Abstract
Study design:
A retrospective chart review.
Objectives:
To evaluate different methods of estimating renal function compared with patient-specific vancomycin and aminoglycoside (AG) clearance (CLDRUG) in patients with spinal cord injury (SCI), and to develop a new equation to more accurately estimate glomerular filtration rate (GFR) in SCI patients in order to optimize dosing for vancomycin and AG.
Setting:
Veterans Affairs medical center in California, United States of America, tertiary care facility with the largest inpatient SCI center in the VA system.
Methods:
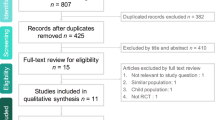
Retrospective data collection from patient records. Pharmacokinetic analysis was performed to obtain actual CLDRUG, which is compared with different methods of estimating GFR.A total of 310 patients were initially assessed; however, only 141 patients met the inclusion criteria, had a diagnosis of chronic SCI, and received vancomycin or AG with at least one drug level at steady state from January to December of 2008.
Results:
All four equations evaluated to estimate GFR significantly overestimated CLDRUG: the Modification of Diet in Renal Disease equation by 141%, Cockcroft–Gault equation by 83%, Chronic Kidney Disease Epidemiology Collaboration equation by 82% and 24-h endogenous creatinine clearance by 71% (P<0.001). The modified Cockcroft–Gault equation (CLM) showed improvement, however, still overestimated CLDRUG by 39% (P<0.001). Thus, a new equation for SCI (CLSCI) was developed which underestimated CLDRUG by <5% (P=0.16).
Conclusion:
Compared with different methods of estimating GFR, CLSCI=2.3 × x0.7 (x equals CLM in ml min−1) more accurately estimates CLDRUG in chronic SCI patients.
Similar content being viewed by others
Introduction
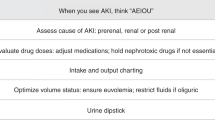
It is crucial to renally adjust medications that are eliminated primarily by the kidneys in order to avoid toxicity and/or decrease incidence of adverse drug reactions. Cockcroft–Gault creatinine clearance (CLCG) has been exclusively used to estimate glomerular filtration rate (GFR) based on serum creatinine (SCr) to calculate dosing regimens for renally cleared medications including vancomycin and aminoglycosides (AG). However, CLCG may not extrapolate to patients with spinal cord injury (SCI) because the Cockcroft and Gault (CG) study excluded 31 patients with 24-h creatinine excretion <10 mg kg−1, and it did not reveal whether the study population included SCI patients and to what extent.1 Furthermore, CG reported that creatinine excretion in paraplegics was as much as 40% lower than predicted.1 Likewise, other studies have found that patients with SCI have significantly low SCr, therefore, CLCG is overestimated.2, 3, 4 Such findings may be because of reduced creatinine production caused by diffuse muscle atrophy and persistent immobility. Overestimation of GFR results in dosing renally cleared medications higher than recommended, and this could lead to supratherapeutic vancomycin and AG serum levels leading to adverse drug effects and/or toxicity.5, 6, 7 In the nephrology arena, a more recently developed equation, the Modification of Diet in Renal Disease equation (MDRD), has been widely used to estimate GFR.8, 9 Moreover, a new equation, the Chronic Kidney Disease Epidemiology Collaboration equation (CKD-EPI), has been proposed to more accurately estimate GFR compared with MDRD.10 However, data on the application of MDRD in pharmacokinetic dosing of vancomycin and AG are inconsistent, while there is no data to date on CKD-EPI.11, 12, 13, 14
The objectives of this study are: (1) to evaluate different methods of estimating GFR compared with patient-specific vancomycin and AG drug clearance (CLDRUG) in SCI patients, (2) to assess whether there is a difference in the estimation of renal function between anatomical degrees of SCI when compared with CLDRUG and (3) to develop a new equation to more accurately estimate GFR in SCI patients in order to optimize dosing for vancomycin and AG.
Materials and methods
This study was a retrospective chart review, and the protocol was reviewed and approved by the institution's institutional review board.
All patients with a diagnosis of chronic SCI (defined as duration of injury >1 year) at a Veterans Affairs medical center, who received tobramycin, gentamicin, amikacin, or vancomycin with at least one drug level at steady state from January 2008 to December 2008, were evaluated for enrollment in this study. Patients were excluded from the study if they had a limb amputation, received dialysis treatment, experienced changing of renal function (defined as >20% or ⩾0.3 mg dl−1 change in SCr concentration), had a history of SCI <1 year, had diagnosis of multiple sclerosis, their antibiotic doses had not been administered or charted, their drug levels had not been at steady state (defined as at least 4 half-lives), or if the drug levels had been reported as below the sensitivity of the assay.
Patient demographics, degree of SCI, vancomycin and AG administration records, sampling times, SCr concentrations and 24-h endogenous creatinine clearance (CL24H) were obtained and recorded. Method of bladder emptying was documented, and 24-h urine was collected according to Lippincott's nursing procedures and skills.15 The dose of vancomycin was infused over ∼60 min and AG over 30 min. AG peak drug concentration was measured at least 30 min after the infusion was completed, and AG and vancomycin trough generally within 1 h before the end of the dosing interval. Ideal body weight (IBW) was determined by using the method of Devine.16 Patient-specific vancomycin volume of distribution (Vd) was calculated using the Rushing and Ambrose method.17 Empiric vancomycin clearance and AG clearance are equal to the estimated creatinine clearance (CLCR), according to the method described by CG.1 Estimation of pharmacokinetic parameters of vancomycin and AG was made using a one-compartment open model. Patient-specific Vd and CLDRUG were determined from the measured serum levels using the method of Sawchuk et al.18
The formulas can be described as follows:
Adjusted body weight=IBW+0.4 (actual weight–IBW)
Rushing and Ambrose method: Vd (L)=0.17 (age)+0.22 (actual body weight in kg)+15
4-Variable MDRD=175 × standardized SCr−1.154 × age−0.203 × 1.212 (if black) × 0.742 (if female)
CKD-EPI=141 × min (SCr/k, 1)α × max (SCr/k, 1)−1.209 × 0.993Age × 1.018 (if female) × 1.159 (if black), where k is 0.7 for females and 0.9 for males, α is −0.329 for females and −0.411 for males, min indicates the minimum of SCr/k or 1, and max indicates the maximum of SCr/k or 1.
CL24H (ml min−1)=[urine creatinine × urine volume (ml)]/[SCr × time (h) × 60]
CLCG (ml min−1)=[(140–age) × IBW in kg]/(72 × SCr); (multiply 0.85 for females)
Modified CG formula (CLM) (ml min−1)=[(140–age) × IBW in kg]/(72 × SCr); (multiply 0.85 for females); (SCr rounded to 1 mg dl−1 for patients with SCr <1 mg dl−1 while using the actual SCr for patients with SCr⩾1 mg dl−1).
CLDRUG is compared with each of the different methods of estimating GFR:
-
1
MDRD.
-
2
CKD-EPI.
-
3
CL24H using standard collection techniques.
-
4
CLCG.
-
5
CLM.
-
6
A new equation for SCI (CLSCI).
Using Microsoft Excel 2007, a best-fit line between CLDRUG and the method closest to estimating GFR was obtained to determine CLSCI that would better predict CLDRUG. Analyses between CLDRUG and each of the different methods to estimate GFR were conducted using independent two-tailed t-tests, with an alpha level of 0.01 and 95% power. The calculated CLCR determined by CLSCI was correlated with the values obtained by pharmacokinetic analysis of actual drug levels using standard linear regression analysis (Pearson product-moment correlations, r).
Results
The patient characteristics are presented in Table 1. There were no patients on gentamicin or tobramycin who met the inclusion criteria, as amikacin is the primary AG at the study institution. The study population almost entirely used an aid of bladder retention catheter for 24-h urine collection: 75% had indwelling catheters, 20% external condom catheters, 2% ileal conduit and 3% reflex voiding.
Table 2 presents evaluation of different methods to estimate GFR compared with CLDRUG. The data demonstrates that all methods overestimate CLDRUG (<0.001). The mean difference between CLDRUG and MDRD is largest where overestimation by MDRD is ∼140%. Figure 1 depicts the difference between MDRD and CLDRUG. A total of 32% (45 of 141 patients) had estimated clearance from MDRD within ±30 ml min−1 of CLDRUG. On the other hand, 67% (95 of 141) of the patients had overestimation of clearance by ⩾30 ml min−1 when using MDRD to predict empiric dosing for vancomycin and AG (P<0.001). Levey et al.10 demonstrated that CKD-EPI was less biased and more accurate than MDRD. Likewise, our findings showed that estimated GFR by CKD-EPI was closer to CLDRUG than MDRD (Table 2). Despite this, CKD-EPI significantly overestimated CLDRUG by more than 80%. Compared with MDRD, CLCG, CKD-EPI and CL24H, CLM showed better prediction of CLDRUG. A total of 66% (93 of 141 patients) had estimated clearance from CLM within ± 30 ml min−1 of CLDRUG (P<0.001) (Figure 2). In all, 1% (2 of 141) of the patients had underestimation of clearance whereas 33% (46 of 141) of the patients had overestimation of clearance by ⩾30 ml min−1, when using CLM to predict empiric dosing for vancomycin and AG (P<0.001) (Figure 2). In spite of substantial improvement by modification of the existing CG formula, CLM significantly overestimated CLDRUG by ∼40%.
Table 3 presents evaluation of CLM to estimate CLDRUG for vancomycin and AG separately. The mean difference between CLM and CLDRUG for combined amikacin and vancomycin groups is 19.61 ml min−1 (P<0.001) where CLM overestimated CLDRUG by ∼20 ml min−1. However, when the groups are separated, the mean difference between CLM and CLDRUG for amikacin group is 12.1 ml min−1 (P=0.033), while the difference for vancomycin is 21.81 ml min−1 (P<0.001). As the mean difference between the predicted and actual clearance for amikacin group was statistically insignificant and included 32 of 141 patients, only the vancomycin group was used to develop a new SCI equation for estimating GFR.
Figure 3 depicts plots of patient-specific CLDRUG based on pharmacokinetic level analysis versus CLM for the vancomycin group. In order to improve CLM's ability to predict CLDRUG, the best-fit line is drawn between the two and expressed by the equation y=2.3 × x0.7 where x equals CLM and y equals CLDRUG in ml min−1. This newly developed SCI equation (CLSCI) may better predict CLDRUG based on CLM. Figure 4 presents linear regression plots of CLDRUG versus CLSCI. The regression equation found is y=0.8425x+6.7281 (r=0.4, P-value <0.001), where x equals CLSCI, y the CLDRUG and r the correlation coefficient. The dotted line in Figure 4 represents a line with a slope of 1 that indicates a perfectly one-to-one association between CLSCI and CLDRUG. The point where the dotted line and regression line meet is 43 ml min−1. CLSCI <43 ml min−1 may overestimate CLDRUG whereas CLSCI >43 ml min−1 may underestimate CLDRUG. The mean difference between CLSCI and CLDRUG for the vancomycin group is −2.35 ml min−1 where CLSCI underestimates CLDRUG by ∼5%, however, there is no statistical significance (P-value=0.16).
Table 4 illustrates evaluation of methods to predict CLDRUG for different anatomical degrees of SCI. The mean difference between CLSCI and CLDRUG was not statistically significant when separated into paraplegics and tetraplegics. Similar finding was noted for CLM and CL24H. On the contrary, the mean differences between CLCG, CKD-EPI, and MDRD and CLDRUG were statistically significant between the two anatomical degrees of SCI where tetraplegics had a gross overestimation of CLDRUG compared with paraplegics.
Discussion
SCr is used to estimate the dose of potentially toxic drugs eliminated primarily by the kidneys. SCI patients have significantly lower SCr compared with non-SCI patients due to immobility and muscle atrophy. In this study, MDRD was found to significantly overestimate CLDRUG by more than two times higher than the actual on average. This could result in supratherapeutic vancomycin and AG peak, and trough levels where potential for nephrotoxicity and/or ototoxicity could drastically increase. This could be devastating to many SCI patients who have existing renal insufficiency.
MDRD was derived from a study of relatively young population (mean age 51±13 years) with chronic kidney disease, primarily to stage kidney disease. The data on its use specifically for drug dosing are scarce and inconsistent. A study by Bookstaver et al.14 reported that MDRD performed better than CLCG in estimating AG clearance. On the other hand, a more recent study done by Ryzner11 found that CLCG correlated better with actual AG clearance compared with MDRD. The results from our investigation are consistent with that of the Ryzner where the mean difference between CLCG and CLDRUG was smaller than the difference between MDRD and CLDRUG (P<0.001).
In 2009, Levey et al.10 stated that clinicians should be aware of limitations of all creatinine-based equations in patients with extremely low muscle mass. The serum concentration of creatinine is greatly influenced by muscle mass, and all equations evaluated in this study include SCr to a various degree. Although some equations attempt to capture the difference in creatinine production by age, weight, gender and/or race, they do not capture all factors, especially SCI. Consequently, using such equations in SCI patients with significantly reduced muscle mass and SCr would result in considerable overestimation of GFR.
Despite overestimation, CLM was closest to CLDRUG. Compared with 50% (70 out of 141) of patients with estimated GFR from MDRD, only 1 out of 141 patients with estimated GFR from CLM was found to have CLDRUG overestimated by ⩾60 ml min−1. Hence, an adjustment was made to the CLM equation to further improve dosing for vancomycin in SCI patients.
The line of best fit between CLM and CLDRUG was drawn in this study.
The newly developed SCI equation for estimating CLDRUG is expressed as the following:
CLSCI (ml min−1)=2.3 × x0.7, where x equals CLM.
This may better estimate actual vancomycin clearance; thus, optimize dosing for vancomycin in SCI patients. According to the regression equation y=0.8425x+6.7281 (r=0.4, P-value <0.001), there is close to one-to-one association between CLSCI and CLDRUG with moderate correlation. CLSCI may slightly underestimate CLDRUG, however, there is no statistically significant difference between the two.
Compared with paraplegics, tetraplegics had a gross overestimation of CLDRUG when using CLCG, CKD-EPI and MDRD to estimate CLDRUG (P<0.001). This may be due to higher extent of muscle atrophy and immobility in tetraplegics resulting in lower SCr. As all three equations have SCr in the denominator, estimated GFR would be higher in tetraplegics. On the other hand, there was no statistically significant difference between the two groups when using CLM and CL24H to estimate CLDRUG. As both equations either round SCr up to 1 mg dl−1 for patients with SCr <1 mg dl−1 or use a ratio of urine creatinine to SCr, lower SCr in tetraplegics may have been blunted.
This study has several limitations. The AG group had only 32 amikacin patients. Hence, there is not enough power to determine statistical significance to analyze amikacin group separately from that of the vancomycin, and the data may not be generalized to gentamicin and tobramycin. The study was conducted in a veterans population, with nearly all male (99%) of advanced age (mean 66 years), thus, the data might not extrapolate to other populations with SCI. Although CG mentions the use of the aid of bladder retention catheter in paraplegics, the study does not mention whether the catheter was the sole method of bladder emptying. If there is a significant difference in the bladder emptying methods between this study, which had <3% of patients who had spontaneous voiding, and that of the CG, assessment of CL24H could be inaccurate. Other limitations include the variability inherent in using clinical data, assumption that both AG clearance and vancomycin clearance equal CLCR, and the assumption that the equations used to calculate Vd are accurate in our study population. It is recommended that laboratories report GFR as >60 ml min−1 instead of the actual value.19 In this study, we reported the actual values obtained by MDRD and CKD-EPI to evaluate the study outcome. In addition, the abbreviated form of MDRD was used in this study. Finally, our study did not adjust the equations including CLCG for body surface area. This is consistent with the recommendation by the National Kidney Disease Education Program that does not recommend routine adjustment for body surface area.20
Despite these limitations, this study suggests that compared with different methods of estimating GFR, CLSCI=y=2.3 × x0.7 more accurately estimates GFR to dose vancomycin, thus, achieving serum levels closer to goal in chronic SCI patients.
References
Cockcroft DW, Gault MH . Prediction of creatinine clearance from serum creatinine. Nephron 1976; 16: 31–41.
Macdiarmid SA, Mcintyre WJ, Anthony A, Bailey RR, Turner JG, Arnold EP et al. Monitoring of renal function in patients with spinal cord injury. BJU Int 2000; 85: 1014–1018.
Mirahmadi MK, Byrne C, Barton C, Penera N, Gordon S, Vaziri ND et al. Prediction of creatinine clearance from serum creatinine in spinal cord injury patients. Paraplegia 1983; 21: 23–29.
Lawrence AL, Davis RL . Vancomycin pharmacokinetics in spinal cord injured patients: a comparison with age-matched, able-bodied controls. J Spinal Cord Med 1995; 16: 233–235.
Rybak M, Lomaestro B, Rotschafer J, Moellering Jr R, Craig W, Billeter M et al. Therapeutic monitoring of vancomycin in adult patients: a consensus review of the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, and the Society of Infectious Diseases Pharmacists. Am J Health-Syst Pharm 2009; 66: 82–98.
Hidayat L, Hsu D, Quist R, Shriner KA, Wong-Beringer A . High-dose vancomycin therapy for methicillin-resist staphylococcus aureus infections: efficacy and toxicity. Arch Intern Med 2006; 166: 2138–2144.
Kahlmeter G, Dahlager JI . Aminoglycoside toxicity—a review of clinical studies published between 1975 and 1982. J Antimicrob Chemother 1984; 13: 9–22.
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D . A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Ann Intern Med 1999; 130 (6): 461–470.
Stevens LA, Coresh J, Feldman HI, Greene T, Lash JP, Nelson RG et al. Evaluation of the modification of diet in renal disease study equation in a large diverse population. J Am Soc Nephrol 2007; 18: 2749–2757.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro III AF, Feldman HI et al. A new equation to estimate glomerular filtration rate. Ann Intern Med 2009; 150: 604–612.
Ryzner KL . Evaluation of aminoglycoside clearance using the modification of diet in renal disease equation versus the cockcroft-gault equation as a marker of glomerular filtration rate. Ann Pharmacother 2010; 44: 1030–1037.
Roberts GW, Ibsen PM, Schioler CT . Modified diet in renal disease method overestimates renal function in selected elderly patients. Age Ageing 2009; 38: 698–703.
Probst LA, Darko W, Smith A . Pitfalls of the application of the modification of diet in renal disease equation to drug-dosing practice: a tertiary care teaching hospital experience. Hosp Pharm 2008; 43 (7): 564–570.
Bookstaver PB, Johnson JW, McCoy TP, Stewart D, Williamson JC . Modification of diet in renal disease and modified Cockcroft-Gault formulas in predicting aminoglycoside elimination. Ann Pharmacother 2008; 42: 1758–1765.
12- or 24-hour timed urine collection. (2010) Lippincott's Nursing Procedures and Skills. Retrived November 16, 2010, from http://www.procedures.lww.com.
Devine BJ . Gentamicin therapy. Drug Intell Clin Pharm 1974; 8: 650–655.
Rushing TA, Ambrose PJ . Clinical application and evaluation of vancomycin dosing in adults. J Pharm Technol 2001; 17: 33–38.
Sawchuk RJ, Zaske DE, Cipolle RJ, Wargin WA, Strate RG . Kinetic model for gentamicin dosing with the use of individual patient parameters. Clin Pharmacol Ther 1977; 21: 362–369.
Meyers GL, Miller WG, Coresh J, Fleming J, Greenberg N, Greene T et al. Recommendations for improving serum creatinine measurement: a report from the laboratory working group of the National Kidney Disease Education Program. Clin Chem 2006; 52: 5–18.
National Institutes of Diabetes and Digestive and Kidney Diseases and National Kidney Disease Education Program. Chronic kidney disease and drug dosing: information for providers. 2009 September. www.nkdep.nih.gov/professionals/drug-dosing-information.htm (accessed May 2011).
Acknowledgements
We thank Patricia Chun, Pharm D for her continuous support of research and Rebecca Chumbley, Pharm D for her expert opinion on SCI.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Lee, J., Dang, A. Evaluation of methods to estimate glomerular filtration rate versus actual drug clearance in patients with chronic spinal cord injury. Spinal Cord 49, 1158–1163 (2011). https://doi.org/10.1038/sc.2011.82
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2011.82
Keywords
This article is cited by
-
Evaluation of the Accuracy of Standard Renal Function Equations in Critically Ill Patients with Subarachnoid Hemorrhage
Neurocritical Care (2020)
-
Evaluating estimated glomerular filtration rates of creatinine and cystatin C for male patients with chronic spinal cord injury
Spinal Cord (2018)
-
The management of neurogenic lower urinary tract dysfunction after spinal cord injury
Nature Reviews Urology (2016)
-
50 years follow-up on plasma creatinine levels after spinal cord injury
Spinal Cord (2014)
-
Estimating the glomerular filtration rate using serum cystatin C levels in patients with spinal cord injuries
Spinal Cord (2012)