Abstract
Study design:
A randomized controlled trial.
Objectives:
To determine the effectiveness of electrical stimulation (ES)-evoked muscle contractions superimposed on progressive resistance training (PRT) for increasing voluntary strength in the quadriceps muscles of people with spinal cord injuries (SCI).
Setting:
Sydney, Australia.
Methods:
A total of 20 people with established SCI and neurologically induced weakness of the quadriceps muscles participated in the trial. Participants were randomized between experimental and control groups. Volunteers in the experimental group received ES superimposed on PRT to the quadriceps muscles of one leg thrice weekly for 8 weeks. Participants in the control group received no intervention. Assessments occurred at the beginning and at the end of the 8-week period. The four primary outcomes were voluntary strength (Nm) and endurance (fatigue ratio) as well as the performance and satisfaction items of the Canadian Occupational Performance Measure (COPM; points).
Results:
The between-group mean differences (95% confidence interval (CI)) for voluntary strength and endurance were 14 Nm (1–27; P=0.034) and 0.1 (−0.1 to 0.3; P=0.221), respectively. The between-group median differences (95% CI) for the performance and satisfaction items of the COPM were 1.7 points (−0.2 to 3.2; P=0.103) and 1.4 points (−0.1 to 4.6; P=0.058), respectively.
Conclusion:
ES superimposed on PRT improves voluntary strength, although there is uncertainty about whether the size of the treatment effect is clinically important. The relative effectiveness of ES and PRT is yet to be determined.
Similar content being viewed by others
Introduction
Neurologically induced weakness is a common impairment after spinal cord injury (SCI). It imposes activity limitations and participation restrictions, both of which compromise quality of life.1, 2 It is believed that voluntary strength in the paretic muscles of people with SCI may be enhanced by an appropriate exercise program.1 The most widely used exercise program for this purpose is progressive resistance training (PRT). The key components of PRT are resistance, repetition and progression.3
PRT is effective in non-paralyzed muscles and is the key strategy used for strengthening the upper limb muscles of people with paraplegia.1, 2 However, its clinical efficacy for paretic muscles after SCI is less clear4 and it has only been investigated in two randomized controlled trials,1, 5 neither of which have provided conclusive evidence of benefits. It is commonly believed that the effectiveness of PRT may be enhanced through superimposed electrical stimulation (ES)-evoked muscle contractions. The addition of ES to PRT is usually justified by observed increases in stimulated strength or muscle hypertrophy in paralyzed muscle.6, 7, 8 However, there is no direct evidence from clinical trials to suggest that voluntary strength is increased by superimposing ES on PRT4, 9, 10 or by superimposing ES on any type of voluntary exercise in people with muscle paresis.11, 12, 13 Therefore, the primary purpose of this trial was to determine the clinical effectiveness of ES superimposed on PRT for increasing voluntary strength in the paretic quadriceps muscles of people with SCI.
Materials and methods
Participants
A total of 20 people with neurologically induced weakness in the quadriceps muscles after SCI were recruited from a community-based sample of convenience. Participants were referred to the study by community- and hospital-based therapists. The inclusion criteria were complete or incomplete SCI sustained more than 6 months before testing, at least 90° passive knee range of motion and moderate neurologically induced weakness in their quadriceps muscles of one leg that was responsive to ES (moderate weakness was defined as grade 3/5 or 4/5 on a manual muscle test14 and/or strength <2 s.d. below age-matched able-bodied individuals15). If both legs were suitable for inclusion, the weaker leg was selected for investigation. Exclusion criteria were recent history of trauma to the lower extremity, currently participating in a lower limb strength or ES training program or limited ability to comply.
A computer-generated random allocation schedule was compiled before commencement by a person not involved in the recruitment of participants. Participants’ allocations were placed in opaque, sequentially numbered and sealed envelopes that were held offsite by an independent person. Once a participant passed the screening process and completed the initial assessment, an envelope was opened and allocation was revealed. The participant was considered to have entered the trial at this point. The trial was registered with clinicaltrials.gov (ACTRN12609000079246). We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed.
Intervention
Participants in the experimental group received ES superimposed on PRT to the quadriceps muscles of one leg, thrice weekly for 8 weeks. All training was undertaken in participants’ homes with a portable device specifically designed for the trial (Figure 1). Participants were seated with their training leg strapped to the device. The device consisted of a lever arm attached to a wheel that applied a concentric constant torque throughout knee range of motion. The resistance to knee extension was applied through weights suspended from the wheel and was adjusted to match each individual's strength and training progression. A counterbalance was used to offset the torque due to the mass of the lower leg and lever arm.
The training device. The device consists of a wheel (A), weights suspended from the wheel (B) and a counterbalance (C) to offset the torque due to the mass of the lower leg and lever arm. The image was copied with permission from www.physiotherapyexercises.com.
ES was delivered through a STIWELL med4 portable neurostimulator (Otto Bock Healthcare Products, Vienna, Austria). Stimulation parameters were 50 Hz frequency, 300 μs pulse width and up to 100 mA stimulation amplitude (according to individuals’ tolerance to ES current density). The duty cycle was 50% of a 12 s on:off phase with non-ramped ES amplitude onset. Electrodes (7 × 13 cm) were placed over the participants’ quadriceps muscles at sites that evoked the strongest muscle contractions.
The intervention consisted of 12 sets of 10 knee extension repetitions. The first six sets involved ES superimposed on maximal voluntary knee extension. The second six sets involved ES-evoked muscle contractions alone. Resistance was applied throughout the range of motion and progressed between sets and sessions to ensure that the knee could only just be extended 10 times before fatigue limited knee extension. A short recovery of 2–3 min was provided between each set of 10 repetitions. Initially, some participants could not extend the knee 10 times with ES alone, despite the removal of all resistance. These participants were provided with manual assistance that was withdrawn as soon as possible. All sessions were directly supervised on a one-to-one basis by trained staff.
Control participants neither received PRT or ES to their lower limbs, nor did they have contact with research staff. However, both control and experimental participants were allowed to continue general fitness or mobility programs that they had been participating in before the trial. They were requested not to change their usual activities of daily living.
Assessment
All assessments were conducted at the beginning and end of the 8-week training period by assessors blinded to group allocation. An additional familiarization session was held a few days before initial testing. Four primary outcomes were used, including: (1) voluntary quadriceps strength (Nm), (2) voluntary quadriceps endurance (fatigue ratio), (3) the performance item of the Canadian Occupational Performance (COPM; points) and (4) the satisfaction item of the COPM (points). Three secondary outcomes were used, including: (1) ES-evoked quadriceps strength (Nm), (2) ES-evoked quadriceps endurance (fatigue ratio) and (3) participant perception of treatment effectiveness (points).
Muscle strength and endurance outcomes were measured using a Biodex Isokinetic System (Biodex Medical Systems, Shirley, NY, USA). This device automatically adjusted resistance to participants’ maximal efforts to maintain a constant pre-set angular velocity. The participants were tested in a seated position with their thighs and chests strapped and their arms crossed. Voluntary quadriceps strength was determined from the best of six trials of one-repetition maximum efforts at an angular velocity of 30 ° s–1. A 1-min rest was provided between each maximal contraction and a 5-min rest was provided after the six maximal contractions. Voluntary quadriceps endurance was tested by asking participants to maximally contract their quadriceps muscles for 3 s and then recover for 3 s and repeat the process for 3 min. Angular velocity was set at 20 ° s–1. The average strength (Nm) of the last five contractions was divided by the average strength of the first five contractions to derive a muscle fatigue ratio. A higher fatigue ratio represented greater quadriceps endurance. Throughout voluntary strength and endurance testing, participants were verbally encouraged and provided with instantaneous visual feedback about their torque production to maximize effort.
ES-evoked quadriceps strength and endurance were tested in the same way as voluntary strength and endurance but without voluntary effort. Stimulation was delivered at 140 mA amplitude (or up to an individual's maximum tolerable stimulation amplitude), but otherwise with the same ES characteristics as used during muscle training. The same stimulation intensity was used at pre- and post-assessments for each participant.
Participant perception of treatment effectiveness was assessed at the end of the 8-week treatment period by asking both control and experimental participants to rate their impressions of change in strength over the preceding 8 weeks on a 15-point scale, in which –7 indicated ‘a very great deal worse’, 0 indicated ‘no change’ and +7 indicated ‘a very great deal better’.16 The COPM17 determined participants’ perceptions about treatment effectiveness relative to self-nominated goals. At the start of the trial, all participants nominated three goals of treatment in terms of tasks related to knee strength. They rated each task on a 10 cm visual analogue scale with respect to their ability to currently perform the task and their satisfaction with their performance of the task. Participants were asked to repeat the ratings for each task at the completion of the 8-week period. In addition, at the end of the trial all experimental participants were asked to rate the inconveniences of training on a 10 cm visual analogue scale.
Statistical analysis
Power calculations were based on a comparable study18 indicating that 20 participants would provide an 80% probability of detecting a between-group difference equivalent to 15% of the mean baseline for voluntary quadriceps strength. This assumed mean baseline strength of 88 Nm, an s.d. of the between-group difference of 4.9 Nm,18 an α of 0.05 and a loss to follow-up of 15%.
All statistical analyses were performed using the principles of ‘intention to treat’. All data are reported as means (s.d.) unless skewed, in which case data are reported as medians (interquartile ranges). Significance was set at P⩽0.05 but results were interpreted with respect to pre-determined sufficiently important differences16 (defined as 15% of mean initial values for strength and endurance, 2 points for the COPM19 and 1 point for participant perception of treatment effectiveness).20 The sufficiently important differences for strength and endurance were set by the investigators after weighing up the time, cost and inconvenience of the intervention along with the real-life implications of improvements in strength. The purpose of all analyses was to determine the effect of group allocation (experimental and control) and time (pre and post) on outcome. Strength and endurance outcomes were analysed using four separate linear regression models with initial values entered as covariates. Time since injury was initially entered as a covariate but then discarded from the analyses after it became evident that it had no effect. The COPM results were skewed and therefore analysed using the Mann–Whitney test. The corresponding median between-group differences and 95% confidence intervals (CI) were calculated using bootstrapping techniques with 10 000 iterations.
Results
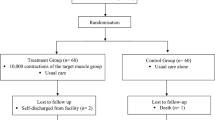
The median (interquartile range) age and time since injury were 39 years (26–50) and 3 years (2–7), respectively. All participants had motor incomplete lesions with neurological levels ranging from C5 to L2 as defined by the International Standards for Classification of SCI21 (Table 1). The flow of participants through the trial is shown in Figure 2. Outcomes were attained for all variables on all participants and there were no dropouts. On average, participants received a median (interquartile range) of 25 (24–25) training sessions over a mean (s.d.) of 8 (1) weeks.
Table 2 provides a summary of the results. The mean between-group difference (95% CI) for voluntary quadriceps strength was 14 Nm (1–27; P=0.034). The sufficiently important difference was defined a priori as 15% of mean initial strength (that is, 8 Nm). The 95% CI crossed the sufficiently important difference, indicating uncertainty as to whether the size of the treatment effect was clinically important. The between-group mean difference (95% CI) for participant perception of treatment effectiveness (a secondary outcome) was 4 points (2–6; P=0.000). The sufficiently important difference was defined a priori as 1 point. This result is statistically significant and clinically important. There were no other statistically significant or clinically important between-group differences for any of the other five outcomes (see Table 2 for details). The mean (s.d.) rating by experimental participants of the inconvenience of the training was 4 cm (2 cm) in which zero represents ‘not at all inconvenient’ and 10 cm represents ‘extremely inconvenient’.
Discussion
This is the first randomized controlled trial designed to determine the effectiveness of ES superimposed on PRT for increasing voluntary strength in the paretic muscles of people with SCI.4 The results indicate a statistically significant increase in voluntary strength, although there is uncertainty as to whether the size of the treatment effect is clinically important (the 95% CI spanned the sufficiently important difference of 8 Nm). The effects of ES superimposed on PRT on stimulated strength, stimulated endurance and voluntary endurance were equivocal. This may reflect the use of PRT that primarily targets voluntary strength and not endurance. The failure to find a convincing increase in stimulated strength may indicate limited change in muscle morphology or histochemistry. If this was the case, then the observed increases in voluntary strength may primarily be neural in nature.
Participants perceived that the treatment was effective. When participants were asked to explain their responses, they commonly cited improvements in their ability to move from sit to stand, to transfer and to clear the foot during swing phase of gait. However, these self-reports need to be interpreted with caution because participants were not blinded and possibly influenced by optimistic expectations of the intervention. Interestingly, participants’ perceptions about treatment effectiveness were not reflected in the results of the COPM, although this may partly reflect an insufficient sample size (for example, the 95% CI associated with the between-group difference of the COPM satisfaction item was wide and spanned the pre-determined sufficiently important difference of 2 points).
The effects of the intervention may have been more pronounced if the intervention had been delivered for more than 8 weeks. The results of strength training in the neurally intact muscles of able-bodied individuals suggest a 2% increase in strength for every week of training22 (the precise gains in strength are influenced by initial conditioning). The trainability of paretic muscles is not clear, although it is possible that the functional demands of daily living for people with paresis may impose limits on the effectiveness of PRT by reducing the dose-potency of the intervention.2 However, the situation might differ in people with recent SCI who have greater potential for neurological improvement and who are not yet routinely performing activities of daily living.
Although the intervention was only applied for 8 weeks, it was intensive. Each session took 1 h and was physically demanding for participants. In addition, the training involved both PRT and ES. This type and intensity of training was selected to provide a large contrast between control and experimental participants and hence the best possible chance of finding a treatment effect. It is disconcerting that despite the contrast between groups, there was still uncertainty as to whether the size of the treatment effect was clinically important.
The quadriceps muscles were selected for this trial because they have important implications for everyday mobility and are commonly affected by SCI. The quadriceps muscles were also used because they are a large muscle group and we had previously run into problems with statistical power related to reliably measuring torques in the small wrist muscles of people with tetraplaegia.5, 23 To avoid these problems, we also restricted the inclusion criteria to participants with grade 3/5 or 4/5 strength. It is not clear whether smaller and weaker muscles are more or less responsive to ES superimposed on PRT than larger and stronger muscles such as the quadriceps used in this trial. However, it is clear that large participant numbers will be required to conduct an adequately powered trial to answer this question.
This trial is not without its limitations. For example, a sample of convenience was used exposing the trial to the possibility of selection bias. Selection bias tends to overestimate treatment effectiveness. In addition, control subjects had less neurological impairment than experimental subjects with a higher proportion of American Spinal Injury Association classification D than C injuries (see Table 1). This difference occurred despite the randomization process and reflects differences in upper and lower limb strength of affected limbs. Importantly, there were only small differences in strength of the quadriceps muscles at randomization. Differences in overall upper and lower limb strength are only of concern if they influence the trainability of the quadriceps muscles. There is no evidence to suggest that this was the case, although it cannot be ruled out. There were no other differences in key prognostic factors such as age, time since injury or quadriceps strength.
The results of this trial provide initial support for the use of ES superimposed on PRT for increasing voluntary strength in the paretic quadriceps muscles of people with SCI, but there is uncertainty about whether the size of the treatment effect is clinically important. It is not clear whether ES was the critical component of the training program or whether the same results could have been attained with PRT alone.
References
Hicks AL, Martin KA, Ditor DS, Latimer AE, Craven C, Bugaresti J et al. Long-term exercise training in persons with spinal cord injury: effects on strength, arm ergometry performance and psychological well-being. Spinal Cord 2003; 41: 34–43.
Harvey L . Management of Spinal Cord Injuries: A Guide for Physiotherapists. Elsevier: London, 2008.
American College of Sports Medicine, Bryant CX, Mahler DA Kenney WL, Humphrey RH . ACSM's Guidelines for Exercise Testing Prescription. 5th edn. Williams and Wilkins: Baltimore, MD, 1995.
Harvey L, Lin CM, Glinsky J, De Wolf A . The effectiveness of physical interventions for people with spinal cord injuries: a systematic review. Spinal Cord 2009; 47: 184–195.
Glinsky J, Harvey L, Korten M, Drury C, Chee S, Gandevia SC . Short-term progressive resistance exercise may not be effective for increasing wrist strength in people with tetraplegia: a randomised controlled trial. Aust J Physiother 2008; 54: 103–108.
Shields RK, Dudley-Javoroski S . Musculoskeletal plasticity after acute spinal cord injury: effects of long-term neuromuscular electrical stimulation training. J Neurophysiol 2006; 95: 2380–2390.
Mahoney ET, Bickel CS, Elder C, Black C, Slade JM, Apple Jr D et al. Changes in skeletal muscle size and glucose tolerance with electrically stimulated resistance training in subjects with chronic spinal cord injury. Arch Phys Med Rehabil 2005; 86: 1502–1504.
Crameri RM, Weston A, Climstein M, Davis GM, Sutton JR . Effects of electrical stimulation-induced leg training on skeletal muscle adaptability in spinal cord injury. Scand J Med Sci Sports 2002; 12: 316–322.
Glinsky J, Harvey L, van Es P . Efficacy of electrical stimulation to increase muscle strength in people with neurological conditions: a systematic review. Physiother Res Int 2007; 12: 175–194.
Hamzaid NA, Davis GM . Health and fitness benefits of functional electrical stimulations—evoked leg exercise for spinal cord-injured individuals: a position review. Top Spinal Cord Inj Rehabil 2009; 14: 88–121.
Needham-Shropshire BM, Broton JG, Cameron TL, Klose KJ . Improved motor function in tetraplegics following neuromuscular stimulation-assisted arm ergometry. J Spinal Cord Med 1997; 20: 49–55.
Klose KJ, Schmidt DL, Needham BM, Brucker BS, Green BA, Ayyar DR . Rehabilitation therapy for patients with long-term spinal cord injuries. Arch Phys Med Rehabil 1990; 71: 659–662.
Kohlmeyer KM, Hill JP, Yarkony GM, Jaeger RJ . Electrical stimulation and biofeedback effect on recovery of tenodesis grasp: a controlled study. Arch Phys Med Rehabil 1996; 77: 701–706.
Daniels L, Worthingham C . Muscle Testing: Techniques of Manual Examination, 5th edn. Saunders: Philadelphia, 1986.
Murray MP, Gardner GM, Mollinger LA, Sepic SB . Strength of isometric isokinetic contractions: knee muscles of men aged 20–86. Phys Ther 1980; 60: 412–419.
Barrett B, Brown D, Mundt M, Brown R . Sufficiently important difference: expanding the framework of clinical significance. Med Decis Making 2005; 25: 250–261.
Law M, Baptiste S, McColl M, Opzoomer A, Polatajko H, Pollock N . The Canadian Occupational Performance Measure: an outcome measure for occupational therapy. Can J Occup Ther 1990; 57: 82–87.
Gregory CM, Bowden MG, Jayaraman A, Shah P, Behrman A, Kautz SA et al. Resistance training and locomotor recovery after incomplete spinal cord injury: a case series. Spinal Cord 2007; 45: 522–530.
Law M, Baptiste S, McColl M, Opzoomer A, Polatajko H, Pollock N . COPM The Canadian Occupational Performance Measure. Available from URL: http://www.caot.ca/copm/questions.html. (2005).
Schneider LS, Olin JT . Clinical global impressions of change. Clinical global impressions in Alzheimer's clinical trials. Int Psychogeriatr 1996; 8: 277–288.
American Spinal Injury Association. Reference Manual for the International Standards for Neurological Classification of Spinal Cord Injury. American Spinal Injury Association: Chicago, 2003.
Hubal MJ, Gordish-Dressman H, Thompson PD, Price TB, Hoffman EP, Angelopoulos TJ et al. Variability in muscle size and strength gain after unilateral resistance training. Med Sci Sports Exerc 2005; 37: 964–972.
Glinsky J, Harvey L, Korten M, Chee S, Gandevia SC . The addition of electrical stimulation to progressive resistance training does not enhance the wrist strength of people with tetraplegia: a randomized controlled trial. Clin Rehabil 2009; 23: 696–704.
Acknowledgements
This trial was funded by the Spinal Cord Injury and Other Neurological Conditions Research Grants Program of the NSW Office for Science and Medical Research. We acknowledge the assistance of Ray Patton and the Department of Biomedical Engineering at the Royal Rehabilitation Centre Sydney for designing and manufacturing the training devices.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Harvey, L., Fornusek, C., Bowden, J. et al. Electrical stimulation plus progressive resistance training for leg strength in spinal cord injury: A randomized controlled trial. Spinal Cord 48, 570–575 (2010). https://doi.org/10.1038/sc.2009.191
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2009.191
Keywords
This article is cited by
-
Early and intensive Motor Training for people with spinal cord injuries (the SCI-MT Trial): description of the intervention
Spinal Cord (2023)
-
Physiotherapy interventions for increasing muscle strength in people with spinal cord injuries: a systematic review
Spinal Cord (2019)
-
A preliminary investigation of mechanisms by which short-term resistance training increases strength of partially paralysed muscles in people with spinal cord injury
Spinal Cord (2019)
-
Effect of electrical stimulation on muscle atrophy and spasticity in patients with spinal cord injury – a systematic review with meta-analysis
Spinal Cord (2019)
-
Effect of tendon vibration during wide-pulse neuromuscular electrical stimulation (NMES) on muscle force production in people with spinal cord injury (SCI)
BMC Neurology (2018)