Abstract
Study design:
Cohort study.
Objectives:
To provide recent estimates of the incidence of traumatic spinal cord injury (SCI) in adults living in Ontario.
Setting:
Ontario, Canada.
Methods:
The study included all men and women aged 18 years and older living in Ontario. The two primary data sources used for this study were the census data provided by Statistics Canada and the hospital Discharge Abstract Database (DAD) provided by the Canadian Institute for Health Information. Incidence was estimated for the fiscal years 2003/04–2006/07, and examined by age, gender, mechanism and seasonality of injury, the level of injury, the presence of comorbidity and in-hospital mortality.
Results:
The incident cases had a mean age of 51.3 years (s.d. 20.1). The majority of the cases was male (74.1%) and had a cervical SCI caused by falls (49.5%). The age-adjusted incidence rate was stable over the 4-year study period, from 24.2 per million (95% CI: 21.2–27.6) in 2003 to 23.1 per million (95% CI: 20.2–26.3) in 2006.
Conclusion:
Despite worldwide trends that have indicated motor vehicle collisions (MVCs) as the leading cause of injury, falls emerged as the leading cause of traumatic SCI in this study. This finding, and the fact that the number of fall-induced injuries increased steadily with age, may indicate that there is growing concern for the consequences of falls in the elderly. Further work is needed to understand this trend in age and gender and the causes of falls to develop effective fall prevention strategies.
Similar content being viewed by others
Introduction
Although only one in 40 patients admitted to a major trauma center suffers an acute spinal cord injury (SCI),1 these injuries have a devastating impact on quality of life as they contribute to a high level of long-term disability,1 morbidity,2, 3, 4, 5 mortality1, 6, 7 and impose an economic burden to communities1, 8, 9, 10 and the patient.11, 12 Like most forms of trauma, the incidence of injuries may be minimized given sufficient information about patterns of occurrence and underlying causes.
Published incidence rates of SCI vary according to the definition of injury used and the availability of the data sources. In North America, the incidence of SCI has been described as stable over the past 30 years, and ranges from 27 to 47 cases per million.13 In the nineties, the worldwide incidence rates per million per year were reported to vary from 10.4 to 29.7 in Europe, from 27.1 to 83.0 in North America, from 18 to 40.2 in Asia and ∼14.5 per million per year in Australia during the same period.14
In North America, SCI was described as more commonly experienced by young men as a result of a motor vehicle collision (MVC).13 Some studies highlighted an increase in the mean age at injury over time,6, 15 with the highest increase in incidence rate in elderly people aged 65 years and older.1 This shift in the age pattern seems to be correlated with a shift in the etiology, characterized as an increase in fall-induced injuries.16 Falls have been reported as the leading cause of injury in the province of Ontario, Canada.6 Some studies have also highlighted an increase in the proportion of women with SCI16 and an increase in the percentage of cervical injuries.16
The most recent study on a Canadian population was based on a retrospective analysis of medical records from London, Ontario between 1997 and 2001.6 This study reported incidence rates for the population hospitalized in one trauma center. Assuming that the population that might be hospitalized in this center lives in the London catchment, the rates estimated in this study could only be extrapolated to this population, which roughly represents 3% of the Ontario population and 1% of the Canadian population. This study confirmed that a large proportion of injuries were seen among older adults, predominantly as a result of falls.
Our goal was to provide recent estimates of the incidence of traumatic SCI in men and women aged 18 years or older living in Ontario. Incidence was estimated for the period 2003–2006 and examined by age, gender, mechanism and seasonality of injury, the level of injury, the presence of comorbidity and in-hospital mortality. This is the first study in a three-part investigation of SCI incidence, health-care utilization and rehospitalization in Ontario, Canada.
Materials and methods
Study population
The study included all men and women aged 18 years or older living in Ontario during the fiscal years 2003–2004 (1 April 2003–31 March 2004) through 2006–2007 (1 April 2006–31 March 2007). The province of Ontario has a population of over 11 million residents and represents 40% of the total population of Canada. Ontario residents have universal access to a publicly funded health-care system (that is, no private institutions), making hospital data a valid tool for studying the population.
Data source
The two primary data sources were the census data provided by Statistics Canada and the hospital Discharge Abstract Database (DAD) provided by the Canadian Institute for Health Information. Statistics Canada provides annual population figures on 1 January by 1-year age groups of men and women living in Ontario. Collection of the DAD is mandatory for resource allocation. It includes standard inpatient discharge abstracts containing compulsory information on the patient (that is, gender, age, external causes of injury, admission and discharge date), the diagnoses (using ICD-10 codes) and the care received for each patient stay in an acute care hospital. The most responsible diagnosis is the most significant contributor to the length of stay during hospitalization. The data quality of the DAD is routinely evaluated (http://secure.cihi.ca/cihiweb/dispPage.jsp?cw_page=quality_e.).
Identification of SCI
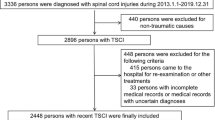
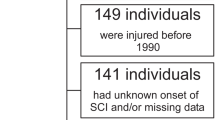
In Ontario, the records of all patients with at least one hospital stay with a most responsible diagnosis code of traumatic SCI (see ICD-10 in Appendix A) and a valid health-card number during the study period were selected. This includes Ontario residents hospitalized in the province regardless of where the injury took place. The inclusion and exclusion criteria are detailed in Figure 1.
Statistical analysis
The number and percentage of incident SCI cases were described by age at admission, gender, external causes of injury, level of injury (cervical, thoracic, lumbar or other), Charlson index (co-morbidity), seasonality of the injury (month of admission) and discharge disposition after the index admission. The causes of injury were stratified based on the International Collaborative Effort on Injury Statistics17 into the following categories: traffic collision, fall, struck by/against object (that is, pedal cyclist injured in collision with pedestrian and so on) or other (that is, firearm, machinery and so on). The causes and level of injury were also analyzed by age group. Mean and standard deviation were estimated for age at admission and length of stay at the index admission. Non-parametric statistical tests were used to evaluate age effects.
Standardized incidence rates using the age structure of the Ontario population (census data) and age-specific incidence rates were estimated by gender and by year, and over the four cumulated fiscal years (that is, 2003/04–2006/07).
Results
Patients with an incident SCI
The incident cases had a mean age of 51.3 (s.d. 20.1) years. The majority of the cases was male (74.1%) and had a cervical SCI caused by falls (49.5%) with a slight increase in the number of injuries (32.1%) between July and September (Table 1). The mean length of acute stay was 22.7 days (s.d. 32.8), and most of the patients were directly discharged to rehabilitation hospitals (50.2%). Results were similar across the 4-year study period.
Incidence
The age-adjusted incidence rate was rather stable over the 4-year study period, from 24.2 per million (95% CI: 21.2–27.6) in 2003 to 23.1 per million (95% CI: 20.2–26.3) in 2006. These results were observed for both men and women (Figure 2). The average age-standardized annual rate over the 4-year period was 24 per million (95% CI: 22.5–25.6). This rate was 36.3 per million (95% CI: 33.7–39.1) for men and 12.1 per million (95% CI: 10.6–13.7) for women. Figure 3 shows that age-specific incidence increases, more markedly for the age group 40–49 years in men and 50–59 years in women. For men, the incidence for the 80+ age group was three times higher than the incidence for the 40–49 age group. For women, the incidence for the 80+ age group was more than four times higher than the incidence for the 50–59 age group. Regarding the level of injury (Figure 4), the number of cervical cases increased with age (26.1% for age group 19–39 years to 42.6% for age group 60+ years), whereas the number of the other level of injuries tended to decrease with age (P<0.001).
Cause of injury
Falls were the leading cause of injury in men (47.8%) and women (54.1%) followed by MVCs in both men (23.0%) and women (28.5%). Men were more likely than women to be struck by or against an object (12.9 vs 5.4%) or in other circumstances (15.1 vs 8.7%) (P<0.001). Figure 5 shows that the number of fall-induced injuries steadily increased with age (19% for age group 18–39 years and 51.8% for age group 60+ years), whereas the three other causes decreased with age (P<0.001).
In-hospital mortality
Of the 109 (11.6%) patients who died during the index admission, 92 (84%) were aged 60 or older, 79 (72.5%) were men, 77 (70.6%) were injured after a fall, 91 (83.5%) had a cervical SCI and 55 (50.5%) scored 0 on the Charlson co-morbidity index.
Discussion
This study reported a stable incidence rate of SCI over 4 years between 2003 and 2006. Given that the pre-hospital deaths were not included, the incidence rate might be underestimated as ∼15.8% of cases die before hospitalization.9 The current population was predominantly composed of men who had sustained a cervical SCI induced by a fall. An increase in incidence with age was observed from age 40 to 49 years in men and from age 50 to 59 years in women. This increase with age was higher in women. In parallel, an increase with age in the number of cervical cases and in the number of falls was observed.
Incident rates of SCI estimated for Ontario fall within the range of other published estimates worldwide, which vary from 10.4 per million in The Netherlands to 83 per million in Alaska.14 Our estimates are slightly different from two earlier published studies on the Ontario population.6, 18 The most recent study reported incident rates between 20 and 50 per million for the period 1997–2000.6 It may be difficult to compare results because of a referral bias, as Pickett based his incidence rates on cases from one hospital in Ontario. The second study reported rates of hospitalizations from 37.2 to 46.2 per million for the period 1994–1998.18 Discrepancies between the rates published in these studies and the rates reported in our study can be explained by at least two methodological differences. First, the other study had no exclusion based on age (that is, included pediatric cases), whereas our study only included those individuals 18 years of age or older. Second, although one of the same data sources (DAD) was used to identify the SCI cases, it did not exclusively select incident cases and likely captured re-admissions within the incident rates. In addition, they included records that had an emergency department visit but no hospitalization. These cases most likely represent patients with a suspected, but not confirmed SCI.
The mean age at onset of SCI was particularly high in our study compared with the mean ages published earlier.1, 13, 14, 15 Part of the difference with published results may reside in our selection of a population aged 18 years or older. In contrast, compared with a US population, violence as a cause of SCI is rare in the Canadian population (roughly 10 vs 3%, respectively).13 As SCI caused by acts of violence usually occurs among a younger age group, this might explain part of our higher mean age at onset. Finally, the difference might also be explained by the increased number of elderly people in our society. Currently, ∼13% of the Ontario population is aged 65 years or older. Our results confirm the trend in the increased age at onset of SCI.13, 15, 16
The increase with age in the number of falls and cervical injuries associated with an increase in incidence observed in our study is consistent with several studies.1, 6, 15, 16 A Finnish study highlighted a 131% increase in the incidence of fall-induced cervical injury among Finns aged 50 years or older between the years 1970 and 2004 and incidence was higher in men. The authors hypothesized that even if women fall more often than men, their fall-induced injury is probably milder. The authors highlighted that this increase in the incidence of fall-induced injury cannot be explained merely by demographic changes. They hypothesized that impaired muscle strength, balance and reaction time related to poorer physical condition, less active lifestyle, poorer nutritional status (vitamin D and calcium) or increased consumption of cigarettes and alcohol might partly explain the phenomenon. They also hypothesized that less healthy and functionally less capable elderly people are now surviving to older ages because of more effective health care.19
Our study highlights, falls as the leading cause of injury before vehicle traffic collisions, which induced 24.5% of SCI. Unintentional falls (43.2%) followed by unintentional transport incidents (42.8%) were already reported as the leading causes of injury in the Ontario population with no age selection in 1994–1999.18 MVCs have remained the leading cause of SCI worldwide in the last decades even as falls have been increasing over time and becoming the second leading cause. Our results could partly be related to our selection of an adult population and to demographic changes as SCI because of MVCs are more frequent in younger populations. In contrast, changes in seat belt legislation and motor vehicle licensing regulations may also explain the decrease in MVC etiology.
Our study contains some limitations. First, the sensitivity and specificity of our identification of traumatic SCI incident cases have not been evaluated. The incident cases that might have been missed by our selection are of (1) patients who die at the scene of injury, which could underestimate our incident rate by as much as 15%; and of, (2) trauma patients for whom the SCI diagnosis is delayed or missed. The SCI diagnosis can be made easily in the awake, alert and clinically not intoxicated trauma patient. Thus, the SCI diagnosis may be delayed for patients with multiple traumas because of emergency procedures (that is, patients requiring prolonged mechanical ventilation). A delayed diagnosis can also occur for the rare patients with non-skeletal cervical spine injury (that is, patients with subluxation or cord injury without associated vertebral fractures), as neurological deficits may appear later. In both situations, the SCI diagnosis could be recorded in a second (or more) hospital stay after injury and would be captured by our selection procedure. For multiple trauma, the SCI could also be missed if it was not considered as the most responsible diagnosis, but this situation is likely rare. Our selection may also have identified false incident cases. This was minimized by excluding patients who had had a SCI diagnosis within 1 year before the index event. Some false positives and false negatives can be related to data quality (that is, SCI ICD-10 code not recorded in the presence of a SCI or SCI ICD-10 code over-coded in the absence of SCI). These situations were considered marginal.
Second, administrative data provide limited clinical information and do not permit description of the severity of injury. Third, our study suffers a lack of power because of the small number of incident cases. Further analyses are necessary to understand age and gender effect in our results.
Studies that provide information on the epidemiology of traumatic SCI in Canadian populations are scarce. The current study presents recent data and highlights that SCI because of MVCs are decreasing, whereas fall-induced cervical SCI are increasing. These findings need to be confirmed in other Canadian provinces and in other countries. In addition, further analyses are necessary to understand this trend regarding age and gender. Further, research related to the mechanisms of falls is needed to develop and promote effective fall-prevention programs.
References
Sekhon LH, Fehlings MG . Epidemiology, demographics, and pathophysiology of acute spinal cord injury. Spine 2001; 26 (24 Suppl): S2–S12.
McKinley WO, Jackson AB, Cardenas DD, DeVivo MJ . Long-term medical complications after traumatic spinal cord injury: a regional model systems analysis. Arch Phys Med Rehabil 1999; 80: 1402–1410.
Berlly M, Shem K . Respiratory management during the first five days after spinal cord injury. J Spinal Cord Med 2007; 30: 309–318.
Smith BM, Evans CT, Kurichi JE, Weaver FM, Patel N, Burns SP . Acute respiratory tract infection visits of veterans with spinal cord injuries and disorders: rates, trends, and risk factors. J Spinal Cord Med 2007; 30: 355–361.
Siddall PJ, McClelland JM, Rutkowski SB, Cousins MJ . A longitudinal study of the prevalence and characteristics of pain in the first 5 years following spinal cord injury. Pain 2003; 103: 249–257.
Pickett GE, Campos-Benitez M, Keller JL, Duggal N . Epidemiology of traumatic spinal cord injury in Canada. Spine 2006; 31: 799–805.
Garshick E, Kelley A, Cohen SA, Garrison A, Tun CG, Gagnon D et al. A prospective assessment of mortality in chronic spinal cord injury. Spinal Cord 2005; 43: 408–416.
DeVivo MJ . Causes and costs of spinal cord injury in the United States. Spinal Cord 1997; 35: 809–813.
Dryden DM, Saunders LD, Jacobs P, Schopflocher DP, Rowe BH, May LA et al. Direct health care costs after traumatic spinal cord injury. J Trauma 2005; 59: 443–449.
French DD, Campbell RR, Sabharwal S, Nelson AL, Palacios PA, Gavin-Dreschnack D . Health care costs for patients with chronic spinal cord injury in the Veterans Health Administration. J Spinal Cord Med 2007; 30: 477–481.
Woolhandler S, Himmelstein DU . Double catastrophe: injury-related bankruptcies. Med Care 2007; 45: 699–701.
Hollingworth W, Relyea-Chew A, Comstock BA, Overstreet JK, Jarvik JG . The risk of bankruptcy before and after brain or spinal cord injury: a glimpse of the iceberg's tip. Med Care 2007; 45: 702–711.
Fisher CG, Noonan VK, Dvorak MF . Changing face of spine trauma care in North America. Spine 2006; 31 (11 Suppl): S2–S8; discussion S36.
Wyndaele M, Wyndaele JJ . Incidence, prevalence and epidemiology of spinal cord injury: what learns a worldwide literature survey? Spinal Cord 2006; 44: 523–529.
Ho CH, Wuermser LA, Priebe MM, Chiodo AE, Scelza WM, Kirshblum SC . Spinal cord injury medicine. 1. Epidemiology and classification. Arch Phys Med Rehabil 2007; 88 (3 Suppl 1): S49–S54.
Jackson AB, Dijkers M, Devivo MJ, Poczatek RB . A demographic profile of new traumatic spinal cord injuries: change and stability over 30 years. Arch Phys Med Rehabil 2004; 85: 1740–1748.
National Center for Health Statistics. Injury ICE Activities. Available at: http://www.cdc.gov/nchs/about/otheract/ice/matrix10sas.htm. Accessed June 10, 2008.
Pickett W, Simpson K, Walker J, Brison RJ . Incidence of traumatic spinal cord injury in Ontario, Canada. J Trauma 2003; 55: 1070–1076.
Kannus P, Parkkari J, Koskinen S, Niemi S, Palvanen M, Järvinen M et al. Fall-induced injuries and deaths among older adults. JAMA 1999; 281: 1895–1899.
Acknowledgements
This research was supported by a grant from the Ontario Neurotrauma Foundation (ONF). Dr Jaglal is the Toronto Rehabilitation Institute Chair at the University of Toronto in Health Services Research. Dr Couris postdoctoral fellowship was supported by the Toronto Rehabilitation Institute and the University of Toronto. We acknowledge the support of Toronto Rehabilitation Institute that receives funding under the Provincial Rehabilitation Research Program from the Ministry of Health and Long-Term Care in Ontario. The views expressed do not necessarily reflect those of the Ministry.
Author information
Authors and Affiliations
Corresponding author
Appendix A
Appendix A
Traumatic SCI ICD-10-CA codes (obtained from Rick Hansen Foundation), stratified by level of injury
Note: All these ICD10 diagnosis codes have been checked for evolution.
Rights and permissions
About this article
Cite this article
Couris, C., Guilcher, S., Munce, S. et al. Characteristics of adults with incident traumatic spinal cord injury in Ontario, Canada. Spinal Cord 48, 39–44 (2010). https://doi.org/10.1038/sc.2009.77
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2009.77
Keywords
This article is cited by
-
Quality of in-hospital care in traumatic spinal column and cord injuries (TSC/SCI) in I.R Iran
European Spine Journal (2024)
-
Epidemiological features of traumatic spinal cord injury in Wuhan, China
Journal of Orthopaedic Surgery and Research (2023)
-
Current state of fall prevention and management policies and procedures in Canadian spinal cord injury rehabilitation
BMC Health Services Research (2020)
-
Reactive stepping after a forward fall in people living with incomplete spinal cord injury or disease
Spinal Cord (2020)
-
International Standards for Neurological Classification of Spinal Cord Injury: factors influencing the frequency, completion and accuracy of documentation of neurology for patients with traumatic spinal cord injuries
European Journal of Orthopaedic Surgery & Traumatology (2019)