Abstract
Study design:
A retrospective study.
Objectives:
To study the outcome of repair of cauda equina fibres with fibrin glue after lumbar fracture and/or dislocation.
Methods:
Seven acute cases and one chronic case of L2 or L3 fracture and/or dislocation complicated with complete cauda equina injury were selected. Sural nerve or ventral roots of injured cauda equina were chosen to repair the motor cauda equina fibres with fibrin glue after open reduction and internal fixation of the unstable vertebrae. The functional recovery after surgery was observed.
Results:
Recovery of the strength of thigh muscles (iliopsoas, quadriceps femoris, gluteus maximus, adductors) was observed in all seven acutely injured patients (t=3.74, P<0.05), but not in the chronic one. Neither recovery of leg muscles nor sensation of the lower extremities was observed in any case.
Conclusions:
The cauda equina ventral roots injured after lumbar fracture and/or dislocation can be repaired with fibrin glue and motor recovery is expected.
Similar content being viewed by others
Introduction
Fracture and/or dislocation of vertebrae L2/3 is a unique level of injury where spinal cord proper ends and cauda equina begins. These vertebral injuries may cause damage to only cauda equina. Cauda equina shares common neural structures with peripheral nerves. If anastomosing the torn ends of its nerve roots is successful, neurological recovery of all functions of lower extremities, pelvis and pelvic organs innervated by spinal nerves L2 to S5 should be possible at this level. Conventionally, bone injuries are properly dealt with, whereas the associated injury of cauda equina is left unattended and allowed to find its own way to heal.1 Very few attempts have been made to connect torn nerves by microsuture.2, 3, 4 Even when such attempts were made, they were rarely successful, because, unlike peripheral nerves,5 cauda equina nerve roots lacked perineurium to hold the sutured ends securely together. In view of the poor neurological recovery with both of the above-mentioned approaches, particularly in complete injuries, attempt was made by the authors to find a better method of anastomosis to improve outcome. As fibrin glue has been approved by US Food and Drug Administration and used successfully in repairing cranial nerves and other tissues clinically,6, 7 we decided to use it to join the torn ends of nerve roots of cauda equina with the hope of improving the outcome of anastomoses and hence neurological recovery. The study results constitute the content of this report.
Patients and methods
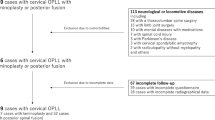
We retrospectively selected and reviewed eight patients admitted to the Department of Orthopedics of Beijing Army General Hospital from 2002 to 2004 who fulfilled the following criteria for this study.
-
1)
Vertebral injury was L2 or L3 fracture/dislocation.
-
2)
All patients could walk before the incident.
-
3)
The injury was complete with American Spinal Injury Association Impairment Scale (AIS) A.
-
4)
In addition to operations on relevant vertebrae, all nerve roots from L2 to S5 were repaired surgically.
-
5)
Follow-up was 2 years or longer.
-
6)
Availability of acknowledged informed consent.
Of the eight patients, six were men and two were women. The age at the time of operation ranged from 21 to 46 years (33.3±8.1 years). Five patients sustained L2, whereas the other three patients had L3 fracture/dislocation. The characteristics of these patients are presented in Table 1. Seven patients were operated upon in the acute stage. The time from injury to operation ranged from 3 to 7 days (4.14±1.46 days). One patient had an old injury and was operated upon 2.6 years after the incident. This patient had an L3 fracture/dislocation.
American Spinal Injury Association Impairment Scale was used for patient selection (Table 1).8, 9 However, this scale only tests a group of muscles and hence was not appropriate for assessing the strength of individual muscles that this study required. In view of this, individual muscle strength was also tested using the Medical Research Council method.10
In addition, recording of the somatosensory evoked potentials of tibial, peroneal and femoral nerves was carried out in all patients. As all nerve roots below L1 were repaired, including S3–5, the functions of pelvis and pelvic organs, particularly lower urinary tract, were also studied. However, special methods of urological rather than neurological assessment were needed. The results of these assessments are more suitable for a separate study.
Repairing nerve roots of cauda equina is a delicate procedure that requires a comfortable and stable environment. For this purpose, the following necessary steps were followed before the procedure.
-
1)
Reposition realignment of damaged vertebrae to create space for manipulation, and restore normal arrangement of nerves as much as possible. This would facilitate easy and correct identification of relevant nerve roots.
-
2)
Two to three vertebrae were fixed with pedicle screws and rods or plates to stabilize the segment of interest for accurate manipulation. Bone grafting was carried out between segments L2 and L4.
-
3)
Decompressive laminectomies11 of L2/3 and neighbouring vertebrae were carried out for ample and easy access to the spinal canal and its contents.
-
4)
Discectomy and partial corpectomy were carried out through the laminectomy opening to further relieve entrapped and compressed nerves and create more space for delicate manipulation.
-
5)
Longitudinal incision of the dura was made to expose intrathecal contents.
All anterior roots at fracture level were observed to be torn or severely bruised. A section about 5 mm at the ruptured or bruised end seemed translucent, indicating a void of its contents. The continuity of all posterior roots was intact but bruised. Repair of the cauda equina was carried out under an operative microscope of × 4 magnification. All contused tissues were removed with microsurgical instrument and the end was trimmed to normal-appearing tissue. This left a gap of about 10 mm between nerve ends12 to be filled (Figure 1). A segment of sural nerve was harvested to bridge the gap in five patients with recent injuries. In other two fresh and one chronic case, sensory nerve fibres from the cauda equina were used to fill the gap of motor nerve fibres as nerve graft. In general, two or three bundles of sensory nerve fibres were sufficient to bridge one bundle of motor nerve fibres.
The epineurium was cleared and the nerve ends were glued together from end to end with fibrin glue, which is composed of thrimbase and human fibrinogen and provided by Immuno (Vienna, Austria). It could coagulate in 3–5 s when the ends of nerve fibres were polymerized in vivo. A 1 ml tuberculin syringe was used to apply the glue accurately so that no excessive amount was left at the site of anastomosis. Too much glue would enlarge the distance between the nerve ends and make regeneration of nerve fibres through the extra distance of the glue difficult. The difference in appearance between sensory and motor roots was obvious under the microscope. This would naturally avoid cross-anastomosis between them by mistake. However, motor roots of different levels looked so similar that it was almost impossible to differentiate between them. However, some nerve roots were easier to identify than others by the shape, length and approximation of the stumps. Tracing the distal stumps to their exit was possible at the level of decompression and not far beyond. By carefully combing the damaged nerve roots, their origin could be roughly located according to their lateral-to-central arrangement. A slight straightening of the roots helped to restore them to near normal arrangement for identification. The origin and exit of nerve roots far beyond the decompression window could be estimated only with less certainty. In our case, after careful observation and anastomoses, only 1–2 nerve roots were left without clear identification. This did not seem to matter too much, as most of the work was correctly carried out. The remaining one or two might also be correct or the overlapping of innervation might compensate for minor errors in anastomosing neighbouring roots. Locating the exact level of the severed motor roots would be ideal but it requires extensive exposure. Such excessive exposure would have added unnecessary trauma to an already major operation. Owing to segmental overlapping innervation of the spinal cord and its nerve roots and neural plasticity, it was believed that cross-anastomosing neighbouring motor roots would not compromise the outcome significantly. Bearing this in mind, anastomosis of motor roots of exactly the same level was not pursued during the operation.
Special attention was paid to the axial and longitudinal orientation of nerve ends. This was assured using corresponding anatomical landmarks and surgical markings, such as binding the motor nerve roots with suture, to avoid connecting the motor nerves with sensory ones, and twisting the nerves.
This technique simplified the procedure of anastomosis to a great extent and caused only minor damage to nerves. The simplicity and efficiency made it possible to complete the operation of repairing all cauda equina nerve roots from L2 to S5 of both sides (18 altogether) and all other procedures in less than 4 h.
The follow-up period ranged from 24 to 36 months, with a mean of 26.5±3.92 months.
Preoperative and postoperative muscle strength of iliopsoas, quadriceps, gluteus maximus, adductors, gluteus medius, tibialis anterior, gastrocnemius, tibialis posterior and peroneal muscles of both sides were tested, recorded, compared and analysed. Statistical analysis was performed using SPSS 16.0 statistical software package (SPSS Inc., Chicago, IL, USA), paired sample t-test.
Results
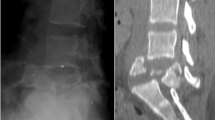
In all the eight cases, the spinal canal was restored to its original sagittal diameter (Figure 2).
Details of recovery of individual muscle strength of both lower extremities based on the Medical Research Council scale are presented in Table 2. In all the seven acute patients, the order of recovery does not follow myotome from top down, it rather follows the distance between the site of anastomosis and the muscle from short to long. The gluteus maximus that is mainly innervated by S1 had good recovery, whereas the tibialis and peroneal muscles innervated by higher nerve roots did not. There was no significant difference between the sides (left and right), but there was a significant improvement postoperatively in all thigh muscles, except the gluteus medius. In the chronic case, there was no recovery in any of the muscles (Table 2).
There was no recovery of sensation after repair. It was supported by somatosensory evoked potential results.13 No amplitude was recorded from tibial and peroneal nerves in any of the patients. As to femoral nerves, no amplitude was recorded in six patients. In the remaining two patients with L3 acute injury, decreased amplitudes were recorded and the latent period was prolonged.
Recovery of nerve roots S3—5, which innervate sacral area, the pelvis and pelvic organs, was also observed after their repair warranted a separate report.
Discussion
Repositioning and realignment of damaged vertebrae and decompression of the spinal canal and the dural sac alone are not sufficient to bring the ends of severed nerves close enough to achieve satisfactory regeneration and recovery of function that may follow. Since 1960, much research2, 3, 14 has been conducted on intervening directly by repairing severed or severely bruised cauda equina fibres in lumbar fracture/dislocation. More satisfactory recovery is expected from this direct approach, as nerve roots simulate peripheral nerves structurally.
However, the reported results of surgical anastomosis of damaged nerve fibres by microsuture were not entirely satisfactory.2, 3 The microsuture method has the following pitfalls:
-
a)
The unabsorbable suture constitutes a permanent foreign body that may compromise healing of anastomosis, and in worse case, even hamper regeneration.
-
b)
It is more difficult to perform anastomosis with suture because of the shortage of connective tissue in nerve roots compared with peripheral nerves outside the spinal canal. Surgery under difficult circumstances may cause unnecessary damages to the already damaged nerves.
-
c)
Blood supply to nerves may be compromised if blood vessels are caught by stitches.
The pattern and degree of recovery of muscle strength did not follow the myotome simply because at L2 or L3 vertebral level, the spinal cord ends and segmental innervation becomes irrelevant. They rather followed the distance from the site of anastomosis to the target muscles. This was in line with the process of regeneration of peripheral nerves, as nerve roots simulate them structurally.
As generally acknowledged, the peripheral nerve grows around 1 mm a day; within 1.5–2.0 years, it can grow up to approximately 55–60 cm. As endplate atrophies within 1.5 years after injury, no peripheral nerve can grow to restore muscle function after that period. This stresses the importance of early repair of damaged nerve roots after injury. The distance from L2/3 vertebra to the knee joint in an average adult is about 60 cm. That was why muscles below the knee joint did not recover. The first muscle to recover was iliopsoas at 92 days after the operation. It was followed by other muscles above the knee joint: quadriceps femoris, gluteus maximus and adductor, in that order.
The fact that restoration of motor function was much better than sensation in our study was consistent with the results of many other reports.15, 16 Following are only a few possible explanations: the alien environment of the central nervous system, particularly glial cells, may have hampered the growth of sensory axons into the spinal cord, whereas the axons of the motor neuron grow in the same environment of the peripheral nerve system. The mechanism of such failure is complex and much remains to be explained. Moreover, the environments of neurons nourishing sensory root and motor root are different. Motor neurons in the anterior horn have more abundant blood supply than neurons of the dorsal ganglion that floats in a pool of cerebrospinal fluid of the subarachnoid space. Cullheim et al.17 noted that axon growth from a glial scar stopped at the borderline between the scar and the normal posterior fasciculus. Other reports also showed stoppage of growth at the dorsal root entry zone. The presence of nerve fibres confirmed that the regenerating sensory fibres did indeed originate from the dorsal root ganglion, en route to the spinal cord, and passed through the dorsal root entry zone and the peripheral nerve system–central nervous system barrier. The dorsal root entry zone is the place where the supporting structure of the nervous tissue (neuroglia), consisting of a fine web of tissue, encloses neuroglial cells, which are of three types: astrocytes, oligodendrocytes and microcytes. This is also where axonal growth is inhibited because the axons either turn around along the dorsal root or form swollen end bulbs abutting the astrocytes.18 Full explanation is not only far beyond the scope of this report but also unavailable based on existing scientific data. Raisman and colleagues19, 20 are working on using olfactory ensheathing cells to overcome the barrier after spinal cord injury. It is a task of further intensive and extensive research for a long time to come. However, at the current status of science, those sensory nerve roots that fail to regenerate functionally can be used to bridge the gap between severed ends to repair motor roots, and enhance the chance of functional recovery after motor nerve root repair. This procedure also makes the repair much simpler and salvages the sural nerve.
Owing to the nature of cauda equina that is similar to that of peripheral nerves, surgical repair is preferable as early as possible;21 if total transection is confirmed, as seen in our cases, early repair should bring about better results. With modern surgical technique under the microscope, there is negligible danger that any remnant nerve fibres can be overlooked and hence cut or damaged by accident. This is different from the observation period needed for injury of spinal cord proper, in which the damage inside the cord cannot be seen and hence accurate assessment of damage is impossible.
Conclusion
The preliminary results of connecting torn cauda equina nerve roots with fibrin glue were encouraging in acute injuries. No recovery was observed in a chronic case. The method could be recommended for wider tests and use. In chronic cases, no improvement was observed to justify its use.
References
Hause M, Kikuchi S, Sakuyama Y . Anatomic study of their relation between lumbosacral nerve roots and their surrounding tissues. Spine 1983; 8: 50–58.
Meier C, Sollmann H . Regeneration of cauda equina fibers after transacted and end-to-end suture: light and electron microscopic study in the pig. J Neurol 1977; 751: 81–90.
Conzen M, Sollmann H . Reinnervation of the urinary bladder after microsurgical reconstruction of transected cauda fibers: an experimental study in pigs. Urol Res 1982; 10: 141–144.
Moy OJ, Peimer CA, Koniuch MP, Howard C, Zielezny M, Katikaneni PR . Fibrin seal adhesive versus nonabsorbable microsuture in peripheral nerve repair. J Hand Surg Am 1988; 13: 273–278.
Hart AM, Terenghi G, Wiberg M . Neuronal death after peripheral nerve injury and experimental strategies for neuroprotection. Neurol Res 2008; 30: 999–1011.
Wieken K, Angioi-Duprez K, Lim A, Marchal L, Merle M . Nerve anastomosis with glue: comparative histologic study of fibrin and cyanoacrylate glue. J Reconstr Microsurg 2003; 19: 17–20.
Brodbaker E, Bahar I, Allan R . Slomovic, novel use of fibrin glue in the treatment of conjunctivochalasis. Cornea 2008; 27: 950–952.
American Spinal Injury Association/International Medical Society of Paraplegia. International Standards for Neurological and Functional Classification of Spinal Cord Injury, Revised 2000. American Spinal Injury Association: Chicago, 2000.
Wyndaele JJ, Biering-Sörenson F . Standardizing to focus knowledge and improve communication on spinal cord care around the world. Spinal Cord 2008; 46: 767.
McRae R . General principles in the examination of a patient with an orthopaedic problem. In: McRae R (ed). Clinical Orthopaedic Examination, 5th edn. Churchill, Livingstone: Edinburgh, 2004, pp 1–10.
Delamarter RB, Sherman JE, Cair JB . Award in experimental studies cauda equina syndrome: neurologic recovery following immediate, early or late decompression. Spine 1991; 16: 1022–1029.
Mackinnon SE . Surgical management of the peripheral nerve gap. Clin Plast Surg 1989; 16: 587.
Conzen M, Sollmann H . Reinnervation after microsurgical repair of transected cauda equina fibers: an electromyographic study. Neurochirurgie 1985; 28: 6–7.
Steven K, Garfin Mark S . Nerve-roots of the cauda equina. J Bone Joint Surg 1990; 72A: 1185–1192.
Fujii E . Regeneration of the cauda equina after transection and end-to-end anastomosis in the dog. Nippon Seikeigeka Gakkai Zasshi 1995; 69: 43–52.
Moradzadeh A, Borschel GH, Luciano JP, Whitlock EL, Hayashi A, Hunter DA et al. The impact of motor and sensory nerve architecture on nerve regeneration. Exp Neurol 2008; 212: 370–376.
Cullheim S, Carlstedt T, Risling M . Axon regeneration of spinal motorneurons following a lesion at the cord–ventral root interface. Spinal Cord 1999; 37: 811–819.
Stensaas LJ, Partlow LM, Burgess PR, Horch KW . Inhibition of regeneration: the ultrastructure of reactive astrocytes and abortive axons terminals in the transition zone of the dorsal root. Prog Brain Res 1987; 71: 457–468.
Raisman G . Repair of spinal cord injury by transplantation of olfactory ensheathing cells. C R Biol 2007; 330: 557–560.
Raisman G, Li Y . Repair of neural pathways by olfactory ensheathing cells. Nat Rev Neurosci 2007; 8: 312–319.
Acknowledgements
All panel members (authors) volunteered their time and effort.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Sun, T., Liu, Z., Liu, S. et al. The clinical study of repairing cauda equina fibres with fibrin glue after lumbar fracture and dislocation. Spinal Cord 48, 633–637 (2010). https://doi.org/10.1038/sc.2009.195
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2009.195