Abstract
Study design:
Radiographic analysis of sagittal spinal alignment of paraplegics in a standing position under surface neuromuscular electrical stimulation (NMES).
Objectives:
Describing the radiographic parameters of the sagittal spinal alignment of paraplegics going through a rehabilitation program with NMES.
Setting:
The University Hospital's Ambulatory (UNICAMP), Campinas, São Paulo, Brazil.
Methods:
Panoramic X-ray images in profile were taken for 10 paraplegics. All patients participated in the rehabilitation program and were able to perform gait through NMES of the femoral quadriceps muscles. The radiographic parameters used for the analysis were the same as those described in the literature for healthy people. The results were didactically organized into three groups: anatomical shape of the spine, morphology and kinetics of the pelvis and spinopelvic alignment.
Results:
The physiological curvature of the spine in paraplegics showed average values similar to those described in the literature for healthy patients. The inversion of the pelvic tilt and the increase in the sacral slope were defined by the anterior backward rotation of the pelvis. The existing theoretical mathematical formulas that define lumbar lordosis, pelvic incidence and pelvic tilt showed normal values, despite the anterior intense sagittal imbalance.
Conclusions:
The adaptive posture of the spine in paraplegics standing through the stimulation of the femoral quadriceps does not allow for a neutral sagittal alignment. This novel radiographic detailed description of the various segments of the spine can be of assistance toward the understanding of the global postural control for such subjects.
Similar content being viewed by others
Introduction
Spinal cord injury is a catastrophic event that affects mainly young individuals. In the United States, its prevalence is growing because of an increase in the lifespan of these patients due to advances in early and late multidisciplinary assistance.1 Current technology is allowing one to catch glimpses of the beginnings of a new dimension in the treatment of patients with spinal cord injury: (1) functional rehabilitation, where paraplegics are standing and sauntering under electrical stimuli2, 3 and (2) the attempt to regenerate the injured spinal cord tissue.4
Rehabilitation programs offer these patients the acquisition of postural reorientation from the use of the intact residual sensory-motor system, above the neurological damage.5 Potten et al.6 and Seelen et al.7 observed that in paraplegics, the loss of function of the erector spinae muscle is partially offset by an increase in electromyographic activity and hypertrophy of the latissimus dorsi and the upper third of the trapezius muscles.
The use of neuromuscular electrical stimulation (NMES) in paraplegics, to conduct exercises and to support their own weight, decreases the morbimortality. One observes that there is a cardiovascular conditioning improvement, an increase in bone mineral density,8 and a decrease in the risk of bedside ulcers.9 The simplest system for obtaining the bipedal posture in paraplegics uses open-loop NMES with stimulation of the knee extensors associated with AFO-type orthoses complemented by a bimanual hand support. New systems are being developed to eliminate two problems associated with NMES: muscle fatigue and non-functional bipedal posture due to the need for a hand support to maintain the posture and to achieve balance.10
Aiming at allowing an interaction with the environment, Matjacic and Bajd2 proposed a strategy to control the bipedal posture in paraplegics with hands free. Their theory model was based on a mathematical model of an interconnected double-inverted pendulum that ignores the mobility and shape of the spine and begins to accept the entire body segment above the hips as a single rigid structure.
In light of the knowledge of the authors, there are no descriptions in the literature about the current sagittal spinal alignment radiographical parameters in use directed specifically at paraplegics in a bipedal position under NMES.
The authors believe that although the complex spinopelvic dynamic control for the maintenance of sagittal alignment is lost in paraplegics, the postural adjustments arising from the use of the superficial dorsal muscles and of the non-injured erector spinae culminate in changes in the sagittal morphology of the spine that definitely need to be better understood with the ultimate goal of optimizing the postural rehabilitation and alignment.
Materials and methods
A total of 10 paraplegic patients were involved in this study. Written informed consent from each patient was obtained in accordance with the Declaration of Helsinki and with the prior approval of the ethics committee of the institution. The selection of patients was carried out from medical records and the imaging exams, among those who actively participated in the rehabilitation program of gait with NMES, in the Spinal Cord Injury Rehabilitation Ambulatory of the Department of Orthopaedia and Traumatology at the University Hospital of Campinas State University (UNICAMP), São Paulo, Brazil. The work was carried out during the first half of 2008.
The criteria for inclusion were complete paralysis, absence of scoliosis and pelvic obliquity, absence of visual or vestibular comorbidities and capacity of standing through NMES. All subjects were examined by only one of the authors (R Castro de Medeiros). Bone deformities and muscle shortening were discarded by classical orthopedic physical examination and joint X-rays obtained for exclusion of heterotopic ossification that limited the arcs of motion of the hips and knees. Finally, the spasticity was assessed by the modified Ashworth Scale.
Epidemiological, anthropometric and clinical data were collected and displayed in Table 1. To define the neurological level and the quantification of the total residual neurological function, the criteria of the American Spinal Injury Association (ASIA) were used.11 The seated height was measured from the ischium to the skull vertex with the patient in the supine position, with hips and knees flexed at 90°.
Neuromuscular electrical stimulation was generated with the following parameters: constant voltage, rectangular pulses of 300 μs, frequency of 25 Hz, amplitude ranging from 70 to 150 V and a load of 1 kΩ. It was used AFO-type orthesis, bilateral stimulation with two open-loop canals by transcutaneous NMES patches of the femoral quadriceps muscle, complemented by a bimanual hand support. Clinically, all of these enable plantigraded feet and extended knees.
To evaluate the sagittal spinal alignment of paraplegics, lateral panoramic X-rays were obtained at the Hospital's Radiological Department. All the roentgenograms were taken by the same professional, in a single machine, with the same technique. To standardize this procedure, a long chassis with a film of 36.5 × 91 cm remained at a fixed distance of 230 cm from the radiation source, which allowed exposure from the base of the skull to the proximal third of the femurs. The patients were placed in a standing position with NMES complemented by a bimanual hand support so that the right shoulder was toward the chassis and the face directed ahead. To try to reproduce the postural adjustments that precede the first moment of the start of a paraplegic gait, a bimanual hand support was placed at variable distances and heights, adjusted to the balance needs for each patient. To standardize the posture, the angle of flexion of the upper limbs with the vertical axis of the body was set at 25°. A conventional goniometer was used when performing the X-rays.
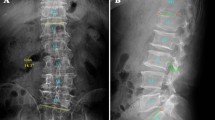
According to the principles of radiographic measurement of sagittal spinal alignment in the literature, several parameters were evaluated directly on conventional X-rays. Each X-ray was measured two times at different moments by two observers (R Castro de Medeiros and APB Jaccard) and the averages were used as a basis for each patient. The data were compiled into three categories: (1) anatomical shape of the spine, (2) morphology and kinetics of the pelvis and (3) spinopelvic balance. The definitions of the measured parameters are presented in Figure 1 and Table 2. The kyphosis and the plumb line located anterior to the posterior upper corner of S1 were represented by positive values, whereas negative values represent the lordosis and the plumb line posterior to the posterior upper corner of S1.
The averages and s.ds. were calculated from the generated data.
Results
All patients were male, presenting complete paralysis and a motor score of 50, according to the ASIA Scale. The neurological level ranged from T6–T10 and car accidents were the most frequent cause of injury. The average age was 36.6 years, average weight 81.6 kg, and average sitting height 92.6 mm. All of them had a history of more than 6 years of paraplegia and were involved in the rehabilitation program with neuromuscular electrical stimulation for at least 1 year (1–10 years) (Table 1).
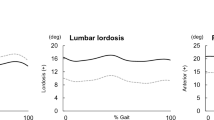
Averages and s.ds. of several radiographic parameters are shown in Table 3. Compared with several articles published in the literature on the ‘variation of normality’ of the sagittal spinal alignment in healthy volunteers (Table 4), the paraplegics showed absolute average values ‘within the normal range’ for thoracic kyphosis (35.8°), lumbar lordosis (−46.6°), lumbosacral lordosis (−53°), segmental lordosis, T12–PR lumbopelvic lordosis (−105.5°), the T4–T12 kyphosis/T12–PR lordosis ratio (0.3) and pelvic incidence (45.4°). By contrast, the paraplegics had average values ‘out of normality’ for the increased sacral slope (60°), inversion of the pelvic tilt (−15.9°), decrease of the sacrofemoral angle (18.4°), important anterior shift in all measured horizontal distances, inversion of the T9–hip axis (HA) sagittal tilt (−12.7°) and a decrease in spinal tilt (74.3°).
Finally, the theoretical mathematical formulas for defining lumbar lordosis (−47.9°), pelvic incidence (44.1°) and spinal tilt (93°), which suggest correlations presented in a balanced spine on healthy volunteers, also showed values considered ‘normal’ in paraplegics.
Discussion
The maintenance of the sagittal posture of the spine is dependent on static stabilizers (osteoligamentar system) and dynamic stabilizers (muscles) as well as neurological controllers. Several studies described the spinopelvic interrelations as major mechanisms for controlling the sagittal balance of the spine and of the body's gravity line.12, 13, 14 However, there is a wide variation for the values considered normal and little understanding about the true clinical significance of these variations.
Jackson et al.12 described the radiographic technique for measuring the pelvic radius, the kinetics of the pelvis and its correlation with the curvatures of the spine. According to this author, neurologically normal individuals regulate the sagittal balance of the spine and the balance through a coupled rotation-translation of the pelvis on the axis of the hips. Legaye et al.15 defined pelvic incidence as a constant geometric parameter, individual specific and as the sum of the sacral slope and the pelvic tilt. More recently, Roussouly et al.13 described the spinal tilt. According to this author, no correlation was found between the positions of the C7 plumb line and the line of body gravity, the latter being related to the spinal tilt, regardless of the value of the sacral slope. Finally, Schwab et al.14 analyzed the sagittal balance and the line of gravity in relation to the feet in accordance with the theory of cone-saving of Dubousset and concluded that every spinopelvic compensation has as its ultimate goal the maintenance of the line of gravity in a close relationship with the position of the feet.
Toward surmounting those concepts to assess the sagittal balance in paraplegics, sensory-motor deficits, lack of balance, spasticity and non-coordinated pathological reflexes were observed. Although obtaining postural control and balance in paraplegics has been attempted through NMES, Matjacic et al.10 observed that the strategy is effective only when it incorporates the voluntary and reflex actions of the neurologically intact upper body. For them, the balance in paraplegics in a standing position can be obtained through the ‘strategy of the hips’ in a double-inverted pendulum. In this model, the pendulum of the lower limbs translates taking the pelvis along so that the pelvic tilt is passively obtained from the change in the position of the hips in the upper pendulum's center of gravity (proximal part of the body), which would remain balanced with the axis of the feet. From the point of view of the paraplegic gait, there is a need for the use of the upper limbs for the control and support of part of the body weight. However, the overloading of the upper limbs causes later injuries to the shoulders with consequent pain and further functional disability.16
Analyzing the spine's anatomical-structural characteristics of spinal cord injured patients with stimulation to the quadriceps, ‘normal values’ were found for thoracic and lumbar sagittal curves. As there are no coordinated postural reflexes and the body weight was not supported only by the lower limbs, these findings might represent a partial adaptive postural control from the functioning paravertebral muscles remaining, but with no functional effectivity to support the body weight. The sagittal alignment found would be because of the sum of anatomical characteristics of the bodies and intervertebral disks,17 the viscoelastic properties of the discoligamentar components of the spine, the hypertonia spasticity-type at the paravertebral muscles, the postural muscle activity acquired by the latissimus dorsi and trapezium,6, 7 the support effect exerted by the support of upper limbs, the action of gravity and the characteristics of the morphokinetics of the pelvis.
In the morphokinetic parameters of the pelvis, the increased sacral slope, the inversion of the pelvic tilt and the decrease of the sacrofemoral angle reflect a great anterior rotation of the pelvis, which means flexion of the hips with the superior plateau of S1 positioned anterior to the hip's axis. According to Schwab et al.,14 the line of gravity in healthy subjects is anterior to all vertebral bodies and in close relation to the center of the hips. In paraplegics, that would generate a flexor moment over the hips that could not be offset by the anti-gravitational paravertebral and extensor hip muscles. An additional possible causal factor for the anterior rotation of the pelvis would be the contraction of the reflex portion of the rectus femoralis because of NMES to the quadriceps, which would ensure some postural resistance to the hips.
The spinopelvic parameters represent the final outcome of the balance drawn from the adaptive changes of sagittal curvatures of the spine and the pelvic tilt. In this study, the identification of the high positive values for the horizontal distances C7–S1, C7–HA, T4–L4 and T4–HA as well as an inversion of the spinal tilt defines the presence of a significant anterior sagittal imbalance. Despite all the above findings, the theoretical formulas for defining the lumbar lordosis (LL=0.8SS), pelvic incidence (PI=SS+PT) and spinal tilt (ST=99−0.1SS) resulted in values considered ‘normal,’ as described in the literature for healthy patients.
A pattern, not yet described in the literature, about the posture adopted by complete paraplegics with the mid-thoracic level under NMES was found in this study and it does not follow the theories previously described.2, 14 It could be summarized as follows: patients failed to achieve the ‘strategy of the hips,’ remaining with an apparently fixed flexion of the hips; sagittal curvatures of the spine presented ‘normal values,’ but that does not offset the pelvic effects; and large anterior sagittal imbalance supported by the upper limbs (Figure 2).
Contradicting the previous models, van der Spek et al.18 reported that the degree of stabilization of the hips and the distance of the position of the crutches to support paraplegics did not influence in a statistically significant way either the posture adopted by the patients or the force applied to the crutches, although they did allow a stable orthostatic posture. These authors still suggest that the flexibility of the spine and the effect of lumbar paravertebral muscles are fundamental for postural stability and load bearing and that the new models should include these variables to optimize the control of the postural balance.
In this study, the angle of 25° of flexion of the upper limbs with the vertical axis of the body was adopted on the basis of the average of the goniometric measurements for the upper limbs’ placement that precede the first moment of the start of the paraplegics’ steps participating on this and previous studies.19
Hopefully, the understanding of the adaptive sagittal spinal alignment presented in this study will contribute to the development of new strategies for postural control, either through intercostal neurotizations20 or through paravertebral stimulation, and the last one is under investigation.
Conclusion
Although several studies focus on the benefits of using NMES for the rehabilitation of patients with spinal cord injury and try to develop strategies to control postural alignment, there are no references in the literature to the rather important role of the spine in achieving those goals.
The strategies that will be developed should deal with the knowledge of this new paradigm: spine with anterior sagittal imbalance, anterior pelvic tilt with intense hip flexion and sagittal spine curvature seemingly normal, but non-functional.
Conflict of interest
The authors declare no conflict of interest.
References
Nobunaga AI, GO BK, Karunas RB . Recent demographic and injury trends in people served by the model spinal cord injury care systems. Arch Phys Med Rehabil 1999; 80: 1372–1382.
Matjacic Z, Bajd T . Arm-free paraplegic standing—part II: experimental results. IEEE Trans Rehab Eng 1998; 6: 139–150.
Jaime RP, Matjacic Z, Hunt KJ . Paraplegic standing supported by FES-controlled ankle stiffness. IEEE Trans Rehab Eng 2002; 10: 239–248.
Dallo JG, Reichert BV, Valladão Júnior JB, Silva C, Luca BA, Levy BD et al. Differential astroglial responses in the spinal cord of rats submitted to a sciatic nerve double crush treated with local injection of cultured Schwann cell suspension or lesioned spinal cord extract: implications on cell therapy for nerve repair. Acta Cir Bras 2007; 22: 485–494.
Guttman L . The re-orientation of posture and locomotion in the spinal man. Roc R Soc Med 1968; 61: 47–58.
Potten YJM, Seelen HAM, Drukker J, Reulens JPH, Drost MR . Postural muscle responses in the spinal cord injured persons during forward reaching. Ergonomics 1999; 42: 1200–1215.
Seelen HAM, Potten YJM, Drukker J, Reulens JPH . Development of new muscle synergies in postural control in spinal cord injured subjects. J Electromyogr Kinesiol 1998; 8: 23–34.
Betz R, Boden B, Triolo RJ, Mesgarzadeh M, Gardner E, Fife R . Effects of functional electrical stimulation on the joints of adolescents with spinal cord injury. Paraplegia 1996; 34: 127–136.
Bogre KM, Triolo RJ . Effects of regular use of neuromuscular electrical stimulation on tissue health. J Rehabi Res Dev 2003; 40: 469–475.
Matjacic Z, Hunt K, Golle H, Sinkjaer T . Control of posture with FES systems. Med Eng Phys 2003; 25: 51–62.
Maynard Jr FM, Brackem MB, Creasey G, Ditunno Jr JF, Donovan WH, Ducker TB et al. International standards for neurological and functional classification on spinal cord injury patients (revised). Spinal Cord 1997; 35: 266–274.
Jackson RP, Peterson MD, McMannus AC, Hales C . Compensatory spinopelvic balance over the hip axis and better reliability in measuring lordosis to the pelvic radius on standing lateral radiographs of adult volunteers and patients. Spine 1998; 23: 1750–1767.
Roussouly P, Gollogly S, Noseda O, Berthonnaud E, Dimnet J . The vertical projection of the sum of the ground reactive forces of a standing patients is not the same as the C7 plumb line (A radiographic study of the sagittal alignment of 153 asymptomatic volunteers). Spine 2006; 11: E320–E325.
Schwab F, Lafage V, Boyce R, Skalli W, Farcy J-P . Gravity line analysis in adult volunteers. Spine 2006; 25: E959–E967.
Legaye J, Duval-Beaupere G, Jecquet J, Marty C . Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J 1998; 7: 99–103.
Ninomyia AF, Martins de Jesus CL, Auletta LL, Rinkus CM, Ferreira DM, Zoppi Filho A et al. Shoulders of patients with spinal cord injuries submitted to rehabilitation program—A clinical and ultrasound-based assessment. Acta Ortop Bras 2007; 15: 109–113.
Damasceno LHF, Catarin SRG, Campos AD, Defino HLA . Lumbar lordosis: a study of angle values and of vertebral bodies and intervertebral disc role. Acta Ortop Bras 2006; 14: 193–198, 2006.
van der Spek JH, Veltink PH, Hermens HJ, Koopman BFJM, Boom HBK . Static and dynamic evaluation of the influence of supplementary hip-joint stiffness on crutch-supported paraplegic stance. IEEE Trans Rehab Eng 2003; 11: 452–462.
Neto RV, Casanova MAM, Pithon KR, Cocha EWA, Cliquet Jr A . Assessment of Paraplegic Gait: angles, peak moment and six minute walking test. 12th Annual International Functional Electrical Stimulation Society Conference—Nov. 10–14, 2007. Philadelphia, Pennsylvania.
Zhang S, Johnston L, Zhang Z, Ma Y, Hu Y, Wang J et al. Restoration of stepping-forward and ambulatory function in patients with paraplegia: rerouting of vascularized intercostals nerves to lumbar nerve roots using selected interfascicular anastomosis. Surg Technol Int 2003; 11: 244–248.
Jackson RP, Hales C . Congruent spinopelvic alignment on standing lateral radiographs of adult volunteers. Spine 2000; 25: 2805–2815.
Kobayashi T, Atsuta Y, Matsuno T, Takeda N . A longitudinal study of congruent sagittal spinal alignment in an adult cohort. Spine 2004; 29: 671–676.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Castro de Medeiros, R., Jaccard, A. & Cliquet, A. Sagittal spinal alignment in paraplegics: a new paradigm for the rehabilitation under neuromuscular electrical stimulation. Spinal Cord 48, 251–256 (2010). https://doi.org/10.1038/sc.2009.123
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2009.123