Abstract
Study design:
Cross-sectional, mail-back questionnaire study.
Objectives:
To describe women's experiences of sexual functioning and sex life after spinal cord injury (SCI).
Setting:
Sweden, Denmark, Norway, Finland, and Iceland.
Methods:
All community-living SCI women treated at spinal cord centres in Sweden, Denmark, Norway, Finland, and Iceland meeting inclusion criteria (n=963) were mailed the study-specific SCI Women Questionnaire. Out of the 532 respondents, 392 reported having had sex after injury and were thus included in the study. The included women had a mean age of 42 years (range 18–68) and a mean time since injury of 11 years (range 2–54).
Results:
The SCI women reported that the injury caused many changes in their sex life and affected many aspects of their sexuality negatively. Some changes were of a physical nature (for example, decreased, lost, or changed sensation; difficulties to achieve orgasm; bladder or bowel problems; and difficulties to move and position oneself) whereas other changes were of a psychological nature (for example, feeling unattractive or less attractive, having less self-confidence, and difficulties to meet or find a partner).
Conclusion:
Successful SCI rehabilitation requires a holistic approach, taking into account the patient's physical, psychological, and interpersonal circumstances. Given that many women with SCI remain sexually active but often experience less satisfaction after injury, it is important that rehabilitation efforts address this aspect of the patient's life. Our results elucidating strategies applied by women with SCI to compensate for loss of genital sensation and cope with physiological impairment during sexual activity may serve to help professionals in developing rehabilitation programmes for women with SCI.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) is a traumatic event that affects many facets of the injured person's life. One such aspect is sexual functioning.1 Sexual functioning is a fundamental aspect of health and well-being for all individuals. It should thus be addressed in all spinal units and rehabilitation centres and should be given the same consideration as other important issues.2 Nonetheless, previous research has shown that the majority of women with SCI are dissatisfied with the amount and quality of information about sexual functioning and sex life provided at these centres.3, 4, 5, 6 Comparatively, few studies have investigated the sexual functioning and sex life of SCI women, as opposed to that of SCI men; however, a general finding is that most SCI women continue to be sexually active after injury, but to a lesser extent than before injury.4, 5, 7, 8, 9, 10, 11 It has also been shown that many SCI women have difficulty becoming psychologically as well as physically aroused.12 Laboratory-based studies have provided detailed knowledge about how specific injury patterns affect specific aspects of the female sexual response.13
In-depth knowledge about how SCI women experience their sexual functioning and sex life may serve to improve the quality of information provided to these women, as well as to aid health professionals in their attempts to address the SCI women's sexual concerns. The purpose of this study was thus to describe SCI women's experiences of different aspects of sexual functioning and sex life after injury.
Methods
Study group
Names and addresses of 1011 women with SCI were provided by the heads of spinal cord centres in the five Nordic countries: Sweden (n=375), Denmark (n=163), Norway (n=215), Finland (n=236), and Iceland (n=22). Exclusion criteria were known recovery (Frankel Grade E/ASIA Impairment Scale E),14, 15 injured less than 2 years, brain injuries and psychiatric diseases, and inability to understand the Nordic language in question. The inclusion criterion was age between 18 and 70 years. Questionnaires with a letter describing the rationale for the study were mailed to the potential participants. They were guaranteed the complete confidentiality of their responses and were offered the possibility to return the questionnaires anonymously. Two reminders were sent to optimize the number of responses.
Out of the 1011 women, 52 were excluded: 4 because of death, 7 were recovered, 3 with language difficulties, 8 had congenital injuries, 3 because of psychiatric disease, 18 because of other severe illness, and 9 could not be located. The total eligible sample thus comprised 963 women.
Out of the 532 women who returned evaluable questionnaires (response rate 55%), 392 (73.7%) reported having had sex together with a partner after injury and were thus included in this study. Sociodemographic and clinical characteristics are given in Table 1.
Ethic considerations
The local ethics committees in the five Nordic countries approved the study. The ethic committees in Norway and Iceland approved the study under the condition that the questionnaires were to be returned anonymously. The ethics committees in Sweden, Denmark, and Finland did not make this stipulation; however, the women in these three countries were also given the option to return the questionnaires anonymously. The Swedish women were offered 100 Swedish Crowns (approximately 13 US dollars) for their participation, whereas the ethics committees in the other countries did not approve this kind of compensation.
Measurements
Sexual functioning and sexual life. The SCI Women Questionnaire (SCIWQ),5 comprising 104 items, was designed to assess different dimensions of sexuality. Details about the development of the SCIWQ are described elsewhere.5 Responses to 10 open-ended questions from the SCIWQ were analysed in this study.
Results
Changes in sex life after injury
Responses (n=356, 91%) to the question ‘Describe in your own words how your sex life has changed after the SCI’ were grouped as shown in Table 2. Changes of a physical, psychological, and practical nature were reported. Although most women reported that their sex life had been affected negatively, 7 women (2%) considered that it was better and of greater importance after the injury and 38 (11%) reported either no major changes or that their sex life functioned well. A total of 91 women (26%) had sex less frequently after injury, 45 women (13%) claimed that they had no or less sexual desire, need, or longing, and 27 claimed (8%) that they had difficulties to achieve orgasm. Twenty-five of the respondents (7%) reported that they had had no sexual experience before the injury, primarily because of young age, and therefore could not make retrospective comparisons.
How to compensate for decreased sensibility
Totally, 173 women (44%) answered the question ‘If you have impaired sensibility, can you then describe what you do to compensate for the decreased sensibility?’ As shown in Table 3, many women compensated by fantasizing and thinking about how sex was before the injury (n=51, 30%). Other ways to compensate for decreased sensibility included ‘kissing’, ‘touching’, and ‘caressing’ other erogenous zones than the genitals (n=38, 22%); ‘watching the act directly or with the help of a mirror’ (n=11, 6%); and ‘longer foreplay and stronger stimulation of the clitoris, and so on’ (n=9, 5%). Some (n=37, 21%) answered that they did nothing, did not know what to do, or could not do anything.
The experience of having an orgasm
Out of the 234 women who answered the question ‘If you have had orgasm, or something like orgasm after the injury, how would you describe that experience’, 19 women (8%) experienced orgasm in the same way as before the injury and 59 (25%) described it as ‘like being in heaven’, ‘flying’, and ‘unbelievable and very strong feelings’. Thirty-eight women (16%) felt that they had fewer orgasms, that it was more difficult and required more time to achieve orgasm or that it was weaker than before injury, whereas 31 (13%) mentioned that they were satisfied with the quality of their orgasms. Thirty-one women (31%) described their orgasms as ‘relaxing’, whereas others described them as a ‘vibrating, pulsating, shaking sensation’, or as a ‘pressure wave’ (n=16, 7%); ‘warm sensation’ (n=13, 6%), ‘like emptying the bladder’ (n=3, 1%), and ‘contractions’ (n=4, 2%). Negative sensations, such as pain, unpleasantness (n=7, 3%), cramps (n=7, 3%), spasticity (n=4, 2%), and automic dysreflexia and headache (n=6, 3%) were also experienced. Nineteen women (8%) stated that they did not experience anything like an orgasm.
The best thing the sexual partner can do
In response to the question ‘What is the best thing your sexual partner can do to help you to relax and enjoy sex?’ 104 women (38%) mentioned physical stimulation, such as ‘caressing’, ‘kissing’, ‘licking of areas with sensibility, ‘take your time’ and ‘long and good foreplay’ (n=39, 14%), and ‘massage’ (n=18, 7%), see Table 4. Many women considered that being shown ‘love’, ‘closeness’, ‘romance’, ‘tenderness’, and ‘warmth’ were of great importance, as were the partner showing ‘understanding’, ‘consideration’, ‘attention’, ‘honesty’, and ‘acceptance’.
Tips for improving sexual pleasure
Many women recounted ways that they found were helpful in improving their sexual relationship and/or sexual pleasure, see Table 5. The most frequently mentioned tips were that SCI women should openly discuss with their partner what they find pleasurable, what the partner can do to help them attain pleasure, and how they can experiment to compensate for physiological impairments (n=41). Other tips were that the partner should be ‘patient’, ‘respectful’, ‘understanding’, and ‘put the woman first’ (n=16). Other useful tips included ‘try to relax’, ‘use your fantasy’, ‘work with and try to accept your body image’, ‘experiment and explore’, and ‘use aids such as a vibrator, dildo, and massage apparatus’.
Partner's reaction to bladder or bowel leakage during sex
Out of the 206 women who answered the question ‘How has your partner reacted if you had leakage during sex’, 51 (25%) answered that the partner had reacted with understanding and had been supportive and positive. Others answered that the partner had ‘done nothing’, ‘made no comments’, or ‘did not react much’ (n=39, 19%). Some mentioned that they had ‘joked and laughed about it’ (n=10, 5%). Others reacted by ‘cleaning up’, ‘changing bed linen’, ‘bathing together’, ‘pointing out that washing machines exist’, or ‘reacting less than feared’ (n=10, 5%). Some had ‘considered it normal’, ‘reacted quietly and calmly’, and ‘been comforting’ (n=12, 6%). A total of 20 women (10%) reported that the partner had reacted negatively, becoming ‘frustrated’, ‘irritated’, ‘anxious’, ‘afraid’, ‘disgusted’, or ‘loosing interest as well as erection’. Sixty-two women (30%) answered that they had never experienced leakage during sex.
Ways to handle stomas and catheters during foreplay and intercourse
Of the 24 women who answered the question ‘How do you handle urostomy or colostomy during sexual togetherness’, most reported that they emptied the stoma bag before sexual activity. Other solutions were to ‘put on a new and clean bag’, ‘change the stoma bandage and use a body-dress’, ‘attach a little stop-bag’, and ‘empty and tape the bag’. To avoid a permanent urethral or suprapubic catheter from loosening, 11 women (46%) reported that they ‘tape the catheter to the stomach or thigh’ or ‘put it on the side’.
Birth control methods
Totally, 253 women answered the question regarding the use of birth control methods. Practiced birth control methods were p-pills (n=119, 47%), IUD—including hormones (n=81, 32%), condoms (n=80, 32%), sterilization (n=17, 7%), p-syringe (n=16, 6%), mini-pills (n=12, 5%), interrupted coitus (n=5, 2%), p-stick (n=2), safe periods (n=2), hysterectomized (n=2), preventive drug in capsule form (n=1), and day-after pills (n=1).
Discussion
This study showed that most women continue to be sexually active after their injury and that they consider sex to still be an important part of their lives. Although many aspects of their sexual functioning and sex life were negatively affected by the injury, the women in our study reported various means to compensate for the physiological impairments induced by the injury.
Some changes in the women's sexual functioning and sex life were primarily of a physical nature, such as decreased or lost sensation, difficulties to achieve orgasm, and to move and to position oneself. Other changes were of more a psychological nature, such as feeling unattractive or less attractive, less self-confidence, and difficulties to meet or find a partner. Many of the women had sex less frequently after injury; their willingness to engage in sexual activity was affected by bladder or bowel problems, pain, or other unpleasant feelings. The women emphasized the importance of talking openly and honestly with their partner about their sexual needs and desires and of the partner being understanding and sensitive to those needs. Other studies have shown that women with SCI are also concerned about their ability to satisfy their partner, to cope emotionally with changes in sexual functioning, and to help their partner cope emotionally with their sexual limitations.7
Owing to decreased or absent sensation below the level of injury, women with SCI may be unable to respond to the same sexual stimuli that had been pleasurable before injury and the physical stimuli generating subjective arousal may be insufficient.12 Many of the women in our study also reported decreased or absent sensation; however, many of the women compensated for this by fantasizing and thinking about how sex had been before the injury, engaging in longer foreplay and more powerful stimulation, relying on input from other senses and exploiting non-genital erogenous zones.
Sexual intercourse and caressing of the genitals were less important after injury. On the other hand, many of the women emphasized that caressing, kissing, licking, stimulation of areas with sensation, massage, and foreplay as the best their sexual partner could do for them to relax and enjoy sex. Many women also considered that being shown love, closeness, romance, tenderness, and warm feelings were of great importance, as were the partner's understanding, consideration, attention, honesty, and acceptance. Most of the women thought that hugging, kissing, and caressing (also body parts with no sensation) were essential and pleasurable ingredients of the sexual experience.
In agreement with other studies,6, 7 some of the women in our study reported that they could no longer experience orgasm. This may naturally be due to a total loss of sensation in the vagina and clitoris.12 On the other hand, most of those who were able to achieve orgasm described it either as very pleasurable or, in a small number of cases, as painful, unpleasant, and incomplete and therefore frustrating. Even if physiological orgasm for some is not possible, rewarding, or pleasant, the sexual experience may be completed by psychological satisfaction. A warm and close relationship and deep feelings of affection for the partner may compensate for not reaching orgasm during sexual activity. Many women stated that orgasm was less intense and took longer to achieve than before injury, and therefore highlighted the importance of their partner taking time and being considerate of their needs when making love. They also pointed out that memories and fantasies helped to enhance their pleasure. Increased time to achieve orgasm has also been found by Sipski et al.16
Urinary and/or bowel incontinence are a cause of great anxiety for women with SCI.3, 10, 17 A bladder or bowel accident may occur at any time and may be most embarrassing if it happens during sexual activity. Only about 10% of the women in our study reported that their partner had reacted negatively (irritated, frustrated, and so on) to such incidents and a few partners had lost interest in sex. However, there were considerably more partners that had reacted with understanding and consideration and some had even been able to joke about it. Certain practical measures were used to avoid ‘accidents’ during sexual togetherness, such as emptying the bladder or bag before sexual activity or taping the catheter to the stomach or thigh. The respondents stressed the importance of discussing these issues with their partner and sharing their feelings, anxieties, and fears.
As in any mail-back questionnaire study, there is a possibility that our sample was selective and hence may not be representative for the target population (SCI women in the Nordic countries). Possible reasons for non-response are that some women may be too embarrassed to answer questions about their sex life or that women with a poor and unsatisfying sexual life may feel less motivated to answer questions than do those with an active and satisfying sex life. However, our sample was heterogeneous, encompassing a wide range of ages, length of times since injury, neurological status, and marital status, and therefore we believe the experiences expressed by this sample are salient to women with SCI.
Issues relating to sexual functioning and sex life in women after SCI have received relatively little attention in the scientific literature or in clinical rehabilitation efforts. If the goal of rehabilitation is to restore the injured person as fully as possible to their premorbid level of functioning, this must apply to sexuality as well. It is important that all staff have adequate knowledge about sexual functioning after SCI and feel comfortable raising the issue of sexuality to allow the patients opportunities to discuss this topic. Sex information/education programmes should be an integral component of the rehabilitation and during life-long follow-up because sexually related needs and concerns might change over time. The many tips from the women in this study to compensate for the physiological impairments induced by the injury should be communicated in these programmes. Our results are supported by the suggestions for information provided in the ‘Clinical Practical Guidelines on Sexuality and Reproductive Health for Adults with SCI’ published by the Consortium for Spinal Cord Medicine.18
Conclusions
Successful SCI rehabilitation requires a holistic approach, taking into account the patient's physical, psychological, and interpersonal circumstances. Given that many women with SCI remain sexually active but often experience less satisfaction after injury, it is important that rehabilitation efforts address this important aspect of the patient's life. Our results elucidating strategies applied by women with SCI to compensate for loss of genital sensation and cope with physiological impairment during sexual activity may serve to help professionals in developing rehabilitation programmes for women with SCI.
References
Trieschman RB . Spinal Cord Injuries. Psychological, Social and Vocational Rehabilitation. Demos Publication: New York, 1988.
Esmail S, Knox H, Scott H . Sexuality and the role of the rehabilitation professional. In: Stone JH, Blouin M (eds). International Encyclopedia of Rehabilitation. Center for International Research and Exchange (CIRRIE): Buffalo, New York, 2010.
Charliefue SW, Gerhart KA, Menter RR, Whiteneck GG, Scott Manley M . Sexual issues of women with spinal cord injuries. Paraplegia 1992; 30: 192–199.
Richard E, Tepper M, Whipple B, Komisaruk BR . Women with complete spinal cord injury: a phenomenological study of sexuality and relationship experiences. Sex Disabil 1997; 15: 271–283.
Kreuter M, Siösteen A, Biering-Sørensen F . Sexuality and sexual life in women with spinal cord injury: a controlled study. J Rehabil Med 2008; 40: 61–69.
Forsythe E, Horsewell JE . Sexual rehabilitation of women with a spinal cord injury. Spinal Cord 2006; 44: 234–241.
Ferreiro-Velasco ME, Barca-Buyo A, de la Barrera SS, Montoto-Marques A, Vazquez XM, Rodriguez-Sotillo A . Sexual issues in a sample of women with spinal cord injury. Spinal Cord 2005; 43: 51–55.
Sipski ML, Alexander CJ . Sexual activities, response and satisfaction in women pre- and post spinal cord injury. Arch Phys Med Rehabil 1993; 74: 1025–1029.
White M, Rintala D, Hart KA, Fuhrer MJ . Sexual activities, concerns and interests of women with spinal cord injury living in the community. Am J Phys Med Rehabil 1993; 72: 372–378.
Jackson AB, Wadley V . A multicenter study of women's self-reported reproductive health after spinal cord injury. Arch Phys Med Rehabil 1999; 80: 1420–1428.
Matzaroglou C, Assimakopoulos K, Panagiotopoulos E, Kasimatis G, Dimakopoulos P, Lambiris E . Sexual function in females with severe cervical spinal cord injuries: a controlled study with the Female Sexual Function Index. Int J Rehabil Res 2005; 28: 375–377.
Anderson KD, Borisoff JF, Johnson RD, Stiens SA, Elliot SL . Spinal cord injury influences psychogenic as well as physical components of female sexual ability. Spinal Cord 2007; 45: 349–359.
Sipski ML, Arenas A . Female sexual function after spinal cord injury. Prog Brain Res 2006; 152: 441–447.
Frankel HL, Hancock DO, Hyslop G, Melzak J, Michaelis LS, Ungar GH et al. The value of postural reduction in the initial management of closed injuries in the spine with paraplegia and tetraplegia. Paraplegia 1969; 7: 179–192.
Marino RJ, Barros T, Biering-Sørensen F, Burns SP, Donovan WH, Graves DE et al. International standards for neurological classification of spinal cord injury. J Spinal Cord Med 2003; 26: 50–56.
Sipski ML, Alexander CJ, Rosen R . Sexual arousal and orgasm in women: effects of spinal cord injury. Ann Neurol 2009; 49: 35–44.
Westgren N, Hultling C, Levi R, Seiger̊, Westgren M . Sexuality in women with a traumatic spinal cord injury. Acta Obstet Gynecol Scand 1997; 76: 977–983.
Ducharme S, Kewman DG, Chase T, Creasey G, Elliot SL, Goetz LL et al. Clinical Practice Guidelines: Sexuality and Reproductive Health in Adults with Spinal Cord Injury: A Clinical Practice Guidlines for Health Care Professionals. Consortium for Spinal Cord Medicine. Paralyzed Veterans of America, 2010, 1–47.
Acknowledgements
We thank the heads of the spinal cord centres in the Nordic countries for providing the names and addresses for the women with SCI. Above all else, we express our sincere thanks to all women participating in the study and to the women in the kNORR (kNORR was formed in 2001 to draw attention to the particular problems confronting women with SCI. The members of kNORR are women with SCI living in the Nordic countries) for initiating this study and for their input in developing the questionnaire. This work was supported by grants from Swedish National Associations of People Disabled by Road Accidents and Polio (RTP), Norrbacka-Eugenia Foundation, the Association of Cancer and Road Accident Victims (CTRF), Sweden, Landsforeningen af Polio-, Trafik–og Ulykkesskadede ( PTU), and Bevica Foundation (previously Sahva Foundation), Denmark.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kreuter, M., Taft, C., Siösteen, A. et al. Women's sexual functioning and sex life after spinal cord injury. Spinal Cord 49, 154–160 (2011). https://doi.org/10.1038/sc.2010.51
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2010.51
Keywords
This article is cited by
-
A Scoping Review of Literature on Sexual Health and Wellness in Women with Spinal Cord Injury
Sexuality and Disability (2024)
-
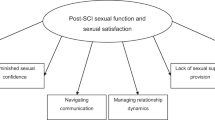
“You feel a bit unsexy sometimes”: The psychosocial impact of a spinal cord injury on sexual function and sexual satisfaction
Spinal Cord (2023)
-
Sexuality After Spinal Cord Injury. Which Factors Influence Sexual Activity and Satisfaction?
Sexuality and Disability (2022)
-
Sexual and Reproductive Health Experiences, Knowledge and Associations: A Neglected Issue Among Adults with Spinal Cord Injury in Sri Lanka
Sexuality and Disability (2022)
-
Evaluation of sexual reproductive health needs of women with spinal cord injury in Tehran, Iran
Sexuality and Disability (2022)