Abstract
Study design:
An observational study.
Objective:
We report clinical, MRI and urodynamic findings in spinal tuberculosis.
Setting:
Tertiary care teaching hospital.
Method:
Patients with spinal tuberculosis having micturition disturbances or high postvoidal residual (PVR) urine were subjected to clinical evaluation, urodynamic and spinal MRI. Urinary symptoms were scored as per the American Urological Association Symptom (AUAS) Index. The outcome was defined at 12 months into complete, partial and poor.
Results:
Of 30 spinal tuberculosis patients, 15 had micturition disturbance and included urinary retention in 4, stress incontinence in 2, hesitancy in 6, urgency in 11 and urge incontinence in 9 patients. Thirteen patients had paraparesis and one had quadriparesis. Spinal MRI revealed granuloma in 2, dorsal vertebral involvement in 12 and cervical and lumbar vertebral involvement in 1 patient each. On urodynamic study, detrusor hyperreflexia (DH) with high-pressure voiding was present in six, detrusor areflexia (DA) in four, normal study in one and increased PVR urine in the remaining patients. AUAS score improved on follow-up. DA changed to DH with high-pressure voiding in one patient. The 15 patients without micturition disturbance had no horizontal sensory level, milder or no weakness and only 2 had spinal cord signal changes. Patients with micturition disturbances had poorer functional recovery at 1 year compared to those without micturition disturbances.
Conclusion:
Bladder symptoms were present in 50% of the admitted patients with spinal tuberculosis and related to severity of paraplegia, horizontal sensory level, cord signal abnormality and poorer outcome compared to those without spinal tuberculosis. Urodynamic study helped in categorization and management.
Similar content being viewed by others
Introduction
Spinal tuberculosis is common in the developing countries and constitutes 1% of all tuberculosis.1 Most of the studies on spinal tuberculosis have focused on motor and sensory deficits and bladder involvement has not received much attention. A Medline search with key words ‘spinal tuberculosis’, ‘bladder dysfunction’ and ‘Pott's paraplegia’ revealed only one case report evaluating urinary symptoms that too without urodynamic study.2
We report urodynamic findings in spinal tuberculosis for the first time and correlate these with clinical and MRI findings. The clinical and MRI findings of these patients were also compared with those without micturition disturbance.
Subjects and methods
Subjects
Patients with spinal tuberculosis with micturition symptoms or increased postvoidal residual (PVR) urine were subjected to urodynamic studies. The clinical and MRI findings of these patients were compared with those without micturition disturbances. The diagnosis of spinal tuberculosis was based on clinical findings, MRI and ultrasound or CT-guided biopsy. A detailed clinical history and the presence of spinal deformity and paravertebral swelling were recorded. Muscle power was graded on Medical Research Council scale, and muscle tone and deep tendon reflexes were categorized into increased, reduced or normal. Sensations of pinprick and joint position were recorded. Disability was assessed by paraplegia score,3 Barthel index score4 and Walking Index for Spinal Cord Injury at admission, 6 and 12 months.
Assessment of micturition disturbances
Clinical
The patients were asked about storage (frequency, urgency and urge incontinence) and voiding (hesitancy, intermittency, poor stream, terminal dribbling, incomplete emptying) problems. Bladder symptoms were scored using the American Urological Association Symptom (AUAS) score.5 The patients were also asked about impotence, erection, ejaculation, constipation and stress incontinence.
Urodynamic studies
Urodynamic studies were carried out using Dantec UD 5500 equipment (Dantec Inc., Copenhagen, Denmark) employing a standard technique.6 On the basis of urodynamic studies, the bladder dysfunction was classified into detrusor areflexia (DA), detrusor hyporeflexia and detrusor hyperreflexia (DH) with or without high-pressure voiding.6 Patients with DA and detrusor hyporeflexia were grouped together in the subsequent analyses because of the small sample size and similar management.
Patients with DA or hyporeflexia were managed with clean intermittent catheterization and DH by anticholinergics. DH with high-pressure voiding was managed with clean intermittent catheterization and anticholinergics.
Investigations
Complete hemogram, serum chemistry, HIV serology and chest roentgenogram were carried out. Spinal MRI was carried out using a 1.5 T scanner (Signa; GE Medical system, WI, USA) and T1, T2, and T1 contrast images were obtained in the sagittal and axial planes. The signal changes in vertebrae, disk space and paravertebral tissue were noted. Any cord compression, thecal compression and signal alteration in the spinal cord were also noted.
Treatment and follow-up
Patients were treated conservatively with 3-month bed rest and four-drug antitubercular treatment; Rifampicin 10 mg kg−1, isoniazide 5 mg kg−1, ethambutol 15 mg kg−1 and pyrazinamide 25 mg kg−1. They were followed up at 3, 6 and 12 months and their clinical and micturition improvement was noted. Urodynamic study was carried out in selected patients. The outcome was defined at 12 months into poor, partial and complete recovery.7 The type of bladder dysfunction on urodynamic studies was correlated with clinical and MRI findings using χ2-test or Fisher's exact test and improvement in AUAS and Walking Index for Spinal Cord Injury score by paired t-test. The clinical and MRI findings in the patients with and without micturition disturbances were compared by χ2-test, Fisher's exact test and independent t-test using SPSS version 13 software.
Results
Thirty patients with spinal tuberculosis were admitted during the study period and 15 (50%) had micturition disturbances.
Clinical and MRI findings of the patients with bladder dysfunction
Clinical
The mean age of the patients with spinal tuberculosis was 39.4 (range 22–60) years and 7 were women. The mean duration of illness was 11 (1–33) months. Fever was present in 7, pain and paresthesia in 14 and walking difficulty in 14 patients. Seven patients were bedridden, one wheelchair bound and six partially dependent. Two patients had history of pulmonary tuberculosis and two had active pulmonary tuberculosis. Spinal deformity was present in six patients. Thirteen patients had paraparesis and one had quadriparesis; the limb weakness was severe (grade 0–I) in four, moderate (grade II–III) in three and mild (grade IV) in seven patients; three of these patients had associated wasting of lower limbs. Tone was increased in 13 patients. Horizontal sensory loss was present in 12 patients, which was in dorsal region in all except in 1 who had C5 level. Lower limb joint position and vibration sensations were impaired in 12 patients.
Urinary symptoms
Thirteen patients had symptoms related to storage, nine to voiding and nine to both storage and voiding dysfunction. Two patients did not have any bladder symptoms but had increased PVR urine (Table 1). Impotence was reported by 3 and constipation by 10 patients. The severity of urinary symptoms on AUAS score ranged between 0 and 35 (16.07±12.86).
Spinal MRI revealed vertebral involvement in 14 and only intraspinal granuloma (D6) in 1 patient. Two adjacent vertebrae were involved in nine, 3–4 vertebrae in three and more than 4 in two patients. Dorsal vertebrae were involved in 11 patients and 1 each had cervical and lumbar involvement. Intervertebral disk space was reduced in 12 patients. Spinous processes were also involved along with body in seven patients. Soft tissue swelling was present in 11 that contributed to cord compression. Spinal cord signal changes were present in 12 patients, of whom 2 had intraspinal granuloma. One patient had enhancement of spinal meninges suggestive of arachnoiditis.
Comparison of clinical and MRI findings with and without bladder dysfunction
None of the 15 patients without micturition disturbance had fever or horizontal sensory level. Eight patients had normal muscle power. On MRI, none had spinous process involvement and only two had spinal cord signal changes. The severity of paraplegia (P=0.02), sensory level (P=0.0001) and spinal cord signal changes on MRI (P=0.001) were significantly related to micturition disturbances. All the patients without micturition abnormality improved at 1 year except one who had partial recovery. The details are shown in Table 2.
Urodynamic study
Urodynamic study was carried out on admission in 14 patients with micturition disturbances and 1 with only increased PVR urine; 4 had DA, 6 had DH with high-pressure voiding and remaining had increased PVR urine.
Detrusor areflexia
Bladder capacity in this group ranged between 385 and 501 ml (mean 457 ml) but compliance was normal in all. Three patients failed to void on command (end filling pressures 12, 28 and 5 cm of water). In the fourth patient, maximum detrusor pressure (Pdet) was 27 cm of water. Sensation of bladder filling was absent in one but appeared in three patients at 193, 467 and 104 ml. Two patients had acute deterioration in neurological symptoms (patient no. 10 and 12). Lower limbs were flaccid in one, spastic in three and wasted in one patient who had arachnoiditis on MRI. All four patients had brisk tendon reflexes in lower limbs. Sensations of pinprick and joint position were impaired in all the patients. Autonomic dysfunction in the form of postural drop of blood pressure and trophic skin changes was present in two patients.
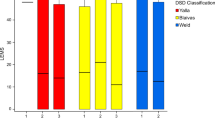
DH with high-pressure voiding
This type was present in six patients (Figure 1) and two of whom had absent bladder sensation. Bladder capacity ranged between 128 and 388 ml (mean 244 ml). All six patients leaked during instability. Detrusor leak point pressures ranged from 40 to 175 cm (90.83±46.09 cm) of water, and leak point volumes 67 to 220 ml (152.83±58.72 ml). Volume of bladder filling at which first unstable contraction appeared was 67–231 ml (154.43±58.8 ml). Pdets at first unstable contraction was 30–175 cm (76.43±51.86 cm) of water. Max Pdets ranged from 40 to 175 cm (91±46 cm) of water. In two patients with absent bladder sensation, maximum bladder capacity was 187 and 388 ml, Max Pdet 40 and 175 cm of water, respectively; and both of them were unable to void on command. In two patients, voiding phase could not be studied as one voided completely at 220 ml due to detrusor instability and the other failed to void on command due to disability and supine position. Lower limb spasticity was noted in five and hypotonia in one patient; lower limb hyperreflexia was present in all the patients. One patient had bilateral calf wasting. Dysautonomia in the form of trophic skin changes and postural hypotension was present in three patients.
Three patients did not have any detrusor function abnormality; two had high PVR urine—100 and 120 ml; first filling sensation appearing at 154 and 129 ml, respectively. Both the patients voided on command and Max Pdet was 46 and 45 cm of water, and maximum bladder capacity was 455 and 300 ml, respectively. Bladder compliance was normal. Lower limb tone and reflexes were normal in one and increased in the other. The third patient had high-pressure poor flow voiding with high PVR urine. His first bladder sensation appeared at 186 ml; Max Pdet was 106 cm of water, maximum bladder capacity 307 ml, normal compliance and PVR urine was 140 ml.
One patient (no. 5) had normal urodynamic study at the time of first evaluation. The patient whose urodynamic study was not possible had PVR urine of 130 ml (by catheterization). He had flaccid areflexic weakness and wasting of legs. The details of clinical, MRI and urodynamic findings are presented in Table 1.
Follow-up
All the patients were clinically followed up at 1 year and follow-up urodynamic study was carried out in three patients; in one patient, DA was replaced by DH with high-pressure voiding. This patient in follow-up study had absent bladder sensation, detrusor instability with leak and voided completely at 100 ml (Figure 2). In the other two patients, DH persisted and maximum bladder capacity was 396 and 157 ml. One patient voided completely at 157 ml and the other had high-pressure poor flow voiding. The symptoms of bladder dysfunction as assessed by AUAS score revealed significant improvement in all the patients at 6 (P=0.0001) and 12 months (P=0.0001). On separately comparing patients based on their urodynamic category (normal, DA and DH with high-pressure voiding), only patients with DH with high-pressure voiding had significant improvement in their AUAS scores at 6 (P=0.003) and 12 months (P=0.000) (Table 3).
Urodynamic study of the patient no. 10. Detrusor areflexia (a) converted to detrusor hyperreflexia (b) at 8 months. (c and d) Spinal MRI, T1 contrast in sagittal and axial section of the same patient showing destruction of C7-D3 vertebrae with anterior and posterior soft tissue swelling resulting cord compression. There is enhancement of spinal meninges and loculations (in axial section) suggestive of arachnoiditis.
Clinical, radiological and urodynamic correlation
The pattern of bladder dysfunction on urodynamic study did not correlate with severity of paraplegia (P=0.41), tone (P=0.49), Barthel Index score (P=0.49) and location of MRI abnormality (P=0.48). Walking Index for Spinal Cord Injury scores improved at 6 (7±9.31–11.8±9.24; P=0.02) and 12 months (7±9.31–13±9.54; P=0.02). At 1 year, six patients had complete, five had partial and four had poor recovery. The patients with micturition disturbances had worse outcome at 1 year compared to those without micturition disturbances (P=0.006); but among the patients with micturition disturbances, the type of bladder dysfunction was not related to outcome (P=0.52).
Discussion
In this study 50% patients with spinal tuberculosis had micturition disturbances. On urodynamic study, bladder dysfunction could be categorized into (1) DH with high-pressure voiding in 42.8%, (2) DA in 28.6% and (3) normal urodynamic study in 28.6% patients. The patients with micturition disturbances had poorer outcome compared to those without micturition disturbances. Spinal tuberculosis, though, is a common cause of paraplegia but bladder dysfunction studies have not received much attention. In a study on 32 children below 16 years of age who had spinal tuberculosis, 8 had paraplegia with bladder and bowel dysfunction.2
In spinal tuberculosis, paraplegia occurs due to diverse pathologies with varying temporal course; acute mechanisms include infarction, subluxation of vertebrae, wedge collapse and abscess formation; whereas more protracted neurological deficit is due to granuloma, arachnoiditis and myelopathy.8, 9 Transspinal pathways connect the pontine micturition center to spinal cord that are important for reciprocal activity of detrusor and sphincter for proper storage and voiding functions. After spinal cord damage, the pontine micturition center is disconnected from spinal cord resulting in co-contraction of detrusor and sphincter. In due course, new reflexes emerge to overcome detrusor sphincter dyssynergia to drive the bladder emptying that results in DH.
We have categorized our patients as DH with high-pressure voiding because sphincter EMG was not possible. One of our patients, who had DA, developed DH at 8 months follow-up. Abnormally overactive, small capacity bladder is typical of spinal cord disease and clinically manifests with storage dysfunctions that were present in majority of our patients. In our study, urodynamic findings did not correlate with MRI changes. Similar observations were noted in acute transverse myelitis,6 spinal cord injury, disk disease, tropical spastic paraplegia and multiple sclerosis.10, 11, 12 In a study on spinal cord injury above sacrum, 94.3% patients had DA and detrusor sphincter dyssynergia, and 4.18% had low compliance bladder. Conversely, the patients with spinal injury presented with DA in 85.7% and low compliance bladder in 78.5%. Combined sacral and suprasacral pathology resulted in DH and detrusor sphincter dyssynergia in 67.9% and DA in 27.3%.11 All our patients had suprasacral pathology on MRI and we did not find a significant relationship of bladder dysfunction with the level of spinal cord involvement. In our study, four out of six patients with involvement at or below D6 spinal level had DH, whereas two patients who had spinal cord involvement above D6 presented with DA; however, at follow-up these patients had DH. This can be attributed to diversity of pathology (acute versus chronic) and variable evolution of local reflexes that could be delayed by presence of infection and bedsore, though latter factors were not found in our patients. One patient each with DA, however, had lower limb wasting and hypotonia suggesting associated tubercular arachnoiditis.
Spinal tuberculosis is amenable to antitubercular therapy and the role of surgery is still controversial.13, 14, 15 A study from the United States recommended decompression and stabilization surgery for the patients with Pott's spine having neurological symptoms and signs. Most of the patients in that study improved but two died.16 In another study with patients having more severe Pott's paraplegia, 29 out of 43 had good outcome at 6 months on conservative treatment and none died.9 In this study, all the patients without micturition abnormality improved and 9 out of 15 patients with micturition disturbance improved completely or partially and the remaining also showed progressive improvement. In four patients, urodynamic study was normal, and the only abnormality was increased PVR urine. Increased PVR urine and elevated leak point pressure above 40 cm of water may result in upper urinary tract damage. In four out of five patients with DH, leak point pressure was significantly elevated (mean 90.8 cm of water), although no evidence of upper tract damage was found on ultrasound and kidney function tests. For some unknown reasons, upper urinary tract involvement is not as common in spinal cord infections as in spinal cord injury.6, 17 Because of high PVR urine and low compliance, six patients were advised clean intermittent catheterization and only three needed it at 6-month follow-up.
In our study 50% patients with spinal tuberculosis had bladder dysfunction that was associated with poor outcome. The urodynamic changes are nonspecific and tend to improve. Attention to urinary symptoms and urodynamic findings is useful for the management of these patients.
References
Davidson PT, Horowitz I . Skeletal tuberculosis. A review with patient presentations and discussion. Am J Med 1970; 48: 77–84.
Mushkin AY, Kovalenko KN . Neurological complications of spinal tuberculosis in children. Int Orthop 1999; 23: 210–212.
Misra UK, Sharma VP, Singh VP . Clinical aspects of neurolathyrism in Unnao, India. Paraplegia 1993; 31: 249–254.
Mahony FE, Barthel DW . Functional evaluation: the Barthel index. Md State Med J 1986; 14: 61–65.
Barry MJ, Fowler Jr FJ, O’Leary MP, Bruskewitz RC, Holtgrewe HL, Mebust WK et al. The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. J Urol 1992; 148: 1549–1557.
Kalita J, Shah S, Kapoor R, Misra UK . Magnetic resonance imaging and bladder dysfunction in acute transverse myelitis: neurophysiological and urodynamic correlations. J Neurol Neurosurg Psychiatry 2002; 73: 154–159.
Misra UK, Kalita J . The role of sensory and motor evoked potentials in the prognosis of Pott's paraplegia. Clin Neurophysiol 2004; 115: 2267–2273.
Shridhar K . Tuberculosis of the spine. In: Ramamurthi B, Tandon PN (eds). Textbook of Neurosurgery, vol I, 2nd edn. BI Churchill Livingstone: New Delhi, 1996, 496–513.
Kalita J, Misra UK, Mandal SK, Srivastava M . Prognosis of conservatively treated patients with Pott's paraplegia: logistic regression analysis. J Neurol Neurosurg Psychiatry 2005; 76: 866–868.
Dong D, Xu Z, Shi B, Chen J, Jiang X, Wang H . Urodynamic study in the neurogenic bladder dysfunction caused by intervertebral disk hernia. Neurourol Urodyn 2006; 25: 446–450.
Weld KJ, Dmochowski RR . Association of level of injury and bladder behavior in patients with post-traumatic spinal cord injury. Urology 2000; 55: 490–494.
Kim YH, Goodman C, Omessi E, Rivera V, Kattan MW, Boone TB . The correlation of urodynamic findings with cranial magnetic resonance imaging findings in multiple sclerosis. J Urol 1998; 159: 972–976.
Moon MS, Ha KY, Sun DH, Moon JL, Moon YW, Chung JH . Pott's paraplegia—67 cases. Clin Orthop 1996; 323: 122–128.
Moula T, Fowles JV, Kassab MT, Sliman N . Pott's paraplegia: a clinical review of operative and conservative treatment in 63 adults and children. Int Orthop 1981; 5: 23–29.
Turgent M . Spinal tuberculosis (Pott's disease): its clinical presentation, surgical management and outcome. A survey study on 694 patients. Neurosurg Rev 2001; 24: 8–13.
Rezai AR, Lee M, Cooper PR, Errico TJ, Koslow M . Modern management of spinal tuberculosis. Neurosurgery 1995; 36: 87–98.
Fowler CJ, Brady CM, Frohman EM, Sakakibara R, Stewart JD . Neurologic bladder, bowel and sexual dysfunction. In: Munsat TL (ed). World Federation of Neurology, Seminars in Clinical Neurology, vol 1. Elsevier Science: Amsterdam, the Netherlands, 2001, 50–62.
Acknowledgements
We thank Mr Rakesh Kumar Nigam for technical help.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kalita, J., Misra, U., Kumar, G. et al. Bladder dysfunction in spinal tuberculosis: clinical, urodynamic and MRI study. Spinal Cord 48, 697–703 (2010). https://doi.org/10.1038/sc.2009.199
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2009.199
Keywords
This article is cited by
-
Magnetic Resonance Image findings of Spinal Tuberclosis at first presentation
International Archives of Medicine (2014)