Abstract
Study
design:This study was designed as a cross-sectional one. A set of structured questionnaires was administered.
Objectives:
The purpose of the study was to explore the psychological response of the caregivers of people with spinal cord injury (SCI) and to assess the burden of caregiving for SCI persons living in the community in Fiji.
Setting:
Fiji, South Pacific.
Methods:
A total of 30 primary caregivers of persons with SCI. The Index of Psychological Well-Being (IPWB) was used to assess the psychological impact of care giving, and Caregiver Burden Inventory (CBI) was used to evaluate the burden associated with caregiving for persons with SCI. Barthel Index (BI) scale was used to measure the functional abilities of the care recipients.
Results:
The majority of the participants (n=20) were women, who had an ethnic Fijian background (n=18) and were married (n=18), and were spouses (n=13). Mean BI of the persons with SCI was 7.1 (s.d.=5.23) on a 0–20 scale, with 90% (n=27) suffering from moderate-to-very severe disability (BI<15). The mean duration of caregiving was 6.1 years (s.d.=4.23). On average, the caregivers provided 6.1 h (s.d.=2.19) of caregiving per day. The experiences of caregiving adversely affected the caregiver psychological well-being. Participants demonstrated high levels of time-dependent and development burden. Caregiving was significantly related to the number of hours spent providing care (rs=0.35, P<0.05), and the older caregiver age (rs=0.46, P<0.01).
Conclusion:
Being a primary caregiver of a SCI person contributes to caregiver burden and psychological distress. The findings indicate that the contributions of these people should be recognized and interventions should be tailored not only toward the needs of the care recipients but also to the needs of the caregivers.
Similar content being viewed by others
Introduction
Spinal Cord Injury (SCI) is defined as damage to the spinal cord that results in a loss of bodily functions such as movements and feelings.1 SCI occurs predominantly among young adults.2 The effects of SCI are catastrophic not only to the once active, independent person but also to the family and the society as a whole.3 With advances in the medical and rehabilitation services, the life expectancy of persons with SCI has markedly increased, and in many cases it has approached that of the general population,3, 4, 5 requiring varied levels of assistance over their lifespan.5 With a change in the health-care system, early discharge towards community living settings has increased the responsibilities of informal family caregivers.6 Caregivers who live together with the SCI persons in the community often have to take over the many roles and responsibilities of these people.7
In the process of caregiving, many psychosocial issues and burdens arise, which can have a negative impact on the caregiver. Psychosocial issues such as an increased emotional stress, burnout, fatigue, anger, resentment, mental weariness and isolation have been reported in the caregivers of SCI persons.8, 9, 10 Caregiving has been associated with constraints in the social, vocational, and recreational opportunities of the caregivers.11, 12 Low levels of life satisfaction and marital adjustment,4 ill-health and poor quality of life in caregivers has also been reported.2, 6
Much of the available research on caregivers of SCI persons is mainly from developed countries. Very little information is available on the caregivers of SCI persons in developing countries. Interventions and supports identified in western cultures may not be necessarily applicable and suitable for the people in the developing regions. From the experiences of the researcher, family caregivers have an important role in the ongoing care of the persons with SCI in Fiji. The support from the caregivers is required to maintain the health and the well-being of the SCI persons, as well as to keep them within the community living environment. At present in Fiji, there are no other alternative forms of accommodation, which these people can access. Thus, all the persons with SCI are discharged home to be cared for by their family members.
This may result in severe psychological distress to both the parties, and create huge burden on the caregivers who are not prepared to take on the role of caregiving.13 The family caregivers who willingly accept the role of caregiving may also experience certain level of distress and burden when they realize they have little support once they have taken over the role.1, 12
The purpose of this study was to determine the psychological impact and examine the burden of caregiving for caregivers of persons with SCI living in Fiji.
Materials and methods
Study design
This study used a cross-sectional study design. The data were collected among 30 primary caregivers of persons with SCI who were citizens of Fiji. The data collection period was between May and August 2009.
Participants
All persons who were admitted to the National Rehabilitation Medicine Hospital in Fiji from January 1990 to December 2007 were identified from the hospital records. Other persons with SCI who had not received treatment at the National Rehabilitation Medicine Hospital but were members of the Spinal Injuries Association in Fiji were also identified. Overall 294 persons with SCI were identified, and attempts were made to contact them either through telephone or by the postal addresses provided to these two organizations. In total, 48 persons with SCI could be contacted during the data collection period of May–August 2009.
The persons with SCI were then informed of the study purposes and were asked to identify their main caregiver and provide them with the information regarding the study, which was provided to them by the researcher. Caregivers wishing to participate in the study were requested to contact the researcher directly either by telephone or by consenting to the research and sending this information in the stamped envelop provided with the research introduction letter. The definition of the main caregiver used in this study was ‘a family member, related by blood or marriage, deemed by the SCI person to hold the main responsibility in providing care at home’.
Caregivers meeting the following inclusion criteria were recruited to participate in the study: (1) cared for a person with SCI who was at least at 1 year after injury and >18 years of age; (2) provided care for at least 1 year period; (3) was an unpaid caregiver who was aged >18 years; and (4) was a Fiji citizen who was able to speak and understand English, Hindi or Fijian language.
Ethical consideration
Ethics approval was obtained from the Flinders University Social and Behavioral Research Ethics Committee, South Australia and the National Health Research Committee of Fiji. Informed consent was signed by all the participants and the confidentiality of their identity and the information obtained from them was assured.
Procedure
A total of 34 caregivers responded. Three did not meet the inclusion criteria (two were underaged and one was not the main caregiver), and one caregiver could not be contacted again after the initial contact. A total of 30 participants were finally recruited in this study. Data was collected through interviews in the form of structured questionnaires. Overall, 28 participants preferred face-to-face interview in their home environment and two participants had telephone interview for the completion of the questionnaires. To avoid any possibility that the presence of the care recipient might influence the response of the caregivers, the interviews were held in an enclosed area out of reach by the SCI person.
Instruments
The major categories of data collected were:
Sociodemographic information of caregivers and care recipients
A specially designed proforma was used to assess the sociodemographic characteristics of the caregivers. This information included age, gender, race, relationship to the care recipient, number of caregiving hours, employment history, types of assistance provided, types of assistance received and economic status. Information about care recipients included clinical details of SCI, employment history and marital status.
Psychological well-being of the caregivers
Index of Psychological Well-Being (IPWB) was used to measure the psychological impact of caregiving. It is an eight-item, self-report scale developed by Berkman14 and is designed to measure mental health in general adult population. The IPWB is composed of five negative and three positive items and provides a composite score describing the relative strength in an individual's positive and negative feelings. The scale provides a score of 1–7, with a score of 1 indicating a high level of psychological well-being and 7 indicating a very poor state of mental health. Berkman14 reports on the validation of IPWB, which is supported by a mental health study of Langer and Michael.15 Index of Psychological Well-Being has been used in the caregivers of persons with SCI.16 Berkman14 reported a mean score of 3.77 for a general population, whereas Schulz et al.16 reported a mean score of 3.91 for their caregiver sample and 4.04 for the SCI sample.
Caregiver burden
Caregiver burden was assessed using Caregiver Burden Inventory (CBI). It is a multi-dimensional instrument developed by Novak and Guest17 that measures the impact of burden on the caregivers. CBI consists of five subscales:
-
Time-Dependence Burden (burden because of restriction on the caregiver's time).
-
Developmental Burden (feeling of being left behind in their development in respect to their peers).
-
Physical Burden (feelings of chronic fatigue and damage to physical health).
-
Social Burden (feelings of role conflict, resulting in arguments and time limitation).
-
Emotional Burden (negative feelings towards the care recipient).
Each subscale consists of five items except for the physical burden subscale, which contains only four items. Each item is scored on a Likert scale from 0 (strongly disagree) to 4 (strongly agree). Scores from each subscale (with a maximum score of 20) are added to give a total score ranging from 0 to 100. The higher the scores in each subscale, the more severe the burden imposed on the caregivers. CBI has shown good internal reliability (0.73–0.85) and inter-correlations of subscales, and high-factor loadings.17 CBI has been used to measure the caregiver burden in spouses of SCI persons.8
Functional independence of the care recipients
The level of independence in self-care and mobility of the SCI persons was measured using a modified version of the original Barthel Index (BI).18 This version of BI contains 10 questions about self-care, continence and mobility tasks. BI scores range from 0 to 20, with a score of:
-
0–4, indicating very severe disability
-
5–9, indicating severe disability
-
10–14, indicating moderate disability
-
15–19, indicating minor disability
-
20, indicating complete independence
Information on BI can be obtained either from an attending nurse or a relative, making it a convenient tool to assess self-care activities of a care recipient through a caregiver. Post et al.19 reported good internal consistency and criterion validity of this measure in a SCI population. In the present study, information on Barthel Activities of Daily Living (ADL) Index for SCI persons was obtained from the caregivers.
Data analysis
All data collected were analyzed using the statistical software SPSS (version 17.0, The Flinders University of South Australia, Adelaide, South Australia) for Windows. Descriptive statistics were obtained for demographic data and BI scores. Mean and s.d. were used to describe continuous variables and frequency distribution was obtained for categorical data. The association between ordinal variables was analyzed with Spearman's rank correlation and Mann–Whitney U-test was used for differences between groups. A one-way between-groups analysis was conducted to compare means of categorical variables with three or more values. A P-value of less than 0.05 (P<0.05) was chosen as the level of significance.
Results
The sample comprised of 30 primary caregivers of persons with SCI. The sociodemographic data of the participants and the care recipients are presented in Table 1. The majority of the participants (n=20) were women, who had ethnic Fijian background (n=18) and were married (n=18), and were spouses (n=13). The average household income was F$3920, with only 10% of the total participants living above the poverty line in Fiji.20 The age of the participants ranged from 21 to 70 years, with the mean age of 39.2 years (s.d.=14.12). The duration of caregiving ranged from 1 to 16 years, with a mean of 6.1 years (s.d.=4.23). On average, the caregivers provided 6.1 h (s.d.=2.19) per day of caregiving, with 63.4% (n=19) spending between 6 and 10 h a day assisting with activities of daily living.
The age of the care recipients ranged from 21 to 65 years, with the mean age of 38.5 years (s.d.=12.4). Majority of the care recipients were men (n=26), suffering from paraplegia (n=18) and had complete injuries (n=23). Epidural abscess (n=9) was a common cause of SCI. The duration of the injury ranged from 1.5 to 18 years, with a mean of 7.4 years (s.d.=4.8). One of the notable findings is that, although 29 (96.7%) persons were either in employment or were studying before SCI, 28 (93.3%) persons became unemployed following SCI. It is also noted that majority of the individuals who were married before the SCI remained married after SCI, whereas majority of those who were single before SCI remained single following SCI.
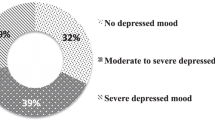
Psychological well-being of the caregivers
The mean score of IPWB for the caregivers was 4.5 (s.d.=1.52). The IPWB scores were not affected by the caregiver age (rs=0.16, P>0.05), the number of hours spent caregiving (rs=−0.12, P>0.05), the number of years of caregiving (rs=−0.02, P>0.05), the level of lesion (z=−0.45, P>0.05) and the severity of disability (F(3, 26)=0.37, P=0.77). However, a strong positive correlation was found between IPWB and CBI scores (rs=0.52, P<0.01).
No statistically significant differences were found between ethnicity (F(2, 27)=2.39, P=0.11)) and the employment status of the caregivers (F(3, 26)=2.10, P=0.12). Although a significant difference was found between the marital status of the caregivers (F(2, 27), P=0.03), post hoc comparison did not reveal any significant differences between the groups. A statistically significant difference among the mean scores on IPWB was found for the various relationships to the care recipient group (F(4, 25)=5.10, P=0.004). Post hoc comparisons indicated the mean scores for spouses (M=5.08, s.d.=1.26), mothers (M=4.80, s.d.=1.30) and siblings (M=5.0, s.d.=1.0) were statistically different from the mean scores of children (M=2.25, s.d.=0.96).
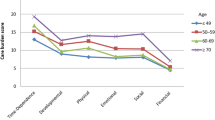
Assessment of caregiver burden
The mean score of total CBI was 47.6 (s.d.=21.39) (Table 2). The participants scored highest in time-dependent burden (mean=13.6; s.d.=4.42) followed by development burden (mean=11.9; s.d.=4.42).
A significant relationship was found between CBI and IPWB scores. Greater caregiver burden correlated positively with poorer psychological well-being (rs=0.52, P<0.01). A significant association between total burden and age was found, (rs=0.46, P<0.01), indicating older caregivers experienced greater caregiver burden. Caregiver total burden was also significantly associated with the number of hours caregiving per day (rs=0.35, P<0.05), suggesting that caregiver burden increased with the increasing amount of time spent providing care. No significant difference was found between the amount of burden experienced by the caregivers of the paraplegic persons and the caregivers of the tetraplegic persons (z=−0.93, P>0.05). Only scores on time-dependent and development burden were significantly associated with the number of hours caregiving per day and caregiver age. Caregiver burden was not influenced by the gender (z=−0.13, P>0.05), income (rs=0.01, P>0.05), number of years in caregiving (rs=0.29, P>0.05), and the completeness of the SCI (z=−0.12, P>0.05). Scores on other subscales of CBI were independent of all the variables.
A statistically significant difference was found for the various relationships to the care recipient group: (F(4, 25)=3.58, P=0.02). Post hoc comparisons indicated that the mean scores for spouses (M=52.13, s.d.=20.83), mothers (M=54.40, s.d.=22.07) and siblings (M=57.35, s.d.=15.70) differed significantly from the mean scores of children (M=17.13, s.d.=5.80). No differences were found between the other groups.
Functional abilities of the care recipients
Analysis of BI scores is listed in Table 3. Majority of the care recipients (n=27) had moderate-to-very severe disability. As such, many individuals required assistance in many activities of daily living as well as assistance in other activities (Table 4).
Types of support received
Assessment of the types of support received by the caregivers of SCI persons is listed in Table 5. Approximately, 90% (n=27) of the participants reported receiving help from other family members. Religious organizations mostly provided spiritual support. Community health professionals’ support was reported to be very low.
Discussion
This study confirms that persons with SCI in Fiji are mostly men, younger in age and require support from their family members for successful community living. It is also worth noting that a major cause of SCI in a developing country is from infectious causes.
The mean psychological well-being score on the IPWB for the caregivers in this study were relatively high in reference to the suggested cutoff value of 3.77 for the general population,14 and the mean scores of 3.91 for the caregivers of SCI persons.16 This indicates that caregiving is a stressful experience. Depression, anxiety and poorer psychological well-being have been a common finding in studies evaluating the caregivers of SCI persons.1, 2, 5, 9, 13, 21 The findings of this study suggest that the caregivers of SCI persons living in Fiji experience a higher level of psychological burden than the caregivers living in the Western world. This study also confirms that caregiver burden is an important contributing factor to poorer psychological well-being, a finding which has been previously documented.10, 12
On the CBI scale, caregivers scored much higher on the time-dependent and the development burden subscales compared with other subscales. These findings are similar to that reported in a Chinese population,8 with the scores in this study being slightly higher than the scores reported in their study. Time-dependent burden reflects the limitations imposed on the caregiver because of the amount of time spent providing care for the SCI person. Development burden is a feeling of being left behind in terms of development with respect to the peers. A significant relationship was found between these two variables and the number of hours of caregiving per day, indicating that burden increased with increasing time spent assisting the care recipients on a daily basis. Owing to the caregiving duties, they most probably felt too fatigued or did not have time to carry out other chosen activities. These findings are consistent with other studies, which have identified level of assistance provided in ADL and the number of hours spent providing support for the SCI person as strong contributors of caregiver burden.16, 19 However, there was no relationship between the caregiver burden and the time till which caregiving had been provided. Family support toward the care of the SCI persons was highly evident in this study. This lack of relationship could reflect that the caregivers still had time to interact with their peers in the long term with the help of other family members toward the overall care of the SCI persons. Scores on the emotional subscale was the lowest, indicating the caregivers have accepted their roles and made adjustments to some extent, and thus do not feel resentful toward their care recipient.
In this study, older caregivers were found to be significantly more burdened than the younger caregivers, a finding, which has been previously reported by Post et al.19 One of the explanations could be that the aging caregivers most probably find it more difficult to devote time and energy in caring for a close family member who requires moderate-to-heavy assistance in many daily tasks. They may require some care themselves.
Siblings, mothers and spouses reported significantly higher levels of psychological distress and caregiver burden compared with children. The low levels of burden and higher psychological well-being in children would most likely be explained by the view of caregiving as an expected family responsibility. In the Fijian and Indian cultures, children are expected to provide care for their aging parents. Thus, caring for a parent with a disability may not be perceived any differently from caring for an aged parent without a disability.
Generally, it is expected that the caregivers will more likely assist an SCI person with a high level injury such as tetraplegia.2, 21 This study did not find any significant relationship between the level of injury and the caregiver burden, and is similar to the findings reported in other non-Western countries.7, 22 This could be because of the fact that the majority of the paraplegic persons, who were expected to be independent in self-care and mobility, suffered from moderate-to-severe disability requiring assistance in many ADL. Information obtained during the interview revealed a lack of appropriate mobility equipment and adaptive devices, inappropriate home environment, restricting wheelchair access and poor socioeconomic status of many families as factors affecting caregiving roles. In total, 26 caregivers specifically mentioned assisting care recipients with transfers and actually ‘lifting’ them with the help of another family member. Severe economic constraint is a common issue when dealing with SCI.23, 24 In this study, unemployment among SCI persons was very high, and majority of the caregivers did not have any paid employment. In many cases, the SCI persons were the sole breadwinners for the family before the injury. This forced many families to slip into poverty, reducing their ability to purchase the necessary items required to enhance the independence of SCI persons. Home renovation became almost impossible. As a result, many caregivers ended up providing many hours of support per day, which otherwise could have been performed by the SCI persons themselves. Thus, with lack of resources, lower level SCI require more care in a developing country like Fiji compared with resource-rich developed countries. Inaccessible physical environment contributing to caregiver burden has been reported in other studies.25, 26 Blanes et al.26 found their sample of caregivers reported much higher on the environment dimension of the Caregiver Burden Scale, suggesting that the caregivers were more burdened by lack of accessible environment, which they perceived as limiting the independence of the SCI persons. Higher household income has been reported to be associated with lower time-dependent burden.8
In addition, the other important findings of this study are the absence of paid support and the presence of other family members in the care of SCI persons. Extended family structure is a common feature of the Fijian culture. Caregivers acknowledged the support of other family members who provided assistance with ADL, helped with respite care when the participants needed time for other commitments, accompanied care recipients on outdoor activities and provided financial support. Assistance of other family members’ towards caregiving chores has been reported in minority ethnic groups and other cultures.4, 12, 26, 27 Although paid care support is a common feature in Western countries,19, 28 it is almost non-existent in a developing country like Fiji. Thus, the gap in the continuation of care is most likely filled by others present around these individuals.
Support from health professionals was noted to be poor. In Fiji, Community Rehabilitation Out-reach Services are conducted by the same group of health professionals who also provide hospital-based care. Thus, they are restricted with time flexibilities, transport needs and lack of adequate staff. However, despite these limitations, every effort is made by these professionals in providing ongoing support for both the caregivers and the care recipients with SCI. Community health professionals based at the district level, who are supposed to provide home support and advice, reached only a few families. There is generally lack of professional support for the caregivers of SCI persons.2 Community health professionals usually lack knowledge related to SCI and its consequences, and the impact it has on the caregivers.2 This could be one of the reasons for the lack of community health support towards this group of persons in Fiji.
Implication
Family members are the primary sources of caregiving for SCI persons in Fiji providing a wide range of support services, extending from assistance in personal care to help with instrumental ADL. Results of this study indicate that the experiences of caregiving adversely affected the psychological well-being of the caregivers in the Fijian context. These results highlight the need to investigate the efficacy of interventions such as providing training, establishing professional support services, such as counseling and provision of respite care for the SCI persons to minimize caregiver burden. In addition, financial support towards home modification and to help acquire essential equipment and adaptive devices may also assist in reducing caregiver burden, thus, improving the well-being of the persons who are essential in maintaining the health and welfare of the SCI persons living in the community in Fiji.
Limitations
One of the limitations of this study includes the nonrandom sampling and the small sample size. Second, this study included only the caregivers of those persons who had received care at the National Rehabilitation Medicine Hospital or were members of the Spinal Injuries Association who had access to professional support. Caregivers of SCI persons outside these organizations were not included. Thus, the findings may have introduced a potential bias. Third, owing to the geographical location of the Fiji Islands, SCI persons living elsewhere other than the main island of Viti Levu could not be contacted because of lack of postal or telephone contacts. No effort was made to physically locate them because of the time limitations and the expenses that would have been incurred. Thus, the statistical power and the generalizability of the findings in this study may be limited.
Despite this the study reveals some interesting findings. This present study serves as an exploratory role into the perceived burden and the psychological well-being of family caregivers of SCI persons in Fiji. Further research with larger sample size and a more representative SCI population is needed to confirm the findings.
References
Azevedo GR, Santos VLC . (Handicapped) caregiver: the social representations of family members about the care-giving process. Rev Latino-am Enfermagem 2006; 14: 770–780.
Boschen KA, Tonack M, Gargaro J . The impact of being a support provider to a person living in the community with a spinal cord injury. Rehabil Psychol 2005; 50: 397–407.
Atrice BS, Morrison SA, McDowell SL, Ackerman PM, Foy TA . Traumatic spinal cord injury. In: Umphred DA (ed). Neurological Rehabilitation, 5th edn. Mosby Elsevier: USA, 2007, pp 605–657.
Chan RCK . Stress coping in spouses of persons with spinal cord injuries. Clini Rehabil 2000; 14: 137–144.
Shewchuk RM, Richards JS, Elliot TR . Dynamic processes in health outcomes among caregivers of patients with spinal cord injuries. Health Psychol 1998; 17: 125–129.
Evans RL, Hendricks RD, Lawrence KV, Bishop DS . Identifying factors associated with health care use: a hospital-based risk screening index. Soc Sci Med 1988; 27: 125–129.
Unalan H, Gencosmanoglu B, Akgun K, Karamehmetoglu S, Tuna H, Ones K et al. Quality of life of primary caregivers of spinal cord injury survivors living in the community: controlled study with short form-36 questionnaire. Spinal Cord 2001; 39: 318–322.
Chan RCK, Lee PWH, Lieh-Mak F . Coping with spinal cord injury: personal and marital adjustment in the Hong Kong Chinese setting. Spinal Cord 2000; 38: 687–696.
Kolakowsky-Hayner SA, Kishore R . Caregiver functioning after traumatic injury. NeuroRehabilitation 1999; 13: 27–33.
Weitzenkamp DA, Gerhart KA, Charlifue SW, Whiteneck GG, Savic G . Spouses of spinal cord injury survivors: the added impact of care-giving. Arch Phys Med Rehabil 1997; 78: 822–827.
Delargy M, Parry H, Burt A . Quadriplegic care: an assessment of the impact on the carer. Int Disabil Stud. 1988; 10: 145–147.
Elliott TR, Shewchuk RM . Recognising the family caregiver: integral formal members of the rehabilitation process. J Vocat Rehabil 1998; 10: 123–132.
Raj JT, Manigandan C, Jacob KS . Leisure satisfaction and psychiatric morbidity among informal carers of people with spinal cord injury. Spinal Cord 2006; 44: 676–679.
Berkman PL . Measurement of mental health in a general population survey. Am J Epidemiol 1971; 94: 105–111.
Langer TS, Michael ST . Life Stress and Mental Health. Glencoe, Free Press, 1963.
Schulz R, Tompkins CA, Wood D . The social psychology of care-giving: physical and psychological costs of providing support to the disabled. J Appl Soc Psychol 1987; 17: 401–428.
Novak M, Guest C . Application of a multidimensional caregiver burden inventory. Gerontologist 1989; 29: 798–803.
Collin C, Wade DT, Davies S, Horne V . The Barthel index: a reliability study. Int Disabil Stud. 1988; 10: 61–63.
Post MWM, Bloemen J, Witte LP . Burden of support for partners with spinal cord injuries. Spinal Cord 2005; 43: 311–319.
Fiji islands bureau of statistics: poverty 2008-2009 household income and expenditure. Accessed: 20 October 2010 on www.Statsfiji.gov.fj/social/povertyindicators.htm.
Dreer LE, Elliot TR . Family caregivers of persons with spinal cord injury: predicting caregivers at risk for probable depression. Rehabil Psychol 2007; 52: 351–357.
Manigandan C, Saravanan B, Macaden A, Gopalan L, Tharion G, Bhattacharji S . Psychological well-being among carers of people with spinal cord injury: a preliminary investigation from South India. Spinal Cord 2000; 38: 559–562.
Jenik F, Kuhn W, Zach GA . Social and vocational reintegration of paraplegic and tetraplegic patients in Switzerland. Paraplegia 1982; 20: 65–70.
Webb SM, Lorenzi ME, Berzins E . Marital, educational, employment, income and general financial status prior to and one to six years post-spinal cord injury. Paraplegia 1982; 20: 108–109.
Bajwa TJ . Impact of physical environment on quality of life of spinal cord injury family caregivers. Arch Phys Med Rehabil 2006; 87 (Poster 29): E17.
Blanes L, Carmagnani MIS, Ferreira LM . Health-related quality of life of primary caregivers of persons with paraplegia. Spinal Cord 2007; 45: 399–403.
Pinquart M, Sorensen S . Ethnic differences in stressors, resources, and psychological outcomes of family care-giving: a meta-analysis. Gerontologist 2005; 45: 90–106.
Kemp LA . Care and services for spinal injured people with and without neurological deficit. Disabil Rehabil 2002; 24: 810–816.
Acknowledgements
I would like to thank my supervisor Mr Simon Gunn for his support in helping me complete my research project. Special thanks to the participants of this study who joyfully agreed to share their knowledge and experiences of caregiving with me. Lastly, I would like to thank the National Health Research Committee of Fiji for the financial support towards this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The author declares no conflict of interest.
Rights and permissions
About this article
Cite this article
Gajraj-Singh, P. Psychological impact and the burden of caregiving for persons with spinal cord injury (SCI) living in the community in Fiji. Spinal Cord 49, 928–934 (2011). https://doi.org/10.1038/sc.2011.15
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2011.15
Keywords
This article is cited by
-
Correlations between ADL in patients with SCI and caregiver burden, quality of life, and presenteeism in South Korea
Scientific Reports (2024)
-
Caregiver burden according to ageing and type of care activity in caregivers of individuals with spinal cord injury
Spinal Cord Series and Cases (2023)
-
Burden of care among primary caregivers’ of spinal cord injury patients attending a tertiary care center in Eastern Nepal
Discover Social Science and Health (2022)
-
Burden in caregivers of spinal cord injury patients: a systematic review and meta-analysis
Acta Neurologica Belgica (2022)
-
Is caregiver quality of life predicted by their perceived burden? A cross-sectional study of family caregivers of people with spinal cord injuries
Spinal Cord (2021)