Abstract
Study design:
Multicenter international cohort study.
Objective:
The objective of this study was to establish target values for Spinal Cord Independence Measure (SCIM) III scoring in rehabilitation for clinically complete spinal cord lesion (SCL) neurological levels.
Setting:
In total, 13 spinal cord units in six countries from North America, Europe and the Middle East were taken.
Methods:
Total SCIM III scores and gain at discharge from rehabilitation were calculated for SCL levels in 128 patients with American Spinal Injury Association Impairment Scale (AIS) grade A on admission to rehabilitation.
Results:
Median, quartiles, mean and s.d., values of discharge SCIM III scores and SCIM III gain for the various SCL levels are presented. Total SCIM III scores and gain were significantly correlated with the SCL level (r=0.730, r=0.579, P<0.001).
Conclusions:
Calculated discharge SCIM III scores can be used as target values for functional achievements at various neurological levels in patients after AIS A SCL. They are generally, but not always, inversely correlated with SCL level.
Similar content being viewed by others
Introduction
Clinicians involved in the care of patients with spinal cord lesions (SCLs) intuitively assess functional outcomes for various purposes. These include the ability to inform patients and families about prognosis, predict rehabilitation potential, assess rehabilitation efficacy and plan the rehabilitation process. Expected functional outcomes related to the neurological level after complete SCL are well established. Functional outcomes in patients with incomplete SCL, however, depend on several factors, including the severity of neurological deficit, and their sequence may not match that of the SCL levels. It is therefore difficult to predict the functional outcome for each level after incomplete SCL.1
Furthermore, data that would allow prediction of functional status, based on quantitative scoring for each level, in either complete or incomplete SCL, is scarce.2, 3, 4 The motor scores of most functional independence measure items were found to be higher when the neurological level was more caudal, in patients with American Spinal Injury Association Impairment Scale (AIS) grade A, B or C.2 Functional independence measure gain was found to be consistently higher when the neurological level was more caudal in patients with complete spinal cord injuries (SCI), and less consistently in patients with incomplete SCI.4 Spinal Cord Independence Measure (SCIM) II scores were significantly higher when SCLs were in lower spinal cord segments, in patients with complete or almost complete tetraplegia (AIS grades A, or B), but not in patients with paraplegia.3
The present study was undertaken to establish target values for SCIM III scoring at various neurological levels, after rehabilitation, for clinically complete SCL neurological levels. For this purpose, we further analyzed data from our previous multicenter study5 and created SCIM III ‘norms’ for groups of SCL levels.
Materials and methods
The original international SCIM III study sample5 included 425 SCL patients from 13 units in six countries. Inclusion criteria were: SCL (AIS grades A, B, C or D), age 18 years or above and no concomitant impairments that might influence everyday function (such as cognitive or mental impairments). For the present study, we analyzed a subgroup of 128 patients with AIS grade A on admission to rehabilitation, after excluding 23 patients who were missing data suitable for the present analysis.
Male/female ratio in the current sample was 4.3:1, and mean age was 37.5 years (s.d.=14.7). Lesion etiology was traumatic in 83.6% of patients and non-traumatic in 16.4%. Mean duration from injury or lesion onset (the earliest event related to the SCL in a patient's hospital records) to rehabilitation was 3.6 months (s.d.=12.0). The mean length of stay in rehabilitation was 151.8 days (s.d.=80.5).
Total SCIM III scores at discharge from rehabilitation were calculated for SCL levels, combining certain adjacent levels to increase the number of patients in each level group. The relationship of SCL level (or group of levels) with discharge SCIM III score and with SCIM III gain (discharge–admission SCIM III score) was examined using a Kruskal–Wallis test followed by pairwise Mann–Whitney U tests with Bonferroni correction, a one-way ANOVA followed by the Tukey's test for homogenous subsets and by Spearman's correlation test. Data were analyzed using SPSS 15.0 for Windows (SPSS, Chicago, IL, USA).
Results
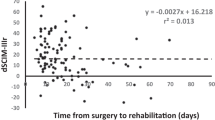
Median and quartile values of discharge SCIM III scores and SCIM III gain, and maximum discharge SCIM III values for the various SCL levels are presented in Tables 1,2,3,4. Mean and s.d. values of discharge SCIM III scores for level groups are presented in Figures 1 and 2.
Differences in discharge total SCIM III scores and gain among cervical, thoracic and lumbar SCL were significant (P<0.001). The total SCIM III score and gain were significantly correlated with the SCL level (r=0.730, r=0.579, respectively, P<0.001).
Despite the strong correlation, however, total SCIM III scores and gain were found to be smaller at certain lower lesion levels than at higher ones (Table 1). Furthermore, when analyzing the thoracic levels separately, the difference in discharge total SCIM III scores and in SCIM III gain between the T2 and T12 segments was not significant (P>0.2). Although the increase in SCIM III score was fairly consistent throughout the levels, the differences between pairs of level groups (Figures 1 and 2) were significant for the cervical group and between the lumbar and cervical or upper thoracic groups (P<0.05), but not between the thoracic level groups or between the lumbar and the lower thoracic groups (P>0.05). The difference in SCIM gain between the L1 and L2 segments was likewise nonsignificant (P=0.7).
Discussion
This is the first report from a multicenter study presenting detailed values of SCIM III scores achieved after rehabilitation in a relatively large group of patients with complete SCI at various spinal cord levels. Although score values for SCL levels have already been described for the functional independence measure2 and for SCIM II,3 the data for the current SCIM III version, presented in this study is more detailed, refers to all the subscales and tasks, and is specific for AIS A SCL. Despite the clear differences shown in functional independence measure scores at discharge from rehabilitation for different neurological SCL levels (including patients with Frankel grades B or C),6 we decided to focus on outcomes for patients with AIS A. The lesions of the AIS A patients are more homogenous, and we assume that their discharge score is a better representation of the maximal possible SCIM III score at various SCL levels, and a better ‘functional norm’ or ‘functional benchmark’ for these levels.
Consistent with previous publications,2, 3 in this study, we also found a negative correlation between the SCL level and the discharge functional score, and we demonstrate a similar relationship between SCL level and the functional improvement during rehabilitation, reflected by the SCIM III gain. Note, however, that this relationship is not absolutely sequential, and as already shown in a paper that examined SCIM II,3 the SCIM III scores differ between cervical SCL levels but not significantly among thoracic SCL levels, and may not differ between lumbar and thoracolumbar levels. The nonsignificant difference among thoracic SCL levels corresponds with the limited contribution of thoracic nerve roots to movements that are involved in primary activities of daily living tasks, which are assessed by SCIM. It is possible to argue, however, that the nonsignificant difference between thoracic SCL levels results from a lack of sensitivity of the items included in SCIM III to the contributions of the trunk musculature to the performance of activities of daily living. Also worth noting is the finding that the C6 group total SCIM score at discharge, and particularly its SCIM discharge–admission gain, were much greater than those of the lower C7 group. This may be related to the observation that patients with C6 SCL have a potentially greater ability to respond to intensive rehabilitation and achieve greater functional gains during initial rehabilitation than do other cervical levels.
The discharge SCIM III scores presented in this study can be used as target values for functional achievements in most patients with complete SCLs, whose prospect for neurological improvement is small, and functional improvement relies heavily on the efficiency of rehabilitation. They may also be used as ‘minimum target values’ for patients with incomplete lesions. But their value for assessing rehabilitation potential or success is limited because most of our patients have incomplete lesions5 and even some of the complete lesions recover. Furthermore, the traditional intuitive use of SCL level and AIS grades to assess rehabilitation potential or success is complex and may be inaccurate, because to obtain information about the relationship between the functional status and the impairment, it requires integration of two different variables that do not allow a continuous representation of the impairment. Therefore, an instrument such as the the Spinal Cord Injury Ability Realization Measurement Index 7 should be used for these purposes. It was developed recently by a team from Loewenstein Rehabilitation Hospital to enable functional outcome assessment, independent of the neurological deficit, bypassing the sequence mismatch between the functional status and SCL level. The instrument relates the functional status to the American Spinal Injury Association motor score, and not to the neurological level or to the AIS grade, allowing representation of the impairment by one practically continuous variable.7 The value of the presented scores for patients with complete high tetraplegia may also be limited, because they are underrepresented in the cohort for whom data was analyzed in this study. An additional limitation of the study is the relatively small number of patients for each spinal cord level. This may affect the predictors presented. The predictors may be refined when larger groups with complete SCL are analyzed.
In summary, discharge SCIM III scores and gain values for clinically complete SCL at various levels were calculated and presented. They can be used as target values for functional achievements in patients with complete SCL at various neurological levels, and they are generally, but not always, inversely correlated with the SCL level.
References
Kirshblum S . Rehabilitation of spinal cord injury. In: DeLisa JA (ed). Physical Medicine and Rehabilitation, Principles and Practice. Lippincott Williams and Wilkins: Philadelphia, 2005, pp 1715–1752.
Middleton JW, Truman G, Geraghty TJ . Neurological level effect on the discharge functional status of spinal cord injured persons after rehabilitation. Arch Phys Med Rehabil 1998; 79: 1428–1432.
Van Hedel HJA, Curt A . Fighting for each segment: estimating the clinical value of cervical and thoracic segments in SCI. J Neurotrauma 2006; 23: 1621–1631.
Mingaila S, Krisciûnas A . Occupational therapy for patients with spinal cord injury in early rehabilitation. Medicina (Kaunas) 2005; 41: 852–856.
Catz A, Itzkovich M, Tesio L, Biering-Sorensen F, Weeks C, Laramee MT et al. A multi-center international study on the Spinal Cord Independence Measure, version III: Rasch psychometric validation. Spinal Cord 2007; 45: 275–291.
Ditunno JF, Cohen ME, Formal C, Whiteneck GC . Functional outcomes. In: Stover SL, DeLisa JA, Whiteneck GC (eds). Spinal Cord Injury: Clinical Outcomes from the Model System. Aspen Publishers: Gaithersburg (MD), 1995, pp 10–184.
Catz A, Greenberg E, Itzkovich M, Bluvshtein V, Ronen J, Gelernter I . A new instrument for outcome assessment in rehabilitation medicine: Spinal Cord Injury Ability Realization Measurement Index (SCI-ARMI). Archives of Phys Med Rehabil 2004; 85: 399–404.
Acknowledgements
The study was supported by the Loewenstein Rehabilitation Hospital Spinal Department Research Fund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflicts of interest.
Rights and permissions
About this article
Cite this article
Aidinoff, E., Front, L., Itzkovich, M. et al. Expected spinal cord independence measure, third version, scores for various neurological levels after complete spinal cord lesions. Spinal Cord 49, 893–896 (2011). https://doi.org/10.1038/sc.2011.32
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2011.32
Keywords
This article is cited by
-
Standardized administration and scoring guidelines for the Spinal Cord Independence Measure Version 3.0 (SCIM-III)
Spinal Cord (2023)
-
Prognostic validity of trunk control scales for mobility in individuals with motor complete thoracic SCI: a prospective cohort study
Spinal Cord (2023)
-
Effect of pelvic laparoscopic implantation of neuroprosthesis in spinal cord injured subjects: a 1-year prospective randomized controlled study
Spinal Cord (2022)
-
Functional outcome following inpatient rehabilitation among individuals with complete spinal cord injury in Nepal
Spinal Cord Series and Cases (2021)
-
Advanced weight-bearing mat exercises combined with functional electrical stimulation to improve the ability of wheelchair-dependent people with spinal cord injury to transfer and attain independence in activities of daily living: a randomized controlled trial
Spinal Cord (2020)