further suggest internal barriers, followed by resource barriers, are most strongly related to exercise participation status. This supports previous qualitative work in an SCI cohort7 as well as quantitative work in mixed disability groups.5
Previous work examining exercise participation barriers among persons with SCI has focused on the topic of barrier prevalence.4 An instinctive application of this work is to focus intervention efforts on reducing prevalence of the most common barriers. However, our results suggest that intervention-minded researchers and clinicians should be cautious as to which barriers they target, as barrier prevalence does not appear to index if and by how much a barrier decreases the odds of being an exerciser. Among the five most prevalent barriers, two barriers (lack of time and lack of energy) were not associated with exercise status and three were moderately related (lack of motivation, cost of program, and do not know where to exercise). In contrast, the three barriers most strongly associated with participation status, too lazy to exercise, exercises is too difficult, and lack of interest, had low prevalence rates. Our recommendation for globally improving participation would be to target aspects related to knowledge and cost of program. These barriers have moderate prevalence and strong associations, are resource-related, and have concrete, measureable outcomes. In contrast, altering a person’s perception about themselves and exercise requires a more individualized approach and may thus be cost prohibitive.
Intuitively, we anticipated resource or structural factors would strongly reduce the odds of being an exerciser. However, this assumption was not supported by our data. Examination of Table 2, section A, clearly indicates that four of the five perceived barriers most strongly related to exerciser status are of an internal nature. The relative importance of internal barriers is further supported by our data, which demonstrate that exercise perceptions (that is, not liking exercise, not valuing exercise, and not feeling it could help you) reduce the odds of being an exerciser by a greater amount than resource or structural barriers (that is, lack of in home exercise equipment or inability to pay for transportation or facility). Our proposal that internal barriers may be the most important supports previous qualitative work by Kehn and Kroll.7 They reported that among persons with SCI, non-exercisers and exercisers identified presence or lack of motivation as the most critical factor to being active. They further reported that exercisers anticipated a greater number and type of health and functional benefits from regular exercise than non-exercisers.
The majority of work examining correlates or predictors of exercise status or physical activity levels in SCI has centered on SCI-related factors, for example, injury level,4 injury completeness,8 ambulatory status,4 and so on. In contrast, the possible importance of sociodemographic factors is far less examined. Kehn and Kroll7 suggested that sociodemographic and/or economic factors, that is, income and education, can attenuate or exacerbate SCI-imposed exercise participation barriers.7 Our results support this belief, and specifically indicate that annual household income may be related to exercise participation among persons with SCI. The relationship between income and exercise status was only present at very low annual incomes, with a greater percentage of non-exercisers reporting extremely low annual incomes (<$7,500). Additional study is required to better define the undoubtedly complex and subtle relationship between sociodemographic factors, SCI-related factors, motivational triggers,7 and exercise barriers.
We thus suggest that the strongest determinate of exercise participation may be the relative balance between internal facilitators/barriers and external facilitators/barriers, rather than the absolute levels of either. We propose that persons with fewer internal barriers may be willing and able to devise solutions to overcome or accommodate a greater number of external barriers. This is supported by the qualitative work of Kehn and Kroll,7 who suggest that physical activity levels are contingent on a combination of motivational and socio-environmental factors. We suggest that the next generation of interventions to enhance exercise participation rates in the SCI community should consider a three prong approach focusing on augmenting internal motivation in conjunction with increasing knowledge of how and where to exercise, while reducing exercise participation costs.
Potential sample bias and study limitations,
Our findings must be interpreted cautiously with regard to known sample biases and study limitations. Our sample was drawn exclusively from the United States and was predominantly white, affluent, well-educated, and employed. We therefore acknowledge our results and conclusions may not reflect samples drawn from other countries, minorities, lower incomes, and the unemployed. In addition, because our survey was web based, our sample is biased towards persons who frequent the internet. Finally, our primary recruitment avenues were SCI-focused organizations, thus our findings may not accurately represent persons who do not interact with such organizations.
Additionally, we advise readers of limitations to our analytic approach. First, all analyses are based on the response to the question about current exercise participation, which had a yes or no answer. We do not know at which stage subjects were within an exercise program (early adoption, maintenance, etc.), which could influence their view of barriers. Second, the cross-sectional nature of this study precludes causation determination. OR are a calculation of association, not causation. Third, we provided percent decrease in odds of being an exerciser as more intuitive visualization than OR of how strongly a given barrier is related to exercise participation status, because it is derived from OR, it measures association, not causation. Finally, the substantial overlap among OR 95% CI of barriers associated with being a non-exerciser means the rank order of these barriers may differ in future studies, especially given the heterogeneity of the SCI population.
Data archiving
There were no data to deposit.
References
Percent of adults who engage in aerobic physical activity of at least moderate intensity for at least 150 or 75 min/week of vigorous intensity, or an equivalent combination. Health Indicators Warehouse October 4 2011 Available from: URL http://healthindicators.gov/Indicators/Aerobic-physical-activity-150-minweek-moderate-or-75min/week-vigorous-physical-activity-percent_1319/National_0/Profile/Data.
Rimmer JH, Riley B, Wang E, Rauworth A, Jurkowski J . Physical activity participation among persons with disabilities: barriers and facilitators. Am J Prev Med 2004; 26: 419–425.
Sherwood NE, Jeffery RW . The Behavioral determinants of exercise: implications for physical activity interventions. Ann Rev Nutr 2000; 20: 21–44.
Scelza WM, Kalpakjian CZ, Zemper ED, Tate DG . Perceived barriers to exercise in people with spinal cord injury. Am J Phys Med Rehabil 2005; 84: 576–583.
Kinne S, Patrick DL, Maher EJ . Correlates of exercise maintenance among people with mobility impairments. Disabil Rehabil 1999; 21: 15–22.
Rimmer JH, Rubin SS, Braddock D . Barriers to exercise in African American women with physical disabilities. Arch Phys Med Rehabil 2000; 81: 182–188.
Kehn M, Kroll T . Staying physically active after spinal cord injury: a qualitative exploration of barriers and facilitators to exercise participation. BMC Public Health 2009; 9: 168.
Ginis KA, Latimer AE, Arbour-Nicitopoulos KP, Buchholz AC, Bray SR, Craven BC et al. Leisure time physical activity in a population-based sample of people with spinal cord injury part I: demographic and injury-related correlates. Arch Phys Med Rehabil 2010; 91: 722–728.
Acknowledgements
The authors thank Stanley Lee, responsible for survey website design and maintenance, and Thuy Pham, for recruitment assistance. The study was funded by the National Institute for Disability and Rehabilitation Research (NIDRR-# H133G080150) and the Reeve-Irvine Research Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Spinal Cord website
Supplementary information
Rights and permissions
About this article
Cite this article
Cowan, R., Nash, M. & Anderson, K. Exercise participation barrier prevalence and association with exercise participation status in individuals with spinal cord injury. Spinal Cord 51, 27–32 (2013). https://doi.org/10.1038/sc.2012.53
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2012.53
Keywords
This article is cited by
-
Perceptions of a self-guided web-based exercise programme for shoulder pain after spinal cord injury: A qualitative study
Spinal Cord (2023)
-
Association between weekly exercise minutes and resting IL-6 in adults with chronic spinal cord injury: findings from the fracture risk after spinal cord injury exercise study
Spinal Cord (2022)
-
Qualitative analysis of perceived motivators and barriers to exercise in individuals with spinal cord injury enrolled in an exercise study
Spinal Cord Series and Cases (2022)
-
The Spinal Cord Injury Program in Exercise (SCIPE) study: study protocol for a randomized controlled trial evaluating teleexercise programs for people with spinal cord injury
Trials (2021)
-
A tele-health intervention to increase physical fitness in people with spinal cord injury and cardiometabolic disease or risk factors: a pilot randomized controlled trial
Spinal Cord (2021)