Abstract
Background:
Information on the characteristics of pneumonia in long-term ventilator-assisted individuals is scarce. We evaluate the incidence, risk factors and outcome of ventilator-associated pneumonia (VAP) in a large series of chronically ventilated patients.
Methods:
All patients assisted in a chronic ventilator-dependent unit were prospectively followed up for the development of VAP. Patients with a new and persistent lung infiltrate and a purulent tracheal aspirate were suspected to have VAP. Pneumonia was considered microbiologically confirmed in the presence of (1) a positive blood culture and/or (2) ⩾105 CFU ml−1 in quantitative bacterial culture of tracheal aspirates or ⩾103 CFU ml−1 in quantitative mini-bronchoalveolar lavage cultures.
Results:
In total, 100 consecutive long-term ventilated individuals with spinal cord injury (mean age 49 years) were prospectively followed up. The length of mechanical ventilation before admission in the unit was 54±37 days, and the follow-up after admission was 119±127 days. There were 32 episodes of VAP in 27 patients (1.74 episodes per 1000 days of mechanical ventilation). By logistic regression analysis, hypoalbuminaemia (P=0.03), administration of antacids (P=0.002) and length of mechanical ventilation (P=0.05) were independent risk factors for VAP. The most frequently isolated organisms were Pseudomonas aeruginosa (62%), methicillin-resistant Staphylococcus aureus (25%) and Acinetobacter baumannii (15%); 9 (28%) episodes were polymicrobial. Antimicrobial treatment, including monotherapy in 66%, was successful in most patients. Only three patients (11%) died in relation to VAP.
Conclusions:
Patients on long-term ventilation are at significant risk for the development of VAP, but the mortality is low.
Similar content being viewed by others
Introduction
Ventilator-associated pneumonia (VAP) is a frequent complication of mechanical ventilation. Its rate of occurrence ranges from 10 to 70% depending on the population studied and on the criteria used to establish the diagnosis.1 The clinical importance of VAP is demonstrated by several investigations, suggesting that its occurrence is an independent determinant of mortality for critically ill patients requiring mechanical ventilation.2, 3 Crude mortality rates vary from 25 to 50%, whereas directly attributable mortality is 27%.4 In patients who receive mechanical ventilation, 5% remain unweanable after 4 weeks and have been classified as chronic ventilator-dependent patients. It is more appropriate to refer to these patients as long-term ventilated-associated individuals.5
Acute spinal cord injury is a devastating event whose incidence varies from country to country, according to cause, methodology applied, and national and local database registries.6 In the United States, its incidence ranges from 28 to 50 injuries per million persons per year.7 In other parts of the world, the incidence varies from 10 to 83 injuries per million persons per year.6 Patients with cervical spinal cord injuries have respiratory dysfunction and are unable to sustain spontaneous breathing, which predisposes them to respiratory complications and respiratory failure. Pulmonary complications are the leading cause of death in this population, with most respiratory death attributed to pneumonia.8, 9 In the last 15 years, there has been an increase in the incidence of patients with high-level quadriplegia (C1–C4) and represent approximately one-third of the patients with spinal cord injury, and 50% of them have a complete lesion.6, 8 Most of them require mechanical ventilation either temporary or permanently.
The overall number of patients who administered long-term mechanical ventilation has progressively increased, because of advances in medical care. In the United States, the incidence of long-term ventilator-assisted individuals increased from 11 419 cases per year in 1990 to 43 700 cases per year in 1998.10 Most of the studies that analyze the clinical and epidemiological characteristics of VAP refer to patients receiving mechanical ventilation for periods of <4 weeks.1, 2 Very few studies have analyzed these characteristics in patients with long-term ventilator-assisted individuals,11, 12 and to our knowledge, the overall characteristics of VAP has never been evaluated in this group of patients. In this study, we aimed to analyze the incidence, chronology, risk factors and the outcome of VAP in long-term ventilator-assisted individuals.
Materials and methods
Setting, patient selection and study design
Our hospital is a 227-bed institution for spinal cord-injured patients, including a 6-bed intensive care unit, and a chronic ventilator-dependent unit with 16 beds. In general, patients are usually admitted in this hospital within 60 days of injury.
In this study, we prospectively evaluated a cohort of long-term ventilator-assisted individuals. Inclusion criteria included patients ventilated for >30 days. The neurological level for this analysis was stratified into five groups: (1) C1-bulbar, (2) C2, (3) C3–C4, (4) C5–C8 and (5) dorsal. Patients were classified into two categories according to the cause of spinal cord injury (medical and traumatic). The following information was recorded: patient's age, sex, severity of underlying medical condition stratified as rapidly fatal, ultimately fatal or not fatal, according to the criteria of McCabe and Jackson,13 and comorbidities. Potential risk factors for VAP at the time of admission and in each episode of pneumonia were also recorded and included intensive care unit stay duration, recent infection, use of a nasogastric tube, gastrostomy tube, endotracheal tube, administration of histamine-2-receptor antagonists, antacids, enteral nutrition, parenteral nutrition, witnessed aspiration, preexisting pulmonary disease, nonpharmacological consciousness depression or coma, sedative agents, bronchoscopy, administration of previous antibiotics, duration of mechanical ventilation and administration of steroids. Other variables measured included serum albumin on admission, presence of anaemia, reintubation, stress ulcer, decubitus ulcer and deglutition disorders. All patients were prospectively and daily followed up by one of the investigators who recorded any relevant data until they were successfully weaned from mechanical ventilation, discharged from the hospital while receiving mechanical ventilation or until death.
Clinical diagnosis of VAP
Clinical suspicion of VAP was defined by a new and persistent infiltrate on chest radiography associated with at least one of the following: purulent tracheal secretions, body temperature of at least 38.3 °C and leukocytosis.1 In addition, other baseline variables were recorded: body temperature, leukocyte count and severity of pneumonia (mild, moderate or severe). The assessment of acute lung injury included evaluation of the chest radiograph and arterial oxygenation using the PaO2/FiO2 coefficient (partial pressure of arterial oxygen to the fraction of inspired oxygen).2 We defined the presence of the acute respiratory distress syndrome as the presence of a generalized pulmonary infiltrate and a lung injury score >2.5,14 and the presence of shock as systolic arterial pressure of <90 mm Hg with signs of peripheral hypoperfusion or need for continuous infusion of vasopressor or inotropic agents.
Microbiological diagnosis of VAP
In all patients, three blood cultures were obtained. Tracheobronchial aspirates (TBAs) and/or mini-bronchoalveolar lavages (mini-BALs) were routinely obtained when VAP was clinically suspected. In addition, TBAs were also taken every 15 days in all patients to evaluate bacterial colonization of the lower respiratory tract. TBAs were obtained by sterile means using a Lukens suction catheter and collected in a mucus collector (Sherwood Medical, Tullamore, Ireland). Mini-BALs were carried out with a single-sheathed, plugged, telescoping catheter. A 50-cm sterile catheter with a 1.7 mm internal diameter occluded by a polyethylene glycol plug (Combicath, Plastimed, Saint-Leu-La-Forêt, France) was inserted into the distal airways and wedged in a peripheral bronchus. The plug was expelled with 10 ml of air, and a second sterile catheter (58 cm in length, 0.8 mm internal diameter) was then passed through the first catheter and advanced to the sample site. A 20 ml aliquot of physiological saline was injected through the internal catheter, and at least 2 ml was suctioned for microbiological examination. Respiratory samples were considered purulent if a Gram stain showed >25 neutrophils per high-power field. TBAs and mini-BALs were cultured by quantitative methods.15 In both samples, serial dilutions performed in sterile saline were inoculated into the following agar media: 5% sheep blood, chocolate and Sabouraud dextrose. All cultures were incubated at 37 °C under aerobic (sheep blood and Sabouraud dextrose) and 5% CO2-enriched (chocolate agar) atmosphere. Identification of microorganisms and antimicrobial susceptibility testing were carried out using an automated method (MicroScan, Siemens, CA, USA). Susceptibility breakpoints were determined following the CLSI guidelines.16 Microbiologically confirmed cases of VAP required the isolation of bacteria in significant quantities: ⩾105 CFU ml−1 for TBAs, and ⩾103 CFU ml−1 for mini-BAL samples.15
Definitions
We considered an episode of microbiologically confirmed pneumonia when there was a clinical suspicion of VAP in addition to a positive blood culture and/or a significant bacterial culture in TBAs and/or in mini-BAL. We considered tracheal colonization when the TBAs culture was positive in the absence of clinical signs of lower respiratory tract infection and persistent colonization was defined as the isolation of the same bacterial species in three or more consecutive cultures.
Initial choice of antibiotics was based on the results of the Gram stain of the TBAs, on the results of the bacterial growth in colonized patients and on the recommendations of the American Thoracic Society for hospital-acquired pneumonia.1 Results of quantitative cultures were used to adjust therapy.
Mortality directly related to VAP was predetermined to be present when a patient died during an episode of nosocomial pneumonia and the death could not be directly attributed to any other cause.
Statistical analysis
Results are expressed as mean±s.d. Differences between categorical variables were assessed by χ2-test (Fisher's exact test when appropriate). Continuous variables were compared by Mann–Whitney U-test. To analyze the effect of risk factors and pneumonia, we used multivariate analysis using logistic regression including all variables found to be significantly associated with VAP by univariate analysis (P<0.05). Data were processed by STATA 8.0.
Results
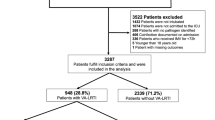
A total of 100 consecutive long-term ventilator-assisted patients were enrolled in the study. The patients (25 women and 75 men) had a mean age (±s.d.) of 49 (±17) years. In all, 67% had a nonfatal underlying disease, 32% ultimately fatal and 1% a rapidly fatal disease. The most frequent comorbid illnesses were diabetes (11%) and high blood pressure (17%), whereas 42% of the patients did not present any associated disease. The spinal cord injury level was traumatic in 74% and the level was above C4 in 58%. All patients had a tracheostomy and were followed up for 119±127 (10–524) days. The total length of stay in the intensive care unit was 52±36 days, and the total length of mechanical ventilation at admission was 54±37 days. A total of 65 patients presented persistent colonization, which was caused in the majority of cases (61%; 40 cases) by Pseudomonas aeruginosa. All patients included in the study had received broad-spectrum antimicrobial therapy at different times during their admission.
During the study period, 32 episodes of VAP were diagnosed in 27 patients (27%); 5 patients had more than one episode. The incidence of pneumonia in the population studied was 6.3 cases per 100 patients per year and the density of incidence was 1.74 per 1000 days of mechanical ventilation.
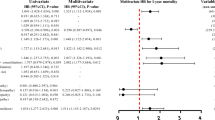
In univariate analysis, factors significantly associated with an increased risk of VAP included underlying disease, anaemia, hypoalbuminaemia, previous use of antacids, low level of consciousness, previous pulmonary disease and duration of mechanical ventilation (Table 1). By regression logistic analysis, hypoalbuminaemia (P=0.03), previous use of antacids (P=0.002) and duration of mechanical ventilation (P=0.05) were independently associated with an increased risk of VAP.
Clinical characteristics of the patients with pneumonia and the outcome are shown in Table 2. Only three patients presented bacteraemia, and the observed attributable mortality rate was 11%. Chest X-ray findings included unilateral alveolar infiltrates (34%) and bilateral alveolar infiltrates (63%). One chest X-ray was compatible with respiratory distress (3%).
In all 32 episodes of pneumonia, the Gram stain of the TBAs and/or mini-BAL samples revealed the presence of microorganisms. Significant counts of TBAs cultures were observed in 31 out of the 32 episodes of pneumonia and in 18 out of the 22 mini-BAL samples that were cultured. A total of 49 microorganisms were cultured from TBAs and/or mini-BAL in the 32 episodes of pneumonia (1.5 microorganisms per pneumonia). The most frequently isolated microorganisms were P. aeruginosa (62%), methicillin-resistant Staphylococcus aureus (25%) and Acinetobacter baumannii (12%). Nine (28%) episodes were polymicrobial, and three patients with persistent colonization by P. aeruginosa presented recurrent episodes of VAP (Table 3).
All patients were eventually treated with an appropriate antibiotic regimen that was active against the bacteria isolated from their respiratory secretions. Empirical therapy always included an antimicrobial regimen with antipseudomonal activity. Monotherapy was administered to 21 patients (17 with monomicrobial pneumonia and 4 with polymicrobial pneumonia) and 18 of them presented a favourable evolution (86%).
Discussion
Our study shows a significant rate of occurrence of VAP in long-term ventilated patients (27% with an incidence of 6.3 cases per 100 patient-years). However, in contrast to what could be expected, patients seldom require intensive care and the evolution is favourable with a low rate of attributable mortality.
There is scarce information on the frequency of development of VAP in long-term ventilated individuals. Jackson and Groomes17 reported that 63% of patients with C1–C4 quadriplegia developed pneumonia. In a short series of 37 long-term ventilated patients, 57% developed VAP.11 These higher frequencies in comparison with our study could be due to the low number of patients included in these series, and because of differences in underlying diseases and in study designs.
We have had the opportunity to evaluate risk factors associated with VAP in this population. The length of mechanical ventilation was an independent factor associated to VAP, similar to other studies findings.11 In the study of Fagon et al.,4 each day that the patient received endotracheal intubation and mechanical ventilation, the crude rate of VAP increased by 1–3% and the risk of death increased 2- to 10-fold. In long-term ventilation, a single study found a daily incidence of 0.002 VAP per ventilator day,18 which is very similar to our own results (1.74 per 1000 days). Antacids was another factor associated with an increased risk of VAP. Antacids are commonly used for prophylaxis against stress gastritis and ulceration, but may increase the frequency of gastric colonization by enteric Gram-negative bacilli and possibly the incidence of pneumonia. The third independent risk factor independently associated with VAP in our study was hypoalbuminaemia, a characteristic frequently found in patients with chronic conditions.19
As indicated above, the most frequently isolated microorganisms producing VAP were P. aeruginosa, methicillin-resistant S. aureus and A. baumannii. Persistent colonization was found in a high proportion of patients infected with P. aeruginosa, and after the first episode of pneumonia caused by this organism, three patients had a recurrent episode. This could be explained by the fact that this microorganism can be directly inoculated into the tracheobronchial tree without first appearing in the oropharyngeal secretions of intubated patients.19 In a prospective study, the frequency and etiology of pneumonia was directly influenced by previous antibiotic therapy.3 The high incidence of infections due to P. aeruginosa, methicillin-resistant S. aureus and A. baumannii in our series could be due to the previous use of antimicrobials in all patients. Another factor that explains the high incidence of infections due to these microorganisms is the length of mechanical ventilation. Trouillet et al.20 showed that the cumulative risk for pneumonia caused by Acinetobacter spp. was 3.4% at 10 days, 20% at 20 days and 48% at 30 days after the onset of mechanical ventilation and therefore was increasing nonlinearly with the duration of ventilation. This risk was similar to the risk for ventilator-associated pneumonia caused by P. aeruginosa. The 28% of polymicrobial infections reported herein is in agreement with previous data from intensive care unit patients ventilated for >48 h, in which 40–62% of whom developed polymicrobial pneumonia.20
In our study, monotherapy with only one effective antimicrobial agent resulted in a favourable outcome. Current consensus suggest that patients with suspected VAP should initially be treated with a broad-spectrum antibiotic regimen aimed at covering all likely bacterial pathogens. This regimen should subsequently be narrowed, according to the results of cultures of microbiological samples and their sensitivity profiles. Initial use of combination therapy reduces the likelihood of inappropriate therapy, and has been recommended to avoid the emergence of antimicrobial resistance and to enhance the killing produced by antimicrobials acting synergistically, particularly against VAP produced by P. aeruginosa.2 However, Garnacho-Montero et al.21 demonstrated that monotherapy with only one active antibiotic provided similar outcomes compared with combination therapy with two active antimicrobials, and suggested that switching to monotherapy once the susceptibility is documented was feasible and safe even against P. aeruginosa.
Several studies have suggested that the mortality attributable to VAP, particularly late-onset infection with antibiotic-resistant pathogens, is >10%.5, 6, 18 Crude mortality rates of 30–75% have been reported for nosocomial pneumonia caused by P. aeruginosa and/or Acinetobacter spp. with the highest rates reported in ventilator-dependent patients.22 In a short series of long-term ventilated patients, VAP was associated with a high mortality rate (56%).11 In our study, the rate of attributable mortality was low (11%).
In summary, we have found that the incidence of VAP in long-term ventilator-assisted patients is significant, although lower than it has been estimated in a few reports. Both the incidence of bacteraemia and the mortality are low, even when the majority of the causal microorganisms were multiresistant. In general, the outcome was favourable with monotherapy with only one active antimicrobial as a consequence of the surveillance and the optimization of the microbiology laboratory resources. The length of mechanical ventilation, previous use of antacid drugs and hypoalbuminaemia are the main risk factors associated with VAP and select a subgroup of patients predisposed to develop this infection.
References
American Thoracic Society Documents. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med 2005; 171: 388–416.
Doyle RL, Szaflarski N, Modin GW, Wiener-Kronish JP, Mattahay MA . Identification of patients with acute lung injury. Predictors of mortality. Am J Respir Crit Care Med 1995; 152: 1818–1824.
Fagon JY, Chastre J, Domart Y, Trouillet JL, Gibert C . Mortality due to ventilator-associated pneumonia or colonization with Pseudomonas or Acinetobacter species: assessment by quantitative culture of samples obtained by a protected specimen brush. Clin Infect Dis 1996; 23: 538–542.
Fagon JY, Chastre J, Hance AJ, Montravers P, Novara A, Gibert C . Nosocomial pneumonia in ventilated patients: a cohort study evaluating attributable mortality and hospital stay. Am J Med 1993; 94: 281–288.
Make BJ, Hill NS, Goldberg AI, Bach JR, Dunne PE, Heffner JE et al. Mechanical ventilation beyond the intensive care unit. Report of a Consensus Conference of the American College of Chest Physicians. Chest 1998; 113: 289S–344S.
Wyndaele M, Wyndaele JJ . Incidence, prevalence and epidemiology of spinal cord injury: what learns a worldwide literature survey? Spinal Cord 2006; 44: 523–529.
Ergas Z . Spinal cord injury in the United States: a statistical update. Cent Nerv Syst Trauma 1985; 2: 19–32.
Wicks AB, Menter RR . Long-term outlook in quadriplegic patients with initial ventilator dependency. Chest 1986; 90: 406–410.
Cardenas DD, Hoffman JM, Kirshblum S, McKinley W . Etiology and incidence of rehospitalization after traumatic spinal cord injury: a multicenter analysis. Arch Phys Med Rehabil 2004; 85: 1757–1763.
MacIntyre NR, Epstein SK, Carson S, Scheinhorn D, Christopher K, Muldoon S . Management of patients requiring prolonged mechanical ventilation. Report of a NAMDRC Consensus Conference. Chest 2005; 128: 3937–3954.
Kobashi Y, Matsushima T . Clinical analysis of patients requiring long-term mechanical ventilation of over three months: ventilator-associated pneumonia as a primary complication. Intern Med 2003; 42: 25–32.
De Vivo MJ, Ivie III CS . Life expectancy of ventilator-dependent persons with spinal cord injuries. Chest 1995; 108: 226–232.
McCabe WR, Jackson GG . Gram-negative bacteremia, I. Arch Intern Med 1982; 110: 847–864.
Murray JF, Matthay MA, Luce JM, Flick MR . An expanded definition of the adult respiratory distress syndrome. Am Rev Respir Dis 1988; 138: 720–723.
Kollef MH, Bock KR, Richards RD, Hearns ML . The safety and diagnostic accuracy of minibronchoalveolar lavage in patients with suspected ventilator-associated pneumonia. Ann Intern Med 1995; 122: 743–748.
Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing; eighteenth informational supplement. 2008. M-100-S18. Clinical and Laboratory Standards Institute, Wayne, PA.
Jackson AB, Groomes TE . Incidence of respiratory complications following spinal cord injury. Arch Phys Med Rehabil 1994; 75: 270–275.
Baram D, Hulse G, Palmer L . Stable patients receiving prolonged mechanical ventilation have a high alveolar burden of bacteria. Chest 2005; 127: 1353–1357.
Niederman MS, Mantovani R, Schoch P, Papas J, Fein M . Patterns and routes of tracheobronchial colonization in mechanically ventilated patients: the role of nutritional status in colonization of the lower airway by Pseudomonas species. Chest 1989; 95: 155–161.
Trouillet JL, Chastre J, Vuagnat A, Jolly-Guillow ML, Combaux D, Dombret MC et al. Ventilator-associated pneumonia caused by potentially drug-resistant bacteria. Am J Respir Crit Care Med 1998; 157: 531–539.
Garnacho-Montero J, Sa-Borges M, Sole-Violan J, Barcenilla F, Escoresca-Ortega A, Ochoa M et al. Optimal management therapy for Pseudomonas aeruginosa ventilator-associated pneumonia: an observational, multicenter study comparing monotherapy with combination antibiotic therapy. Crit Care Med 2007; 35: 1888–1895.
Luna CM, Vujacich P, Niederman MS, Vay C, Gherardi C, Matera J et al. Impact of BAL data on the therapy and outcome of ventilator associated pneumonia. Chest 1997; 111: 676–685.
Acknowledgements
We thank José Luis Rodríguez Martín and Teresa Seoane (Area de Investigación Clínica, SESCAM) for assistance with the statistical analysis. This work was supported, in part, by a grant from the Spanish Social Security Health Investigation Fund (FISS 01/0359).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
García-Leoni, M., Moreno, S., García-Garrote, F. et al. Ventilator-associated pneumonia in long-term ventilator-assisted individuals. Spinal Cord 48, 876–880 (2010). https://doi.org/10.1038/sc.2010.43
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2010.43