Abstract
Study design:
Double-blind, placebo-controlled, flexible-dose study.
Objective:
To evaluate the efficacy, safety and tolerability of oral sildenafil in women with female sexual arousal disorder as a result of SCI (paraplegia/tetraplegia).
Setting:
The study was conducted at clinical practice sites in North America (n =23), 11 European countries (n =23), Australia (n =4) and South Africa (n =2).
Methods:
129 women were randomized and treated with sildenafil or matching placebo. A 4-week baseline period was followed by 12 weeks of treatment, which could be increased from 50 to 100 mg or decreased to 25 mg once during the treatment period, depending on efficacy and tolerability. By use of an event log, sexual activity was monitored between screening and the end of treatment. The Sexual Function Questionnaire, the Sexual Quality of Life Questionnaire–Female, a global efficacy question and Sexual Distress Question were also assessed.
Results:
Sildenafil-treated women and placebo-treated women had an increase in their percentage of sexual activities throughout the course of the study, with no statistically significant difference between groups in the percentage of successful sexual activities at end of treatment versus baseline. There were also no statistically significant differences between sildenafil- and placebo-treated women on the aforementioned measures. The most common adverse events included headache and vasodilatation.
Conclusion:
The results of this study are similar to other reports regarding a lack of clinically meaningful benefit of sildenafil in other populations of women.
Sponsorship:
This study was sponsored by Pfizer Inc.
Similar content being viewed by others
Introduction
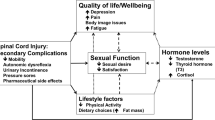
Sexual function is a major concern for persons with spinal cord injuries (SCIs, paraplegia/tetraplegia). Paraplegics have reported return of sexual function as their highest priority, followed by bowel and bladder concerns; tetraplegics have reported sexual function as second in importance after regaining hand function.1
The effects of SCIs on sexual function are well understood. On the basis of the level and degree of injury, predictable alterations in sexual response have been shown to occur in both women and men.2, 3 Laboratory analyses in women have been performed using vaginal pulse amplitude to show responses to audiovisual erotic and manual genital stimulation. Preservation of ability to perceive pinprick and light touch sensation in the T11 to L2 dermatomes has been shown to be predictive of psychogenic genital responses in women.4 In men, preservation of pinprick and light touch sensation in the T11 to L2 dermatomes predicts genital response to psychogenic stimulation.5 These findings suggest that psychogenic sexual arousal is mediated through innervation from the thoracolumbar sympathetic plexus. Studies of persons with SCIs have shown that these sympathetic fibers may be regulatory for genital sexual arousal.6 The ability to experience orgasm was diminished in women with SCIs; however, those with most levels and degrees of injury maintain the neurologic capability to achieve orgasm. The exception is those women with complete absence of reflexes affecting their sacral spinal segments. Similar findings were noted in men.7
Sildenafil citrate was the first approved selective phosphodiesterase type-5 inhibitor and has been successfully used to treat erectile dysfunction in men with SCIs.8, 9, 10 Because a laboratory-based pilot study determined that sildenafil use was associated with significantly improved subjective sexual and genital arousal in women with SCIs,11 a 12-week randomized controlled trial was conducted in women with female sexual arousal disorder (FSAD) as a result of SCI (paraplegia/tetraplegia).
Materials and methods
Study design
This multinational, parallel-group, double-blind, placebo-controlled, flexible-dose study was designed to evaluate the efficacy and safety of sildenafil in women with FSAD resulting from paraplegia/tetraplegia. It was conducted at clinical practice sites in North America (n =23), 11 European countries (n =23), Australia (n =4) and South Africa (n =2). Randomization was stratified by region (Europe/North America) defined a priori; South Africa and Australia were counted in Europe. The sponsor (Pfizer Inc) performed the statistical analyses and maintained the database and study integrity across sites. Investigators were responsible for adhering to the procedures of the study protocol, record-keeping and case report forms. Human subjects committee approval was obtained at all sites. All applicable institutional and governmental regulations concerning ethical use of human volunteers were followed.
Participants were identified through routine query during clinic assessment or previously indicated interest in research participation. At enrollment all women gave informed consent, viewed a video describing the effect of paraplegia/tetraplegia on sexual response and alternative ways to facilitate sexual arousal and orgasm, and completed screening tests, including validated study questionnaires, neurologic (International Neurologic Standards (ISNCSCI)) examination, Pap smear, serum testosterone level and detailed sexual function history.
This was followed by a 4-week, treatment-free, run-in period (baseline) after which eligible women were randomized to receive oral sildenafil 50 mg as needed, or a matching placebo, in a 12-week, double-blind treatment phase. Dose adjustments were allowed once, either increasing to 100 mg for greater efficacy or decreasing to 25 mg for greater tolerability. Assessments were conducted at screening (week −4); baseline (week 0); weeks 2, 4 and 8; and at the end of treatment (EOT; week 12). A follow-up visit occurred at week 16 as needed (Figure 1). Compliance was assessed by comparing participant event logs (completed every time study medication was taken) with returned supplies of study medication.
Eligibility criteria
Women (>18 years old) with a primary diagnosis of FSAD as a direct result of paraplegia/tetraplegia sustained at least 12 months before study entry were included. The FSAD may or may not have been associated with female orgasmic disorder (FOD), hypoactive sexual desire disorder (HSDD), or superficial introital dyspareunia.12 Women with primary anorgasmia or primary HSDD were excluded. Participants had to have means of direct genital stimulation (partner or vibrator); have reported personal distress as a result of their sexual life; be willing to attempt sexual activity at least weekly on average; and have an intact bulbocavernosal reflex and/or anal wink reflex.
Women were excluded who had a positive pregnancy test at screening; were less than 2 years postmenopausal and were unwilling to use acceptable contraceptive methods during the study; reported never having a satisfactory sex life or who had sexual dysfunction before paraplegia/tetraplegia; had sexual dysfunction considered to be situational; had received treatment for major psychiatric disorders in the past 12 months; were receiving treatment or psychotherapy for the sexual dysfunction; were using a clitoral vacuum device; had experienced clinically significant autonomic dysreflexia within the baseline period; were prescribed and/or took nitrates or nitric oxide donors; were taking a selective estrogen receptor modulator or had retinitis pigmentosa.
Assessment measures
Participants recorded information on study dosing, sexual activities and sexual satisfaction in an event log. Validated questionnaires included the Sexual Function Questionnaire (SFQ)13, 14 and the Sexual Quality of Life Questionnaire–Female Version (SQoL-F).15 The 34-item SFQ includes arousal-sensation, arousal-lubrication, arousal-cognitive, desire, enjoyment, orgasm, pain and partner domains. The 18-item SQoL-F assesses the effect of sexual dysfunction on confidence, emotional well-being and relationship. Participants also completed a Sexual Distress Question (SDQ): ‘Over the last four weeks, how much distress has your sexual life caused you?’ and a Global Efficacy Question (GEQ): ‘Did the study medication you received increase your sexual satisfaction?’ at week 12. Adverse events were recorded at each study visit.
Data analysis
The sample size was determined for the primary efficacy endpoint using simulation, assuming a Poisson distribution (with a mean of four events of sexual activity during the baseline period and during the last four treatment weeks). The assumed proportion of satisfactory sexual activities (SSAs) was 0.3 at baseline and 0.4 (placebo) and 0.6 (sildenafil) during the last four treatment weeks. A sample of 42 per treatment group was estimated to give at least 80% power to show a treatment difference at the two-sided 5% significance level; 65 per group were randomized to allow for 35% missing data.
All endpoints were analyzed for the intent-to-treat (ITT) population (all randomized participants who received at least one dose of study medication and had at least one post-baseline efficacy assessment). All analyses included baseline value (if collected for the endpoint) and two-level categorical variables representing treatment and region. In addition, the primary endpoint was analyzed for the subset of women with FOD and for the evaluable population (all study completers who had at least four events of sexual activity at which study medication was taken during the last four treatment weeks; did not violate any inclusion or exclusion criteria that could affect the efficacy outcome and were at least 80% compliant with study medication).
The primary efficacy endpoint was the change in the proportion of SSAs between baseline and the last four treatment weeks (EOT). For events to be included, study medication must have been taken before sexual activity. SSA was defined as one or more of the following: satisfactory intercourse, intercourse resulting in orgasm, oral sex resulting in orgasm, or partner-initiated or self-masturbation resulting in orgasm. For baseline and for EOT, the number of times that a participant took study medication, was sexually active and reported an SSA was tallied, and the proportion of SSAs was calculated using the total number of times of sexual activity as the denominator. This value was compared between treatment and placebo groups using Poisson regression with a (natural) log link function. To avoid zero values being calculated as undefined, +0.1 was added to all numerators. To extend the Poisson regression, incorporating time as an additional factor and appropriately accounting for within-participant correlation across time, an additional analysis was performed for each 4-week period (baseline, first 4 weeks, weeks 4–8 and last 4 weeks), which involved calculating summary statistics and fitting a general estimating equation model.
Secondary endpoints were on the basis of the ITT population and were the change in the number of SSAs between baseline and EOT, SSAs for the subgroup of women with FOD, SFQ domains and individual questions, SDQ, SQoL-F total score and GEQ. Each SFQ question and domain score, and the SQoL-F total score, were calculated for each participant at baseline and EOT. The observed mean (with standard error (s.e.)) and median were calculated by treatment group. Analysis of covariance was used to analyze scores. The least squares mean total score of the SQoL-F for each treatment group was derived and the difference, with 95% confidence interval, calculated.
For the SDQ, responses of ‘not distressed’ and ‘slightly distressed’ were coded as ‘0,’ whereas all other responses were coded as ‘1.’ The proportion of participants with an increased level of sexual satisfaction on the GEQ was also assessed. For both the SDQ and the GEQ, analysis was performed using a binary response logistic regression model. Parameter estimates and odds ratios with 95% confidence intervals were calculated.
Results
Of 185 women who were screened, 130 were assigned to treatment and 129 received treatment. Forty-one failed screening, 7 withdrew consent, 1 had an adverse event before study entry and 6 had other reasons for discontinuing participation.
Demographics and baseline characteristics
The mean age was 37 years (range, 19–62 years) and the mean weight was 65 kg (range, 43–166 kg); 86 (67%) of the women had FSAD and FOD (Table 1). The mean duration of was 9 years (median, 7 years; range, 1–35 years). The mean, median and range for total sensory scores were 133, 136 and 28 to 124, respectively. The same quantities, respectively, for total motor scores were 59, 50 and 0–100. On the ASIA impairment scale, 62 women (48%) were assessed as complete and 54 (42%) as incomplete, with the remainder having normal or missing assessments. Most participants did not experience autonomic dysreflexia (95 (73%)), and most had one or both sacral reflexes (bulbocavernosus/anal wink) intact (108 (83%)). The mean baseline serum testosterone level was 1.2 pg ml−1 (median 1.0 pg ml−1), with a range from 0 (undetectable levels) to 6.4 pg ml−1; the distribution of levels was negatively skewed, with most participants (113 (87%)) in the 0–2 pg ml−1 range.
Efficacy
The proportion of SSAs over time is shown in Figure 2. The difference from baseline to EOT was not statistically significant for the ITT population (adjusted ratio (95% ) for sildenafil versus placebo, 1.08 (0.91–1.28); P=0.4067), the evaluable population or FOD subgroup (Table 2).
Questionnaire data failed to achieve statistical significance between sildenafil and placebo. The raw mean at baseline was higher for women taking sildenafil versus placebo for nearly all SFQ domains; the differences in the least squares means at the EOT for SFQ domains were not significantly different between treatment groups (Table 3). The total score on the SQoL-F increased for both groups but the difference was not statistically significant (Table 4).
Results on the GEQ and SDQ favored sildenafil but were not statistically significant. More than half (55%) of the women receiving sildenafil, compared with 38% receiving placebo, reported improvement on the GEQ measure (Table 5). The number of women with decreased levels of distress was similarly higher for sildenafil as compared with placebo (Table 6).
Safety
More women taking sildenafil reported adverse events overall than did women taking placebo (76 versus 57%). The most common adverse events were headache and vasodilatation (Table 7). Fourteen women had severe adverse events of which five were categorized as treatment-related.
Eight sildenafil recipients and seven placebo recipients discontinued treatment, 3 and 2, respectively, because of adverse events. Laboratory abnormalities resulted in discontinuation by two women receiving placebo: an unintended pregnancy and increased SGPT. Two sildenafil recipients had serious adverse events unrelated to drug (skull fracture and idiopathic thrombocytopenic purpura). No relationships were noted between laboratory tests, vital signs and sildenafil.
Discussion
Improvements in sexual function were observed in both the sildenafil and the placebo groups during the first four treatment weeks, and tended to plateau during the remaining eight treatment weeks. Although sildenafil-treated women reported improvements on most measures of sexual function during the study, and a trend was observed on most study measures in favor of sildenafil, no significant differences were noted compared with placebo. This was true for the primary measure of SSAs and for secondary endpoints. Although not statistically significant, a 17% increase in the GEQ was observed with sildenafil as compared with placebo, and a similar trend was noted for the SDQ. The lack of statistical significance between sildenafil and placebo may be due to a high placebo response rate in the study. Indeed, the proportions of SSAs assumed when designing the study were 0.6 (sildenafil) and 0.4 (placebo), but the baseline-adjusted proportions were actually 0.59 and 0.55, respectively, indicating a higher than assumed placebo response. Thus, the treatment effect is small and a sample of 130 has very low power (<10%) to declare such a difference as statistically significant. The role of the partner and non-pharmacologic beneficial effects of study participation may have also contributed to the lack of significant treatment effect.
Several limitations may have influenced the study results. It is likely there were differential physiologic effects with varying patterns of paraplegia/tetraplegia, in addition to various psychosocial issues affecting the women. Participants may have interpreted ‘satisfactory sexual activity’ differently. Relatively infrequent sexual activity after paraplegia/tetraplegia may have required a longer testing phase. Use of event logs to monitor compliance could have been compromised by backfilling, although this should have been controlled by the counts of returned medication.
Although sildenafil has been shown to be highly effective as a treatment for erectile dysfunction in men with SCIs, with obvious benefit from a biofeedback loop with visible erections, this is not so clear for women. Despite the beneficial results shown in a laboratory study,11 the results in this randomized clinical trial were less convincing.
Future studies may include more specific eligibility criteria, such as only including women for whom FSAD is the primary diagnosis and excluding those with HSDD16 or with sexual disorders that are categorized in the Diagnostic and Statistical Manual of Mental Disorders (4th edn, Text Revision) under the subtypes due to psychological or situational factors.12
Although free testosterone levels were not correlated with SSA frequency, this may be a function of the androgens measured or the assay selected. There is a lack of normative data and literature showing the role of androgens in female sexuality or sexual disorders.
Studies of sildenafil in able-bodied women with FSAD have also shown inconsistent results. In one study,16 efficacy was shown on only one sexual function measure and only in a small subsample of women who had no associated HSDD and had sufficient estradiol and free testosterone concentration or were receiving estrogen and/or androgen replacement therapy. Proposed reasons for the unconvincing efficacy of sildenafil in women have included failure to adequately characterize the study populations, differences in the physiologic response to sildenafil in men and women, and the mechanism of action of the drug needing to be central and not peripheral. It is also possible that lack of concordance between physiological and subjective aspects of women's sexual experiences need to be further investigated.17 These issues should be addressed when designing future studies of women with FSAD due to paraplegia/tetraplegia.
References
Anderson KD . Targeting recovery: priorities of the spinal cord-injured population. J Neurotrauma 2004; 21: 1371–1383.
Sipski ML, Alexander CJ . Sexual activities, response and satisfaction in women pre- and post-spinal cord injury. Arch Phys Med Rehab 1993; 74: 1025–1029.
Alexander CJ, Sipski ML, Findley TW . Sexual activities, desire, and satisfaction in males pre- and post-spinal cord injury. Arch Sex Behav 1993; 22: 217–228.
Sipski ML, Alexander CJ, Rosen R . Sexual arousal and orgasm in women: effects of spinal cord injury. Ann Neurol 2001; 49: 35–44.
Sipski M, Alexander C, Gomez-Marin O, Spalding J . The effects of spinal cord injury on psychogenic sexual arousal in males. J Urol 2007; 177: 247–251.
Sipski ML, Rosen RC, Alexander CJ, Gomez-Marin O . Sexual responsiveness in women with spinal cord injuries: differential effects of anxiety-eliciting stimulation. Arch Sex Behav 2004; 33: 295–302.
Sipski M, Alexander CJ, Gomez-Marin O . Effects of level and degree of spinal cord injury on male orgasm. Spinal Cord 2006; 44: 798–804.
Giuliano F, Hultling C, El Masry WS, Smith MD, Osterloh IH, Orr M et al. Randomized trial of sildenafil for the treatment of erectile dysfunction in spinal cord injury. Ann Neurol 1999; 46: 15–21.
Maytom MC, Derry FA, Dinsmore WW, Glass CA, Smith MD, Orr M et al. A two-part pilot study of sildenafil (VIAGRA) in men with erectile dysfunction caused by spinal cord injury. Spinal Cord 1999; 37: 110–116.
Hultling C, Giuliano F, Quirk F, Peña B, Mishra A, Smith MD . Quality of life in patients with spinal cord injury receiving Viagra (sildenafil citrate) for the treatment of erectile dysfunction. Spinal Cord 2000; 38: 363–370.
Sipski ML, Rosen RC, Alexander CJ, Hamer RM . Sildenafil effects on sexual and cardiovascular responses in women with spinal cord injury. Urology 2000; 55: 812–815.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders DSM-IV-TR 4th edn (Text Revision). American Psychiatric Association: Washington DC, 2000.
Quirk FH, Heiman JR, Rosen RC, Laan E, Smith MD, Boolell M . Development of a sexual function questionnaire for clinical trials of female sexual dysfunction. J Womens Health Gend Based Med 2002; 11: 277–289.
Quirk F, Haughie S, Symonds T . The use of the sexual function questionnaire as a screening tool for women with sexual dysfunction. J Sex Med 2005; 2: 469–477.
Symonds T, Boolell M, Quirk F . Development of a questionnaire on sexual quality of life in women. J Sex Marital Ther 2005; 31: 385–397.
Berman JR, Berman LA, Toler SM, Gill J, Haughie S . Safety and efficacy of sildenafil citrate for the treatment of female sexual arousal disorder: a double-blind, placebo controlled study. J Urol 2003; 170: 2333–2338.
Chivers ML, Rosen RC . Phosphodiesterase type 5 inhibitors and female sexual response: faulty protocols or paradigms? J Sex Med 2010; 7: 858–872.
Acknowledgements
This study was sponsored by Pfizer Inc. Editorial support was provided by Anne Johnson, Janet E Matsuura, PhD, and Deborah M Campoli-Richards, BSPharm, RPh, of Complete Healthcare Communications, Inc., and was funded by Pfizer Inc.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Marca Sipski Alexander reports no commercial interests with the study sponsor. Raymond Rosen reports no current commercial interests with the study sponsor. At the time of this research, Dr Rosen served as a consultant and research advisor for Pfizer Inc. Claes Hultling reports no commercial interests with the study sponsor. Tara Symonds and Scott Haughie are employees of Pfizer. Susanne Steinberg was an employee of Pfizer when the study was conducted.
Rights and permissions
About this article
Cite this article
Alexander, M., Rosen, R., Steinberg, S. et al. Sildenafil in women with sexual arousal disorder following spinal cord injury. Spinal Cord 49, 273–279 (2011). https://doi.org/10.1038/sc.2010.107
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2010.107
Keywords
This article is cited by
-
A Scoping Review of Literature on Sexual Health and Wellness in Women with Spinal Cord Injury
Sexuality and Disability (2024)
-
Sexual Health in the Neurogenic Patient
Current Bladder Dysfunction Reports (2020)
-
Sexual Dysfunction After Spinal Cord Injury
Current Sexual Health Reports (2020)
-
Knowledge Gaps in Urologic Care of Female Spinal Cord Injury Patients
Current Urology Reports (2019)
-
Sexual Function after Spinal Cord Injury: Innervation, Assessment, and Treatment
Current Sexual Health Reports (2016)