Abstract
Objective:
To create an International Urinary Tract Imaging Basic Spinal Cord Injury (SCI) Data Set within the framework of the International SCI Data Sets.
Setting:
An international working group.
Methods:
The draft of the Data Set was developed by a working group comprising members appointed by the Neurourology Committee of the International Continence Society, the European Association of Urology, the American Spinal Injury Association (ASIA), the International Spinal Cord Society (ISCoS) and a representative of the Executive Committee of the International SCI Standards and Data Sets. The final version of the Data Set was developed after review and comments by members of the Executive Committee of the International SCI Standards and Data Sets, the ISCoS Scientific Committee, ASIA Board, relevant and interested international organizations and societies (around 40), individual persons with specific expertise and the ISCoS Council. Endorsement of the Data Sets by relevant organizations and societies will be obtained. To make the Data Set uniform, each variable and each response category within each variable have been specifically defined in a way that is designed to promote the collection and reporting of comparable minimal data.
Results:
The variables included in the International Urinary Tract Imaging Basic SCI Data Set are the results obtained using the following investigations: intravenous pyelography or computer tomography urogram or ultrasound, X-ray, renography, clearance, cystogram, voiding cystogram or micturition cystourogram or videourodynamics. The complete instructions for data collection and the data sheet itself are freely available on the websites of both ISCoS (http://www.iscos.org.uk) and ASIA (http://www.asia-spinalinjury.org).
Similar content being viewed by others
Introduction
The causes of death after spinal cord injury (SCI) have significantly changed from being primarily because of diseases of the urinary tract to those of cardiovascular and respiratory complications.1, 2, 3, 4 The reasons for this change have been through significant improvements in the diagnosis of urological problems, particularly the use of imaging and urodynamics. This has led to more timely interventions and better management over the longer term for people with SCI.
The imaging techniques for investigating the upper and lower urinary tracts include magnetic resonance imaging, computer tomography (CT) urograms, ultrasound and X-rays. More invasive tests include intravenous pyelography, renography, clearance, micturition cystourogram and videourodynamics. Many SCI centers around the world now use these techniques, and such investigations should ideally be carried out on a regular basis and at least biennially across the lifetime of a person with an SCI.5 Collecting data from these follow-up investigations will provide an important record for each patient particularly to determine the course of treatment and management.
On account of the increasing prevalence of individuals living with SCI following a traumatic as well as non-traumatic spinal cord lesion, there is a demand for effective data collection systems to facilitate comparisons regarding diagnoses, treatments and outcomes between patients, centers and countries. Such data should be documented in the form of common International Data Sets collected on individuals with SCI. Therefore, it is increasingly important to have comparable data so that the services affecting the outcome of SCI can be assessed and compared worldwide6 to effect best practice.
The purpose of this paper is to present a standardized format of collecting and reporting the minimum of information from urinary tract imaging investigations required to conform to the purpose and vision of the International SCI Data Sets.6 The International Urinary Tract Imaging Basic SCI Data Set should then make it possible to evaluate and compare results from various published studies across the world.
Methods
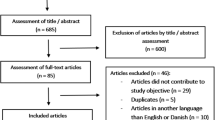
The first draft of the International Urinary Tract Imaging Basic SCI Data Set was made by a working group consisting of members appointed by the Neurourology Committee of the International Continence Society, the European Association of Urology, the American Spinal Injury Association (ASIA), the International Spinal Cord Society (ISCoS), together with a representative of the Executive Committee of the International SCI Standards and Data Sets.
The process for developing this version of the International Urodynamic Basic SCI Data Set followed the steps given below:
-
1
The working group of the International Urodynamic Basic SCI Data Set finalized the first draft during a three-day meeting in Copenhagen in November 2005. This was further elaborated by frequent e-mail contact between the group members.
-
2
The data set has been tried out in practice to test its usability, and was found easy to fill in with data available in medical records.
-
3
The data set has been reviewed by members of the Executive Committee of the International SCI Standards and Data Sets.
-
4
The comments from the Committee members were discussed in the working group and appropriate responses were made to the Data Set.
-
5
Members of the ISCoS Scientific Committee and ASIA Board were also asked to review the data set.
-
6
The comments from the Committee and Board members were discussed in the working group and a response was made, and further adjustments of the data set were performed.
-
7
Relevant and interested scientific and professional international organizations and societies (around 40) and individuals who were interested were also invited to review the data set. In addition, the Data Set was posted on the ISCoS and ASIA websites for over 2 months to allow comments and suggestions.
-
8
The comments were discussed and responded to by the working group where appropriate, adjustments to the data set were made.
-
9
To conclude this part of the consultation, members of the ISCoS Scientific Committee, Council and ASIA Board received the data set for final review and approval.
-
10
Endorsement of the Data Set will be obtained by the relevant international organizations and Societies.
Results
The complete data set is included in the Appendix. The complete data syllabus and data sheet are available for free at the websites of ISCoS (http://www.iscos.org.uk) and ASIA (http://www.asia-spinalinjury.org). It is to be recognized that the data in the International Urinary Tract Imaging Basic SCI Data Set are to be seen in the context of the International SCI Core Data Set,7 the International Lower Urinary Tract Function Basic SCI Data Set8 and the International Urodynamic Basic SCI Data Set.9
Date of data collection
This is the date of collection of data for a particular investigation, that is, the date for the performance of the investigation. This may be at any time after the spinal cord lesion. The date of data collection is imperative to be able to identify the relation to other data collected on the same individual. These include the time interval from the date of birth (age) and lesion (time since lesion), as well as the clinical or urodynamic variables.
Intravenous pyelography/urography or computer tomography urography or ultrasound of the urinary tract
The intravenous pyelography or urography is a radiographic investigation with intravenous contrast medium, which permits one to evaluate the entire urinary collecting and transportation system. It must include a plain film of the abdomen at the start. The CT urography is a CT investigation with intravenous contrast medium, which permits one to evaluate the entire urinary collecting and transportation system. The ultrasound investigation of the urinary tract includes kidneys, renal pelvis, ureters and urinary bladder.
Normal
Normal anatomical conditions were found; in particular, no stasis or dilatation of the upper urinary tract or stones in the kidney, ureter or urinary bladder was observed.
Stasis/dilatation in upper urinary tract
There was no stasis or dilatation in the renal pelvis (hydronephrosis) and/or ureter (hydroureteris) on the right and/or the left side.
Kidney stone
Urinary stone(s) was/were found in the renal pelvis or renal parenchyma on the right and/or the left side.
Stone in ureter
Urinary stone(s) was/were found in the ureter on the right and/or the left side.
Bladder stone
Urinary stone(s) was/were found in the urinary bladder. Stones of any kind or size qualify for this documentation.
Other findings
Findings of any specific deviations from the normal state not documented above can be stated in a text field.
X-ray of the urinary tract: kidney, ureter and bladder
This variable documents the result of the X-ray of the urinary tract.
Normal
Normal anatomical conditions were found; in particular, there were no stones in the kidney, ureter or bladder.
Kidney stone
Urinary stone(s) was/were found in the renal pelvis or renal parenchyma on the right and/or the left side.
Stone in ureter
This means urinary stone(s) was/were found in the ureter on the right and/or the left side.
Bladder stone
Urinary stone(s) was/were found in the urinary bladder. Stones of any kind or size qualify for this documentation.
Other findings
Findings of any specific deviations from the normal state not documented above can be stated in a text field.
Renography
This study documents the result of the renography performed with radioactive isotope-marked substance.
Method
The different methods of renography may give a different focus regarding picture, morphology and function. Therefore, it is important that the method used is known, that is, Technetium-99m dimercaptosuccinic acid, Technetium-99m diethylenetriamine pentaacetic acid or Technetium-99m mercaptoacetyltriglycine 3.
Normal
There was a normal uptake and excretion of the isotope. Normal functional and anatomical conditions were found; in particular, there was equal excretory function of the two kidneys with no stasis or dilatation of the upper urinary tract.
Excretory function
The combined excretory function for the two kidneys was 100%. The percentage of excretory function of each kidney needs to be documented.
Stasis/dilatation in upper urinary tract
Stasis or dilatation was found in the renal pelvis and/or ureter on the right and/or the left side.
Other findings
Findings of any specific deviations from the normal state not documented above can be stated in a text field.
Clearance
The clearance investigation documents the total glomerular filtration capacity of the kidneys. This is an investigation carried out with or without a radioactive isotope-marked substance (for example, Technetium-99m mercaptoacetyltriglycine or non-radioactive creatinine). The value is corrected for the individual's body surface area (1.73 m2). Reference intervals are adjusted for the person's age and the method used.
Cystogram
The cystogram may document anatomical pathologies in the lower urinary tract.
Normal
Normal anatomical conditions were found; in particular, there were no stones in the bladder, vesicoureteral reflux or bladder diverticulum.
Bladder stone
Urinary stone(s) was/were found in the urinary bladder. Stones of any kind qualify for this documentation.
Vesicoureteric reflux
Reflux to the ureter was observed on the right and/or the left side.
Bladder diverticulum
Diverticula of any size within the bladder or bladder neck were found.
Bladder neck at rest
The bladder neck is evaluated to be either open or closed at rest.
Other findings
Findings of any specific deviations from the normal state not documented above can be stated in a text field.
Voiding cystogram or micturition cystourogram or videourodynamics
The cystogram variable may document anatomical pathologies in the lower urinary tract.
Normal
Normal anatomical and functional conditions were found; in particular, there were no stones in the bladder, vesicoureteral reflux, bladder diverticulum or detrusor sphincter dyssynergia.
Vesicoureteric reflux
Reflux to the ureter was observed on the right and/or the left side.
Bladder neck during voiding
Normal bladder neck function is when the bladder neck opens, and is continuously relaxed to allow the bladder to be emptied at normal pressure. Closed bladder neck during voiding (dyssynergia) is when the detrusor contracts with concurrent bladder neck closure.
Striated urethral sphincter during voiding
Normal urethral function is defined as a urethra that opens, and is continuously relaxed to allow the bladder to be emptied at a normal pressure.10 Detrusor sphincter dyssynergia is defined as detrusor contraction with concurrent involuntary contraction of the urethral and/or periurethral striated muscle. Occasionally, the flow may be interrupted.10
Other findings
Findings of any specific deviations from the normal state not documented above can be stated in a text field.
Discussion
The data in this International Urinary Tract Imaging Basic SCI Data Set shall be seen in conjunction with data in the International SCI Core Data Set,7 the International Lower Urinary Tract Function Basic SCI Data Set8 and the International Urodynamic Basic SCI Data Set.9 The International SCI Core Data Set includes, among other things, information on the date of birth and injury, gender, the cause of spinal cord lesion and neurological status, whereas the International Lower Urinary Tract Function Basic SCI Data Set8 includes variables on urinary tract impairment unrelated to spinal cord lesion, awareness of the need to empty the bladder, bladder emptying, average number of voluntary bladder emptying per day during the last week, incontinence within the last three months, collecting appliances for urinary incontinence, any drugs for the urinary tract within the last year, surgical procedures on the urinary tract, and any change in urinary symptoms within the last year. The International Urodynamic Basic SCI Data Set9 includes data on bladder sensation during filling cystometry, detrusor function, compliance during filing cystometry, function during voiding, detrusor leak point pressure, maximum detrusor pressure, cystometric bladder capacity and post-void residual volume.
A spinal cord lesion may be traumatic or non-traumatic of etiology. All lesions to the spinal cord, conus medullaris and cauda equina are included in this context.
It is extremely important that data be collected in a uniform manner. For this reason, each variable and each response category within each variable have been specifically defined in a way that is designed to promote the collection and reporting of comparable minimal data.
The use of a standard format is essential for combining data from multiple investigators and locations. Various formats and coding schemes may be equally effective and could be used in individual studies or by agreement of the collaborating investigators.
Ideally, this International Urinary Tract Imaging Basic SCI Data Set will need to be continually reviewed, and wherever necessary, updated. Ideas for improvement from individual or groups are welcome and will be addressed by the corresponding author. It should be recognized that the data set presented in this paper is a Basic SCI Data Set and, as such, has been kept simple to provide condensed and easily assimilated information for follow-up consultations of people with spinal cord lesions.
The International Urinary Tract Imaging Basic SCI Data Set is the third urological Basic SCI Data Set, and together with the International Lower Urinary Tract Function Basic SCI Data Set8 and the International Urodynamic Basic SCI Data Set9 these three Basic SCI Data can be used to collect basic urological information in individuals with spinal cord lesions admitted to SCI centers.
References
DeVivo MJ, Krause JS, Lammertse DP . Recent trends in mortality and causes of death among persons with spinal cord injury. Arch Phys Med Rehabil 1999; 80: 1411–1419.
Frankel HL, Coll JR, Charlifue SW, Whiteneck GG, Gardner BP, Jamous MA et al. Long term survival in spinal cord injury: a fifty year investigation. Spinal Cord 1998; 36: 266–274.
Hartkopp A, Brønnum-Hansen H, Seidenschnur A-M, Biering-Sørensen F . Survival and cause of death after traumatic spinal cord injury. A long-term epidemiological survey from Denmark. Spinal Cord 1997; 35: 78–85.
Soden R, Walsh J, Middleton JW, Craven ML, Rutkowski SB, Yeo JD . Causes of death after spinal cord injury. Spinal Cord 2000; 38: 604–610.
Sthörer M, Castro-Diaz D, Chartier-Kastler E, Kramer G, Mattiasson A, Wyndaele JJ . Guidelines on neurogenic lower urinary tract dysfunction. Eur Assoc Urol 2006, pp 1–55.
Biering-Sørensen F, Charlifue S, DeVivo M, Noonan V, Post M, Stripling T et al. International spinal cord injury data sets. Spinal Cord 2006; 44: 530–534.
DeVivo M, Biering-Sørensen F, Charlifue S, Noonan V, Post M, Stripling T et al. International spinal cord injury core data set. Spinal Cord 2006; 44: 535–540.
Biering-Sørensen F, Craggs M, Kennelly M, Schick E, Wyndaele JJ . International lower urinary tract function basic spinal cord injury data set. Spinal Cord 2008; 46: 325–330.
Biering-Sørensen F, Craggs M, Kennelly M, Schick E, Wyndaele JJ . International urodynamic basic spinal cord injury data set. Spinal Cord 2008; 46: 513–516.
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U et al. The standardisation of terminology of lower urinary tract function: report from the standardisation sub-committee of the international continence society. Neurourol Urodynamics 2002; 21: 167–178.
Acknowledgements
Coloplast A/S, Denmark have supported the work with this Data Set with an unconditional grant. We are thankful for comments and suggestions received from Susan Charlifue, Marcalee Sipski Alexander and William Donovan. The societies that endorse the International Urinary Tract Imaging Basic SCI Data Set will be announced at the websites of ISCoS (http://www.iscos.org.uk) and ASIA (http://www.asia-spinalinjury.org).
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix

Rights and permissions
About this article
Cite this article
Biering-Sørensen, F., Craggs, M., Kennelly, M. et al. International Urinary Tract Imaging Basic Spinal Cord Injury Data Set. Spinal Cord 47, 379–383 (2009). https://doi.org/10.1038/sc.2008.149
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2008.149
Keywords
This article is cited by
-
What do X-ray images of the bladder during video urodynamics show us in patients with spinal cord injury?
Spinal Cord (2022)
-
International spinal cord injury urodynamic basic data set (version 2.0)
Spinal Cord Series and Cases (2018)
-
Electronic medical record: data collection and reporting for spinal cord injury
Spinal Cord Series and Cases (2018)
-
International Spinal Cord Injury Lower Urinary Tract Function Basic Data Set (version 2.0)
Spinal Cord Series and Cases (2018)
-
Relevance of the international spinal cord injury basic data sets to youth: an Inter-Professional review with recommendations
Spinal Cord (2017)