Abstract
Study design:
Case–control study.
Objectives:
To investigate changes of biomechanical skin properties and their relationship with paralysis following spinal cord injury (SCI).
Setting:
South Korea.
Methods:
A total of 48 male subjects with chronic SCI and 48 age-matched healthy controls were enrolled into this study. The C4 shoulder group and L2 thigh group were prescribed by two measured anatomical regions that represented the C4 and L2 American Spinal Injury Association sensory dermatomes. Each anatomical group was comprised of one control subgroup and three SCI subgroups determined by sympathetic paralysis at the measured region and somatic completeness. The following biomechanical skin properties were compared between the subgroups in each anatomical group by using Cutometer, a non-invasive suction device: distensibility (Uf), elasticity (Ua/Uf and Ur/Uf) and viscoelasticity (Uv/Ue and H). The impact of sympathetic and somatic sensory paralysis, somatic completeness, age, smoking, body mass index and duration of injury on the indices of skin properties were analyzed.
Results:
In each anatomical group, sympathetic paralyzed subgroups regardless of somatic sensory completeness showed lower value of skin distensibility (Uf), and higher values of elasticity (Ua/Uf and Ur/Uf) and viscoelasticity (Uv/Ue and H), compared with other subgroups. Age and duration of injury had significant impact on biomechanical skin properties.
Conclusion:
The non-invasive suction method is useful for quantitative evaluation of skin affected by SCI. In chronic SCI patients, biomechanical skin properties are significantly altered in the skin with sympathetic paralysis rather than somatic sensory paralysis.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) causes many skin complications. However, with the exception of pressure ulcers, these complications are easily overlooked because they do not have life-threatening sequelae. SCI is a systemic disease that involves the immune, sympathetic and sensory nervous systems. Altered physiological conditions following SCI have direct impact on cutaneous behaviors.
Common skin complications following SCI include local fungal infection, seborrheic dermatitis, chronic acne vulgaris and pressure ulcers.1, 2 Attenuated immune response following SCI facilitates skin infections and lack of cutaneous sensation increases the incidence of pressure ulcers. However, the exact mechanism of delayed wound healing and chronic skin thickening remains to be elucidated. Studies have reported that skin following SCI exhibited deficient vascular reactions, decreased fibroblast activity, higher collagen catabolism and subtype changes.3, 4, 5 These deficiencies may interrupt each step of the natural wound healing process.6 Chronic SCI patients also experience skin thickening, which can be observed as early as 6 months after injury and appears to increase gradually over the first 5 years, then plateau. In addition, skin thickening correlates well with the neurologic level of injury (NLI) and the grade of autonomic dysreflexia. It is more commonly found in patients with NLI above T6, and high grade of severe autonomic dysreflexia on a scale of 0–3.2
The lack of supraspinal control following SCI causes autonomic dysfunctions, including vasomotor and sudomotor actions7 that may have important roles in regulating the biomechanical properties of the skin. The descending vasomotor and sudomotor fibers, primarily dependent on the sympathetic nervous system between T1 and L2 spinal segments, travel together within the intermediolateral tract of the spinal cord.8 Therefore, the integrity of the sympathetic pathways following SCI can be assessed not only by measuring either vasomotor or sudomotor responses, but also by investigating the overall properties of the skin.
Cutometer is a reproducible and non-invasive in vivo suction device that can determine the biomechanical properties of human skin. All the parameters measured by Cutometer are related to the composition and structure of the skin that exhibits high inter- and intra-rater reliability.9, 10 The parameters consist of the following biomechanical skin properties: distensibility, elasticity and viscoelasticity. And they can be divided into absolute and relative parameters. The absolute parameters are demonstrated in Figure 1. The relative parameters are independent of skin thickness and can be directly compared between subjects or anatomical regions.9 In this study, the following parameters were selected to compare between subgroups: (1) Uf (final distension), total displacement from initial position at maximum negative pressure, is linked to collagen and elastic fibers stretching, and represents skin distensibility and thickness. (2) Ua/Uf (gross elasticity), the ability of the skin to return to its initial position following deformation, is related to the function of elastic fibers. (3) Ur/Uf (biological elasticity), the ratio of immediate retraction to total distension, is frequently used in the clinical setting, which also explains the function of the elastic fibers. (4) Uv/Ue (viscoelasticity), the ratio of viscoelastic to elastic distension, is attributed to the displacement of interstitial fluid throughout the fibrous network and indicates the viscoelastic component of deformation. (5) H (hysteresis) is the difference between distension between the fifth and the first suction.9, 11
Cutometer has been used as a tool in the research of normal skin and skin diseases that affect skin mechanics, such as psoriasis, scleroderma and diabetes mellitus.12, 13, 14, 15 However, to our knowledge, no study has systematically examined skin affected by SCI with the intention to define the precise biomechanical features and to elucidate which nervous systems are directly associated with skin alterations.
The objective of this study was to compare the biomechanical skin properties between subgroups of SCI and control, to investigate detailed skin changes and their relation to paralysis.
Materials and methods
Subjects and study group
A total of 48 male patients with a minimum of 6-month SCI history and NLI with C4 or below were enrolled into the study. A total of 48 age-matched healthy subjects were recruited as control. To avoid confounding factors, we controlled smoking history, anthropometric data of weight, height and body mass index between subgroups.
Neurological examinations were performed according to the International Standards for Neurological Classification of Spinal Cord Injury.16 We excluded subjects with: (1) focal dermatological conditions at the region of measurement (for example, localized edematous condition, hypertrophic scar and burns), (2) evidence of systemic disorders or known neuropathy that could have influenced the biomechanical skin properties (for example, scleroderma, psoriasis, keloid, diabetes mellitus and renal failure), (3) brain or brain stem lesion and (4) disability to assume a neutral supine position due to severe spasticity or joint contracture.
To investigate the impact of somatic sensory paralysis on the biomechanical skin properties, all participants with SCI and control subjects underwent skin testing in each region of the C4 and L2 American Spinal Injury Association sensory dermatomes. All the subjects belonged to each of C4 shoulder group (SG) and L2 thigh group (TG). Each anatomical group was further divided into one control subgroup and three SCI subgroups, determined by regional sympathetic paralysis and degree of somatic completeness. Figure 2 illustrated the ‘sympathetic dermatomes’17, 18, 19 compared with the American Spinal Injury Association sensory dermatomes.
-
Subgroup 1 (SG1 or TG1) was comprised of complete somatic (AIS A) SCI patients whose sensory NLI were high enough to present sympathetic paralysis of the measured dermatomes. SG1 showed no sensory zone of partial preservation extending throughout the thoracic dermatomes, and TG1 did not have any somatic sensory sensation at L2 dermatome or below.
-
Subgroup 1-I (SG1-I or TG1-I) consisted of incomplete somatic (AIS B to D) SCI patients whose criteria for sensory NLI were identical to that of subgroup 1.
-
Subgroup 2 (SG2 or TG2) was comprised of SCI patients with any AIS whose sensory NLI were low enough to preserve normal sympathetic integrity of the measured dermatomes.
-
Subgroup 3 (SG3 or TG3) consisted of healthy controls for each anatomical group.
Definitions of each subgroup and their characteristics of neural innervations are summarized in Table 1.
Skin measurements
Subjects were made comfortable and acclimatized to room conditions. Room temperature was maintained at 20–25 °C and relative humidity at 40–50 %.12 Biomechanical properties of the skin were determined with a non-invasive, reproducible suction device, Cutometer MPA 580 (Courage & Khazaka Electronic GmbH, Köln, Germany). It evaluates skin vertical deformation using an optical unit when it is pulled upwards by means of a controlled vacuum.9, 11 Among 2−8 mm diameter probes, large 8 mm probe was used in this study. The time/strain mode was selected, with five consecutive cycles of a 5 s application of vacuum at 450 mbar, followed by a 3 s relaxation period (Figure 1).14 In the supine position, biomechanical skin properties were measured in two body regions of the non-dominant side: the anterior shoulder (C4 American Spinal Injury Association sensory dermatome) and the middle of the medial thigh (L2 American Spinal Injury Association sensory dermatome) (Figure 2). In each of the measured regions, the values of skin deformation obtained were analyzed using the Cutometer MPA 580 software. The study protocol was approved by the Research Ethics Committee of Soonchunhyang University Hospital. All patients and control subjects gave written informed consent at study enrollment.
Statistical analysis
In each anatomical group, the mean values of the biomechanical skin parameters, as well as age, duration of injury and anthropometric data, were compared between subgroups. Significant differences of the mean values were analyzed by one-way analysis of variance with post hoc comparisons using the Tukey test. The χ2-test was used to compare the ratio of smoker between each subgroup. The Pearson’s correlation coefficient test was used to evaluate the relationship between age and the measured variables. The impact of age and duration of injury on biomechanical skin properties in the SCI subgroups were determined using multiple linear regression analyses. A level of P<0.05 was considered statistically significant. All analyses were performed using SPSS 14.0 software for Windows (SPSS Inc., Chicago, IL, USA).
Results
A total of 48 male patients with chronic SCI (mean age, 44.8±12.3; range, 21–67) and 48 age-matched normal healthy controls (mean age, 43.9±12.5; range, 21–67) were recruited. For each C4 shoulder and L2 TG, there was no significant differences in age, ratio of smoker, weight, height and body mass index between the subgroups. The mean duration of injury was shorter in SG1 (mean year, 2.7±0.9; range, 0.7–4.2) than in SG1-I (mean year, 6.9±7.0; range, 0.9–19.6, P=0.007) and SG2 (mean year, 12.1±10.7; range, 1.1–35.6, P=0.07), although all SCI patients were in chronic state more than 6 months following injury. Detailed demographic and clinical characteristics of the subjects are presented in Tables 2 and 3.
Comparison of biomechanical skin properties between main subgroups
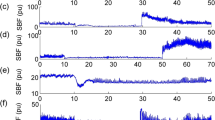
To investigate sympathetic influence on biomechanical skin properties, we compared the mean values of each subgroup in the two anatomical groups (Figure 3). In the C4 SG, in which all the subjects had normal pinprick and light touch sensation (score 2 on three-point scale) at the C4 dermatome, sympathetically paralyzed SG1 (n=11) exhibited significantly different outcomes from SG2 (n=24), as well as SG3 (n=48) (Figure 3a): lower values in the distensibility parameter (Uf, P=0.000 versus SG2, P=0.000 versus SG3) and higher value in the elasticity (Ua/Uf, P=0.001 versus SG2, P=0.000 versus SG3; Ur/Uf, P=0.000 versus SG2, P=0.000 versus SG3) and viscoelasticity parameters (Uv/Ue, P=0.000 versus SG2, P=0.000 versus SG3; H, P=0.001 versus SG2, P=0.000 versus SG3) than SG2 and SG3 subjects. And there were no significant differences in biomechanical skin values between SG2 and SG3 (P⩾0.095). Although all SCI subjects in the L2 TG had no or impaired pinprick and light touch sensation (Score 0 or 1) at the L2 dermatome, TG1 (n=20) also showed significantly different outcomes from TG2 (n=11) and TG3 (n=48) (Figure 3b). The patterns of cutaneous deformation in L2 TG were similar to that observed in C4 SG, except in the absolute viscoelastic parameter of hysteresis (H) that exhibited significantly lower value in TG3 (P=0.000 versus TG1, P=0.010 versus TG2) than that in TG1 and TG2. Thus, TG1 showed lower values in the distensibility parameter (Uf, P=0.046 versus TG2, P=0.014 versus TG3), and higher values in elasticity parameters (Ua/Uf, P=0.048 versus TG2, P=0.003 versus TG3; Ur/Uf, P=0.030 versus TG2, P=0.008 versus TG3) and the relative parameter of viscoelasticity (Uv/Ue, P=0.016 versus TG2, P=0.000 versus TG3) than TG2 and TG3 subjects. There were no significant differences in biomechanical skin values between TG2 and TG3 (P⩾0.888), except in H (P=0.010).
To investigate sympathetic influence on the biomechanical skin properties, the mean skin values were compared between the C4 shoulder subgroups (a), and between the L2 thigh subgroups (b). One-way analysis of variance was performed to compare the three subgroups by using a Tukey’s post hoc test. *P<0.05 versus SG1 or TG1; †P<0.05 versus SG2 or TG2.
Relationship between incomplete somatic lesion and biomechanical skin properties
To examine whether incomplete somatic lesion was associated with sympathetic paralysis, the skin values of subgroup 1-I (SG1-I (n=11) and TG1-I (n=17)) were compared with that of subgroup 1 (SG1 (n=11) and TG1 (n=20)) and that of subgroup 3 (SG3 (n=48) and TG3 (n=48)), respectively (Figure 4). In each C4 shoulder and L2 TG, there were no significant differences across all cutaneous parameters between subgroup 1 and subgroup 1-I (SG1 versus SG1-I, P⩾0.213; TG1 versus TG1-I, P⩾0.902). However, in each anatomical group, complete and incomplete SCI subgroups exhibited significantly different values from normal control subgroups. In the C4 SG, SG3 showed higher value of Uf (P=0.000 versus SG1, P=0.000 versus SG1-I) and lower values of Ua/Uf (P=0.000 versus SG1, P=0.000 versus SG1-I), Ur/Uf (P=0.000 versus SG1, P=0.000 versus SG1-I), Uv/Ue (P=0.000 versus SG1, P=0.000 versus SG1-I) and H (P=0.000 versus SG1, P=0.000 versus SG1-I) than that of SG1 and SG1-I, respectively (Figure 4a). In the L2 TG, although Uf was not statistically different between TG1-I and TG3 (P=0.064), other cutaneous parameters of TG3 were significantly different from that of TG1 and TG1-I (Figure 4b): higher value of Uf (P=0.015 versus TG1), and lower values of Ua/Uf (P=0.002 versus TG1, P=0.006 versus TG1-I), Ur/Uf (P=0.008 versus TG1, P=0.049 versus TG1-I), Uv/Ue (P=0.003 versus TG1, P=0.003 versus TG1-I) and H (P=0.000 versus TG1, P=0.000 versus TG1-I) than that of TG1 and TG1-I.
To investigate the impact of somatic completeness on the biomechanical skin properties, the mean skin values were compared between the C4 shoulder subgroups (a), and between the L2 thigh subgroups (b). One-way analysis of variance was performed to compare the three subgroups by using a Tukey’s post hoc test. *P<0.05 versus SG1 or TG1; †P<0.05 versus SG1-I or TG1-I.
Relationship between independent influential factors and skin variables
Pearson’s correlation coefficients between age and skin variables in each control subgroup (SG3 and TG3) were analyzed (Table 4). In SG3, age had negative correlations with Uf (r= –0.509; P=0.000), Ua/Uf (r= –0.485; P=0.000), Ur/Uf (r=–0.548; P=0.001) and H (r=–0.274; P=0.030), and positive correlation with Uv/Ue (r=0.341; P=0.009). In TG3, age also had negative correlation with Uf (r=–0.292; P=0.022), Ua/Uf (r=–0.294; P=0.021) and Ur/Uf (r=–0.378; P=0.004), and positive correlation with Uv/Ue (r=0.246; P=0.046). Multiple linear regression analyses demonstrated the impact of age in addition to duration of injury on biomechanical skin properties in TG1 (Table 5). Uf and Uv/Ue were significantly influenced by duration of injury, as well as age. Uf and Uv/Ue (dependent variables) could be predicted from linear combination of age and duration of injury, as follows: Uf=1.170+0.072 × duration of injury–0.012 × age, in which adjusted R2=0.82, P<0.001; Uv/Ue=0.144–0.028 × duration of injury+0.013 × age, adjusted R2=0.75, P<0.001. Ua/Uf and Ur/Uf were significantly influenced by duration of injury rather than age, as follows: Ua/Uf=0.837–0.030 × duration of injury, adjusted R2=0.86, P<0.001; Ur/Uf=0.494–0.018 × duration of injury, adjusted R2=0.80, P<0.001. However, independent variables of age and duration of injury did not demonstrate any influence on dependent skin variables in SG1 (n=11) and TG2 (n=11).
Discussion
To evaluate the biomechanical properties of skin affected by SCI, we used a suction skin elasticity meter for the first time in the present study. In doing so we confirmed that biomechanical skin properties were significantly influenced by sympathetic paralysis rather than somatic sensory paralysis.
A recent study on skin axon-reflex vasodilatation (SkARV) demonstrated an excellent relationship between complete somatic lesion (AIS A) and sympathetic paralysis in paraplegic patients with NLI above T12.19 However, there was relatively poor relationship between incomplete somatic lesion and sympathetic paralysis.19 Thus, we hypothesized that SG1 and TG1 based on the classic ‘sympathetic dermatome’17, 18, 19 may have total sympathetic paralysis of the C4 and L2 dermatomes respectively, whereas SG2 and TG2 may show normal sympathetic innervation of the dermatomes. Our study confirmed that the skin of sympathetic denervation showed different values compared with that of normal sympathetic innervation.
As for subgroup 1-I (SG1-I and TG1-I) of incomplete somatic lesion, we hypothesized that the results of skin testing might vary because the extent of sympathetic paralysis was probably related to the severity of the somatic lesion. However, we could not find any differences in skin properties between SCI subjects with complete and incomplete somatic lesion (SG1 versus SG1-I and TG1 versus TG1-I). It can be explained by the small sample size, as only three subjects (6.3%) among 48 SCI patients had mild somatic sensory lesion (AIS D). Furthermore, the duration of injury in SG1-I patients was much longer than that of SG1 patients (6.8 y versus 2.7 y, P=0.007). Thus, SG1-I patients may have had more chance to develop skin deformation than SG1 patients.
In accordance with previous studies,12, 13 age significantly correlates with all biomechanical skin parameters in healthy control subjects. However, in TG1, the duration of injury, rather than the age, was proven to be the most important factor influencing skin changes. Because the amount of dermal thickening is positively correlated with the duration of injury,2 the thickening process following SCI may be strong enough to overwhelm the impact of aging on biomechanical skin properties.
The pathological process of SCI involves not only the epidermis but also the dermis.2, 5 Therefore, we used the large 8 mm diameter measuring probe to determine the biomechanical properties of the whole skin layer, rather than the small 2-mm probe that covers only the epidermis and the papillary dermis.9, 11
Decreased Uf in SG1 and TG1 indicates increased hardening of the skin. This is probably due to chronic skin thickening characterized by brawny induration and dermal fibrosis.2, 5 Clinically, non-pitting thickening and skin hardening is prominent over the face, posterior upper arms and anterolateral thighs in chronic SCI patients. It has been reported that skin thickening is more commonly found in tetraplegia than in paraplegia.2 Histopathologically, fibroproliferative change and shrinkage of the connective tissue were observed in thickened reticular dermis.5 In tetraplegic patients, the skin of the entire body, including that above the somatic sensory NLI, can be affected by interrupted supraspinal control of the sympathetic nervous system. Thus, the face of a tetraplegic is typically characterized by relative pallor, hair loss, anhydrosis, conjunctival redness, oily skin and goose-flesh.20 In the affected skin of chronic SCI patients, Type III collagen exhibiting elastic properties was decreased in the upper dermis without specific changes in Type I collagen.5 However, Ua/Uf and Ur/Uf (gross and biological elasticity) of SG1 and TG1 were unexpectedly increased in this study. The findings suggest that the overall elastic tissues are not seriously involved in the pathological process, and that the elastic fibers are already stretched due to markedly thickened dermis. Moreover, the shrunken collagen bundles might be easily separated from each other, which may reduce the friction between collagen fibers, and facilitates the movement of interstitial fluid in the reticular dermis. This can also explain the reason of increased Uv/Ue. Furthermore, because Uv/Ue is a relative parameter of viscoelasticity, therefore, markedly reduced dermal distension can cause relative increase in the ratio of viscoelastic to elastic distension.
Study limitations
This study has some limitations. First, and most important, sympathetic dermatomes by cord segments are less precise than sensory dermatomes due to larger overlaps.18 To avoid confusion, strict standards were imposed on determining subgroups 1 (SG1 and TG1). Therefore, we did not include patients with incomplete SCI (AIS B to D) to subgroup 1 and excluded two SCI subjects whose somatic sensory NLI were T2 because sympathetic innervation of the skin at the region has not been clearly defined. Second, sexual difference and early findings of skin properties were not demonstrated because all the participants were male, and in a chronic condition with a history of injury of 6 months or more. Third, there was no attempt to quantify hydration using food diary before skin measurements, although it is well known that hydration can affect biomechanical skin properties. Finally, individual skin temperatures at the measured regions were not considered in this study, although room temperature and humidity were strictly controlled in accordance with previous studies.12 It has been generally accepted that skin temperature could be controlled if the room temperature is managed. However, the enrolled subjects were relatively healthy in most previous studies. Thus, it is unclear whether the same can be applied to SCI patients who seriously lack the ability of temperature regulation.
Further studies encompassing larger sample sizes that take into account age, sex, more anatomical regions and important confounding factors are required to ascertain the exact sympathetic dermatome that is important in determining sympathetic NLI.
Conclusions
The biomechanical skin properties were significantly altered following SCI, and these changes were directly influenced by regional sympathetic denervation rather than somatic sensory denervation. Skin property testing using non-invasive, in vivo suction method can have an important role in quantifying the sympathetic involvement of skin affected by SCI.
References
Rubin-Asher D, Zeilig G, Klieger M, Adunsky A, Weingarden H . Dermatological findings following acute traumatic spinal cord injury. Spinal Cord 2005; 43: 175–178.
Stover SL, Hale AM, Buell AB . Skin complications other than pressure ulcers following spinal cord injury. Arch Phys Med Rehabil 1994; 75: 987–993.
Claus-Walker J, Halstead LS . Metabolic and endocrine changes in spinal cord injury: II (section 1). Consequences of partial decentralization of the autonomic nervous system. Arch Phys Med Rehabil 1982; 63: 569–575.
Vaziri ND, Eltorai I, Gonzales E, Winer RL, Pham H, Bui TD et al. Pressure ulcer, fibronectin, and related proteins in spinal cord injured patients. Arch Phys Med Rehabil 1992; 73: 803–806.
Stover SL, Gay RE, Koopman W, Sahgal V, Gale LL . Dermal fibrosis in spinal cord injury patients: a scleroderma variant? Arthritis Rheum 1980; 23: 1312–1317.
Rappl LM . Physiological changes in tissues denervated by spinal cord injury tissues and possible effects on wound healing. Int Wound J 2008; 5: 435–444.
Alexander MS, Biering-Sorensen F, Bodner D, Brackett NL, Cardenas D, Charlifue S et al. International standards to document remaining autonomic function after spinal cord injury. Spinal Cord 2009; 47: 36–43.
Sato K, Kang WH, Saga K, Sato KT . Biology of sweat glands and their disorders. I. Normal sweat gland function. J Am Acad Dermatol 1989; 20: 537–563.
Elsner P . Skin elasticity. In: Berardesca E, Elsner P, Wilhelm KP, Maibach HI (eds). Bioengineering of the skin: Methods and Instrumentation. CRC Pr: Boca Raton, 1995, pp 53–64.
Nedelec B, Correa JA, Rachelska G, Armour A, LaSalle L . Quantitative measurement of hypertrophic scar: interrater reliability and concurrent validity. J Burn Care Res 2008; 29: 501–511.
Barel AO, Courage W, Clarys P . Suction method for measurement of skin mechanical properties: the Cutometer. In: Serup J, Jemec GB (eds). Handbook of Non-Invasive Methods and the Skin, vol. 106. CRC Pr: Boca Raton, 1995, pp 335–340.
Smalls LK, Randall Wickett R, Visscher MO . Effect of dermal thickness, tissue composition, and body site on skin biomechanical properties. Skin Res Technol 2006; 12: 43–49.
Ryu HS, Joo YH, Kim SO, Park KC, Youn SW . Influence of age and regional differences on skin elasticity as measured by the Cutometer. Skin Res Technol 2008; 14: 354–358.
Dobrev HP . In vivo study of skin mechanical properties in psoriasis vulgaris. Acta Derm Venereol 2000; 80: 263–266.
Yoon HS, Baik SH, Oh CH . Quantitative measurement of desquamation and skin elasticity in diabetic patients. Skin Res Technol 2002; 8: 250–254.
Maynard Jr FM, Bracken MB, Creasey G, Ditunno Jr JF, Donovan WH, Ducker TB et al. International Standards for Neurological and Functional Classification of Spinal Cord Injury. American Spinal Injury Association. Spinal Cord 1997; 35: 266–274.
Thomas A . Les moyens d’exploration du systeme sympathique et leur valeur: Affections organiques du systeme nerveux. Rev Neurol 1926; 1: 767–928.
List CF, Pimenta AD . Sweat secretion in man: VI. Spinal reflex sweating. Arch of Neurol Psychiatry 1944; 51: 501–507.
Previnaire JG, Soler JM, El Masri W, Denys P . Assessment of the sympathetic level of lesion in patients with spinal cord injury. Spinal Cord 2009; 47: 122–127.
Ohry A, Rozin R . Clinical note on facies quadriplegiae. Paraplegia 1983; 21: 327.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Park, J., Seo, C., Han, S. et al. Sympathetic influence on biomechanical skin properties after spinal cord injury. Spinal Cord 49, 236–243 (2011). https://doi.org/10.1038/sc.2010.95
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2010.95