Abstract
Study design:
Crossover trial.
Objectives:
To investigate the effects of whole-body vibration (WBV) on muscular activity and blood flow velocity after different vibration treatments in patients with spinal cord injury (SCI).
Setting:
Research Center on Physical Disability (Spain).
Methods:
Eight individuals with SCI received six 3-min WBV treatments depending on a combination of frequency (10, 20 or 30 Hz) and protocol (constant, that is, three consecutive minutes of WBV, or fragmented, that is, three sets of 1 min of WBV with 1 min of rest between the sets). Femoral artery blood flow velocity was registered at minutes 1, 2 and 3 of WBV, and at minutes 1 and 2 after the end of the stimulus. Electromyography activity (EMG) of vastus lateralis (VL) and vastus medialis (VM) was registered at baseline and during WBV.
Results:
Peak blood velocity (PBV) increased after 1, 2 and 3 min of WBV. The 10 Hz frequency did not alter blood flow, whereas the 20 Hz frequency increased PBV after 2 and 3 min of WBV, and the 30 Hz frequency increased PBV after 1, 2 and 3 min of WBV and during the first minute after the end of the stimulus. No protocol effect was observed for blood parameters. EMG activity of VL and VM increased independently of the applied frequency or protocol.
Conclusion:
WBV is an effective method to increase leg blood flow and to activate muscle mass in SCI patients, and could be considered to be incorporated in their rehabilitation programs.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) has muscular and vascular consequences below the level of the injury.1 Regarding muscular changes, these patients suffer a dramatic loss of muscle mass.2 Immediately after the injury and in the following months, there is a preferential atrophy of type 2 fibers, but past 7–10 months post injury, a significant shift of type 1 fibers to type 2B has been observed.3 Regarding vascular changes, there is a reduction in the thigh blood flow,4 femoral artery diameter,1 vascular reactivity,1 and capillary alterations.3 It has been proposed that changes in the muscle vascular function are parallel to the skeletal muscle atrophy in SCI subjects,1 and both changes increase the risk of cardiovascular disease5 and the development of pressure ulcers.6 Therefore, part of the rehabilitation of SCI patients should focus on the activation of muscular and vascular systems.4
The application of whole-body vibration (WBV) with platforms has been shown to improve muscular7, 8 and vascular9, 10, 11 functions. These effects are strongly dependent on the type of platform, protocols and vibration parameters (that is, frequency).7 Specifically, greater vibration frequencies induce higher-muscle activity8 and greater blood flow11 than lower frequencies. Moreover, the most common protocol used to apply WBV consists of short bouts (30–90 s) with ∼60 s rest between the sets. The effects induced by the application of longer bouts (3 min) on peripheral circulation have been poorly investigated.
The previously mentioned benefits of WBV have been observed in healthy subjects; however, no study has focused on the effects of WBV on the muscle and vascular responses of SCI patients. Thus, the purpose of this study was to investigate the effects of WBV on muscular activity and blood flow velocity after different vibration treatments in SCI patients.
Materials and methods
Subjects
Eight patients (six males and two females) volunteered to participate in the study. All the patients had SCI and used wheelchair for their locomotion. All the subjects were clasiffied by the American Spinal Injury Association (ASIA) as A. Table 1 summarizes the characteristics of the sample. All the subjects received rehabilitation ten 2-h sessions per month, which consisted of standing position (or tilt position), passive movements, low intensity resistance training or electrotherapy, and physiotherapy treatment. Experimental treatments were applied to the subjects before their rehabilitation routines. Subjects did not allow their sleeping, eating and drinking habits to change throughout study participation. We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Experimental design
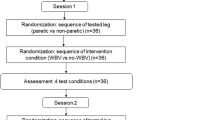
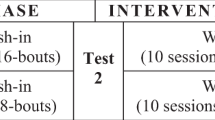
Each subject was assessed in eight different sessions. In the first two sessions, subjects were familiarized with the testing treatments and vibration stimulus. Both sessions were carried out within the same week separated with at least 48 h. The other six sessions were carried out on Monday, Wednesday and Friday during the following two weeks. In each session, a random WBV treatment was applied. The six WBV treatments arise from the combination of the independent variables frequency (10, 20 or 30 Hz) and protocol (constant or fragmented). WBV was applied for three consecutive minutes during the constant protocol, whereas three cycles of 1 min of WBV and 1 min of resting period were applied during the fragmented protocol (Figure 1).
Treatment protocol
Once a subject came to the laboratory, he or she was laid down and fixed to a tilt table with straps (Figure 2). In the distal part of the tilt table, just beneath the feet, a vibration platform was placed (Galileo Home, Galileo, Novotec, Germany). Knee angle was of 60° flexion (considering 0° the full knee extension). Subsequently, the tilt table was placed at 45° and the subject was kept in that position for a period of 10 min before the application of WBV. All the subjects were familiarized with the tilt table and the chosen angle as they usually maintain this position in their rehabilitation routines. In that position, the subject was prepared to register electromyography activity (EMG) and ultrasound variables. The frequency of vibration was set at 10, 20 or 30 Hz. The amplitude of the vibration was set by the position of the feet on the WBV plate at 5 mm (peak–peak). Feet were placed parallel to each other 38 cm apart (measured from the midlines of the feet). The patients were exposed to the vibration each day for a total of 3 min continuous (constant) or fragmented (three bouts 60 s exposures, separated by 60 s rests).
Ultrasound measurements
Blood parameters were registered through an ultrasound system (MyLab 25, Esaote, Genoa, Italy) using a pulsed color Doppler with a linear array transducer (LA 523, 7.5–12 MHz; length, 50 mm; Esaote, Genua, Italy) in the femoral artery as previously described.11 Blood parameters were analyzed at baseline, at the end of minutes 1, 2 and 3 of WBV, and at the end of minutes 1 and 2 of recovery after the stop of WBV (Figure 1). Each image recorded by the ultrasound system corresponded to a period of 4 s. In that period, there were between 3 and 5 beats, and the mean of these beats was analyzed to obtain: mean and peak systolic blood velocities (MBV and PBV, respectively), as well as heart rate.
Surface electromyographic activity
Muscle activity of the vastus medialis (VM) and vastus lateralis (VL) was measured using EMG. One set (two measuring electrodes) of surface electrodes (Ag/AgCl, Skintact, Innsbruck, Austria) was placed longitudinally to the direction of the muscle fibers and approximately halfway from the motor point area to the distal part of the muscle. An inter-electrode distance of 2 cm was maintained. Before electrode placement, the area was shaved, abraded and cleaned with isopropyl alcohol in order to reduce skin impedance until it was lower than 5 kΩ. The location of the electrodes on the skin was marked with permanent ink in order to ensure the same placement throughout the different sessions.
Myoelectric raw signals were detected with a two-channel EMG device (MyoTrac Infiniti, Thought Technology, Montréal, Canada). EMG data analysis was performed with a specific software (BioGraph Infiniti, Thought Technology, Montréal, Canada). The last 10 s corresponding to the control period and corresponding to the third minute of WBV application were chosen for data analysis by the aforementioned software (Figure 1). EMG raw data was averaged by root mean square (EMGRMS) in order to obtain the average amplitude of the EMG signal. On the basis of the frequency analysis, a bandwidth of ±0.8 Hz around each harmonic was excluded from the root mean square calculation.
Statistical analysis
The normality of the dependent variables was checked and subsequently confirmed using the Kolmogorov–Smirnov test. A three-way repeated-measures analysis of variance in frequency, protocol, and time was applied to analyze EMG and blood parameters. When a significant F-value was achieved, pair-wise comparisons were performed using the Bonferroni post hoc procedure. The reliability and variability of blood parameters were assessed with intraclass correlation coefficient and coefficients of variation (that is, CV=s.d.*100/mean). A paired t-test was used to analyze differences between both basal values. Statistical significance was set at P⩽0.05. Effect size statistic, η,2 was analyzed to determine the magnitude of the effect independent of sample size. Values are expressed as mean±s.d.
Results
Blood parameters
Table 2 shows the statistical significance and effect sizes of the analysis of variances. PBV increased after 1, 2 and 3 min of WBV (11.3±10.3%, P<0.05, 19.0±13.5% and 23.0±14.4%, P<0.01, respectively). At 1 and 2 min after the stop of the stimulus, PBV decreased at minute 3 of WBV (−14.4±9.3% and −14.0±8.5%, P<0.05, respectively) and was similar to baseline values. Regarding baseline values, the 10 Hz frequency did not modify PBV, whereas the 20 Hz frequency increased PBV after 2 and 3 min of WBV, and the 30 Hz frequency increased PBV after 1, 2 and 3 min of WBV as well as during the first minute after the end of the stimulus (Figure 3).
MBV increased after 1, 2 and 3 min of WBV (22.0±10.1%, 31.1±11.0% and 36.0±12.7%, P<0.001, respectively). Likewise, MBV remained increased in respect to baseline 1 min after the stop of the WBV (14.0±8.1%, P<0.05). The 30 Hz frequency increased MBV more than the 10 Hz frequency (26.8±8.1% in respect to 13.0±8.7%, P<0.001). However, no differences were observed between the increment with 20 Hz (17.0±11.3%) and the other two frequencies. All the frequencies increased the MBV in respect to baseline at minutes 1, 2 and 3 of WBV (Figure 4). Furthermore, 30 Hz increased MBV to a higher extent than 10 Hz and maintained the MBV increased in respect to baseline values 1 min after the end of the WBV. No protocol effect was observed for PBV or MBV.
Time course changes on mean blood velocity depending on the frequency during and after the application of 3 min of whole-body vibration and three cycles of 1 min of vibration and 1 min resting period. **, *** different from baseline at P<0.01 and 0.001, respectively. a, aaa, b different from 10 Hz at P<0.05, P<0.001 and P=0.08, respectively.
EMG
Regarding VM, EMGRMS was higher after 3 min of WBV in respect to baseline values (26.0±9.9 in respect to 18.9±2.8 mV, P<0.05). Likewise, for each frequency, EMGRMS was higher after 3 min of WBV in respect to baseline values, but no differences in baseline values nor after WBV were observed among frequencies. For both protocols, EMGRMS was higher after 3 min of WBV in respect to baseline values, no differences in baseline values were observed between protocols, but after WBV, EMGRMS was greater after the constant protocol (28.5±5.7 in respect to 23.5±3.3 mV, P<0.05).
Regarding the VL, EMGRMS was higher after 3 min of WBV in respect to baseline values (26.2±5.8 in respect to 15.2±1.1 mV, P<0.05). For each frequency, EMGRMS was higher after 3 min of WBV in respect to baseline values, but no differences in baseline values nor after WBV were observed among frequencies. Finally, for both protocols, EMGRMS was higher after 3 min of WBV in respect to baseline values, no differences in baseline values were observed between protocols, but after WBV, EMGRMS was greater after the constant protocol (29.7±7.5 in respect to 22.8±4.3 mV, P<0.05).
Discussion
The main findings of the present study were that WBV alone can significantly increase leg blood flow velocity and EMG activity in SCI patients. Moreover, higher frequencies (that is, 20 and 30 Hz) produced greater increase in leg blood flow velocity, although a tendency to evoke higher increase in blood flow velocity was observed with 30 Hz, which also maintained this variable above basal values after the stop of the stimulus. No difference was observed regarding the application of the WBV in a constant or fragmented protocol.
Leg blood flow velocity was increased during the application of WBV in SCI patients. However, the magnitude of blood flow response observed in our study is lower than in others carried out with healthy subjects.9, 11 Using an oscillating platform, Kerschan-Schindl9 found a two-fold increase in mean blood flow in the popliteal artery and Lythgo et al.11 found a four-fold increase in mean blood velocity in the femoral artery. These greater responses in comparison to our results could be due to the fact that: (1) the tilt table provides weight unloading, and as blood flow highly correlates with work output,12 a reduction in work output owing to unloaded weight may result in a smaller increase in blood flow;10 (2) greater the active tissue, higher the metabolic demand; as muscle weakness is a feature of SCI,2 the O2 demand should be reduced and subsequently would elicit a reduced response; and (3) the reduced femoral artery diameter and blood flow observed in SCI patients1 would limit the hemodynamic response to exercise.
WBV leads to an increased metabolic demand measured by oxygen uptake in a linear relationship with vibration frequency,13 which is in agreement with our results. As higher the frequency used, the greater increase in blood flow velocity was observed. Although there was no difference in this variable between 20 and 30 Hz, a trend to produce higher increase with 30 Hz was detected. Furthermore, 30 Hz maintained the PBV above basal values 1 min after the stop of the vibration. This would recommend using 30 Hz in order to analyze the long-term effects of the application of WBV in SCI patients.
To the best of our knowledge, this is the first study to apply WBV on a tilt table on SCI patients. Other ways of applying WBV on SCI patients have been through partial standing or standing on the platform with the help of a specific device.14 In the present study, the tilt table was fixed at an angle of 45° for the following reasons: (1) this angle unloads part of the weight of the subject but less than a sitting position; (2) SCI patients can experience episodes of orthostatic hypotension and can faint if angles near to the vertical are reached15 and (3) all the participants were familiarized with this angle as they used to maintain this position during 30 min in their rehabilitation routines.
The improvement of lower-extremity circulation is a goal of the rehabilitation of SCI patients.4 Some of the traditional exercises performed to achieve this goal have been passive leg movements and passive cycling; however, there is evidence supporting that these methods do not increase leg blood flow in SCI patients.16 As well as increasing blood flow, the application of WBV during supine bed rest for 52 days avoided a decrease of the diameter of the common femoral artery in respect to a control group.17 This observation has not been reported in SCI patients but future studies that combine WBV and Doppler ultrasound measures should contrast if this preservation is possible in this collective.
EMGRMS of VL and VM increased after the application of WBV independently of frequency or protocol. In healthy subjects, the same increases have been reported using frequencies between 15 and 30 Hz.18 In SCI patients, we have not found any research that combines WBV and EMG recordings, nevertheless the application of punctual vibration on thigh muscles during locomotion increased the muscle activity of SCI patients.19 This increase in the EMGRMS could be due to the fact that mechanical vibrations applied to the muscle or tendon stimulate sensory receptors and that activation of muscle spindles facilitates the activation of α-motoneurons, leading to tonic vibration reflex.20 In our study, no significant difference was noted depending on the frequency. It could be expected that 30 Hz would increase EMG amplitude more than 10 Hz, as the acceleration of the platform is higher as the frequency increases. Furthermore, in healthy subjects, greater EMG activity with high-frequency WBV training (40 and 45 Hz) has been reported when compared with lower frequencies (25 and 30 Hz).8 In our study, the lack of differences in the EMG activity between frequencies could be due to the reduced EMG response of SCI patients in respect to healthy subjects,21 as well as to the marked difference in the EMG patterns among SCI subjects;21 therefore, this lack of statistical significance could be due to a type II error.
In conclusion, WBV represents an option to induce a reflex muscle contraction in subjects with difficulties or inability to evoke voluntary contractions such as SCI patients. Our results show that WBV is an effective method to increase leg blood flow and to activate muscle mass in these patients, and could, therefore, be considered to be incorporated in rehabilitation programs of this collective. Moreover, the methodology proposed to apply SCI through the use of a tilt table has been safe, easy to perform and welcomed by the subjects and therapists.
References
Olive JL, Dudley GA, McCully KK . Vascular remodeling after spinal cord injury. Med Sci Sports Exerc 2003; 35: 901–907.
Giangregorio L, McCartney N . Bone loss and muscle atrophy in spinal cord injury: epidemiology, fracture prediction, and rehabilitation strategies. J Spinal Cord Med 2006; 29: 489–500.
Scelsi R . Skeletal muscle pathology after spinal cord injury: our 20 year experience and results on skeletal muscle changes in paraplegics, related to functional rehabilitation. Basic Appl Myol 2001; 11: 75–85.
Nash MS, Montalvo BM, Applegate B . Lower extremity blood flow and responses to occlusion ischemia differ in exercise-trained and sedentary tetraplegic persons. Arch Phys Med Rehabil 1996; 77: 1260–1265.
Kocina P . Body composition of spinal cord injured adults. Sports Med 1997; 23: 48–60.
Cruse JM, Lewis RE, Dilioglou S, Roe DL, Wallace WF, Chen RS . Review of immune function, healing of pressure ulcers, and nutritional status in patients with spinal cord injury. J Spinal Cord Med 2000; 23: 129–135.
Marin PJ, Rhea MR . Effects of vibration training on muscle strength: a meta-analysis. J Strength Cond Res 2010; 24: 548–556.
Hazell TJ, Jakobi JM, Kenno KA . The effects of whole-body vibration on upper- and lower-body EMG during static and dynamic contractions. Appl Physiol Nutr Metab 2007; 32: 1156–1163.
Kerschan-Schindl K, Grampp S, Henk C, Resch H, Preisinger E, Fialka-Moser V et al. Whole-body vibration exercise leads to alterations in muscle blood volume. Clin Physiol 2001; 21: 377–382.
Hazell TJ, Thomas GW, Deguire JR, Lemon PW . Vertical whole-body vibration does not increase cardiovascular stress to static semi-squat exercise. Eur J Appl Physiol 2008; 104: 903–908.
Lythgo N, Eser P, de Groot P, Galea M . Whole-body vibration dosage alters leg blood flow. Clin Physiol Funct Imaging 2009; 29: 53–59.
Saltin B, Radegran G, Koskolou MD, Roach RC . Skeletal muscle blood flow in humans and its regulation during exercise. Acta Physiol Scand 1998; 162: 421–436.
Rittweger J, Ehrig J, Just K, Mutschelknauss M, Kirsch KA, Felsenberg D . Oxygen uptake in whole-body vibration exercise: influence of vibration frequency, amplitude, and external load. Int J Sports Med 2002; 23: 428–432.
Davis R, Sanborn C, Nichols D, Bazett-Jones DM, Dugan EL . The effects of whole body vibration on bone mineral density for a person with a spinal cord injury: a case study. Adapt Phys Activ Q 2010; 27: 60–72.
Krassioukov A, Claydon VE . The clinical problems in cardiovascular control following spinal cord injury: an overview. Prog Brain Res 2006; 152: 223–229.
Ter Woerds W, De Groot PC, van Kuppevelt DH, Hopman MT . Passive leg movements and passive cycling do not alter arterial leg blood flow in subjects with spinal cord injury. Phys Ther 2006; 86: 636–645.
Bleeker MW, De Groot PC, Rongen GA, Rittweger J, Felsenberg D, Smits P et al. Vascular adaptation to deconditioning and the effect of an exercise countermeasure: results of the Berlin Bed Rest study. J Appl Physiol 2005; 99: 1293–1300.
Torvinen S, Kannu P, Sievanen H, Jarvinen TA, Pasanen M, Kontulainen S et al. Effect of a vibration exposure on muscular performance and body balance. Randomized cross-over study. Clin Physiol Funct Imaging 2002; 22: 145–152.
Cotey D, Hornby TG, Gordon KE, Schmit BD . Increases in muscle activity produced by vibration of the thigh muscles during locomotion in chronic human spinal cord injury. Exp Brain Res 2009; 196: 361–374.
De Cuyper H . The tonic vibration reflex]. Acta Belg Med Phys 1985; 8: 41–46.
Sherwood AM, McKay WB, Dimitrijevic MR . Motor control after spinal cord injury: assessment using surface EMG. Muscle Nerve 1996; 19: 966–979.
Acknowledgements
This work was supported in part by a grant from the IMSERSO (37/2008).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Herrero, A., Menéndez, H., Gil, L. et al. Effects of whole-body vibration on blood flow and neuromuscular activity in spinal cord injury. Spinal Cord 49, 554–559 (2011). https://doi.org/10.1038/sc.2010.151
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2010.151
Keywords
This article is cited by
-
The immediate effectiveness of whole-body vibration with the modified push-up position on neurocognitive parameters in overheads athletes with and without scapular dyskinesis
Sport Sciences for Health (2023)
-
Whole-body vibration modulates leg muscle reflex and blood perfusion among people with chronic stroke: a randomized controlled crossover trial
Scientific Reports (2020)
-
Palm vitamin E reduces locomotor dysfunction and morphological changes induced by spinal cord injury and protects against oxidative damage
Scientific Reports (2017)
-
Whole Body Vibration for People with Spinal Cord Injury: a review
Current Physical Medicine and Rehabilitation Reports (2017)
-
Chronic effects of simultaneous electromyostimulation and vibration on leg blood flow in spinal cord injury
Spinal Cord (2016)