Abstract
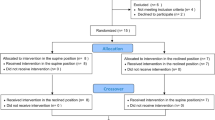
Study design:
A prospective cohort study.
Objectives:
To evaluate whether patients with cervical spinal cord injury (CSCI) are able to learn the technique of glossopharyngeal pistoning (breathing) for lung insufflation (GI) and if learned, to evaluate the effects of GI on pulmonary function and chest expansion after 8 weeks.
Setting:
Karolinska University Hospital, Stockholm, Sweden.
Methods:
Twenty-five patients with CSCI (21 men, four women) with a mean age of 46 years (21–70), from the Stockholm area, were used in this study. The participants performed 10 cycles of GI four times a week, for 8 weeks. Pulmonary function tests made before and after the GI training included vital capacity (VC), expiratory reserve volume (ERV), functional residual capacity (FRC; measured with nitrogen washout), residual volume (RV) and total lung capacity (TLC). Chest expansion was measured before and after training.
Results:
Five of the twenty-five participants had difficulty in performing GI and were excluded in further analysis. Performing a GI maneuvre increased participants' VC on average by 0.88±0.5 l. After 8 weeks of training, the participants had significantly increased their VC 0.23 l, (P<0.001), ERV 0.16 l, (P<0.01), FRC 0.86 l, (P<0.001), RV 0.70 l, (P<0.001) and TLC 0.93 l, (P<0.001). Chest expansion increased at the level of the xiphoid process by 1.2 cm (P<0.001) and at the level of the fourth costae by 0.7 cm (P<0.001).
Conclusions:
After using GI for a period of 8 weeks, the participants with CSCI who could perform GI were able to improve pulmonary function and chest expansion.
Similar content being viewed by others
Introduction
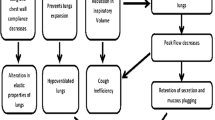
Injury of the cervical spinal cord (CSCI) between C4 and C5 can lead to severe respiratory deficiency because of partial or total paralysis of respiratory muscles. Diminished tidal volumes and cough flows are typical, whereas vital capacity (VC) and compliance in the lungs and thorax may decrease.1, 2 Cough function may also be adversely affected, thus secretions may be retained and impaired gas exchange may develop.1, 2 Pulmonary complications are one of the most common causes of mortality and morbidity in these patients.3
To improve cough flow it is important to increase the MIC (maximum insufflation capacity); this is the maximal volume of air that can be held in the lungs with the glottis closed.4 This can be achieved with mechanical insufflation–exsufflation, by air stacking with a manual resuscitator, or with glossopharyngeal breathing (GPB).5 GPB is the use of glossopharyngeal muscles to piston (gulp) small amounts of air into the lungs, assisting ventilation. It can be used for patients with decreased VC to increase VC, to cough more effectively, increase speech volume, maintain pulmonary compliance and prevent atelectases.6, 7 Glossopharyngeal insufflation volume (GIV) is the lung volume over the inspiratory capacity added by glossopharyngeal pistoning for lung insufflation (GI). VCGI is the VC supplemented by GI, thus VCGI=VC+GIV.8, 9
If VC can be increased, both in the short and long term, it would be beneficial for the patient, enhancing the capability to clear airway secretions and reducing the risk of pneumonia.
The aim of this study was to evaluate whether patients with CSCI can learn the GI technique (and thus GPB) and whether learned to evaluate the effects of GI on pulmonary function and chest expansion after 8 weeks.
Materials and methods
Participants
Participants were recruited from the Spinals clinic at the Karolinska University Hospital in Stockholm. The inclusion criteria were as follows: spinal cord injury with a lesion between the level of C4 and C8, time between injury and inclusion at least 1 year, an American Spinal Injury Association10 impairment classification of A, B or C, ventilatory independent and 16–70 years of age.
Exclusion criteria were chronic obstructive pulmonary disease, symptomatic infection characterized by fever, unable to perform GI because of the presence of severe conditions, trauma or cognitive dysfunction.
Table 1 shows the baseline characteristics of the 25 participants. Table 2 shows the injury level and the American Spinal Injury Association classification. The study was approved by the local Research Ethics Committee at the Karolinska Institutet. All subjects gave their written informed consent to participate.
Procedure
Each participant received individual instruction on the GI technique from the same physiotherapist. They watched an instructional video, received written information and practiced the technique with the instructor.
The participants first carried out a maximal inhalation and then performed GI using as many gulps of air as possible without discomfort. Finally, the air was passively expelled. All participants gulped through the mouth. All participants tried to perform the technique both with and without a nasal clip to avoid air leakage past the soft palate. All carried out a short warm-up with stretching exercises for the chest, then performed 10 repetitions of GI in a sitting or supine position. They performed GI at least four times a week for 8 weeks.
All measurements were performed by the same researcher before and after 8 weeks of GI sessions. Some intermediate measurements were taken during ‘follow-ups’ performed at least three times during the 8-week period. Measurements were performed before, during and after a training session (see below).
Static and dynamic spirometry, including measurements of VC, expiratory reserve volume (ERV), functional residual capacity (FRC), residual volume (RV), total lung capacity (TLC), diffusion capacity (DLCO) and alveolar ventilation were carried out using a Vmax 229 spirometer (SensorMedics, Yorba Linda, CA, USA) in accordance with current American Thoracic Society standard.11 Reference values from Quanjer et al.12 were used for comparison.
A portable infrared interruption flow sensor (Micro Loop; Cardinal Health, Basingstoke, UK) was used for ‘follow-up’ measurements of VCGI during the 8-week training period, along with measurements of VC before and after a session, enabling the calculation of GIV according to VCGI=VC+GIV. Peak cough flows (PCFs) were measured by coughing into a tight-fitting full-face mask (Laerdal Medical AB, Halmstad, Sweden) connected to the Micro Loop.
Mouth pressure was measured using a mouth pressure meter (Precision Medical Ltd, Kent, UK). To measure the maximum expiratory pressure (MEP), participants performed a maximum expiratory effort after a maximum inspiration. The maximum inspiratory pressure (MIP) was measured by exerting the maximum inspiratory effort after a maximum expiration. The value for MEP and MIP was taken as the highest value after three or more attempts.13
Chest expansion was measured at the level of the xiphoid process and at the fourth costae using a tape measure. The participants were instructed to perform a maximal exhalation (to RV) followed by an inhalation to TLC. Chest expansion was calculated as the difference between circumferences at RV and TLC.9 Chest expansion was also measured after gulping to TLCGI.
The number of pistoning gulps in each cycle and number of cycles were recorded in a training diary, along with any remarks on the training. The participants graded their perceived tension in the chest on the Borg CR-10 scale9 while performing GI during the training sessions. The participants were also asked to grade their ability to cough and their ability to clear secretion before and after the training period. They were asked: ‘How is your cough function affected?’ and ‘How is your ability to eliminate secretion affected?’ The answers were also rated on the Borg CR-10 scale.9
Statistical analysis
Descriptive statistics are presented as mean±1 s.d. and/or median and range. Any differences between results at baseline and after 8 weeks were assessed using Student's paired t-test. Ratings on the Borg CR-10 scale were assessed with the Wilcoxon signed-rank test. For the relationship between PCF with GI, GIV and GIV,2 a multiple regression analysis were used. A statistical significance was set at P<0.05. STATISTICA (7.0, Stat Soft Inc., Tulsa, OK, USA) was used for the analysis.
Results
Five of the participants could not exceed their VC when trying to perform GI; therefore, they were excluded from further analysis.
It was found that VC (P<0.001), ERV (P<0.01), FRC (P<0.0001), RV (P<0.001) and TLC (P<0.0001) all increased significantly after the training period (Figure 1). Mean GIV above VC was 0.88±0.5 l (an increase of 28%). PCF changed using GI from 395±83 l min−1 to 424±101 l min−1, (P=0.057). There was a significant multiple regression between PCF with GI, GIV and GIV,2 P<0.05, adjusted R2=0.39 and multiple R=0.68. This is showed with a polynomial of second degree, (Figure 2). DLCO did not change (7.26±1.51 mmol kPa−1 min−1), but alveolar ventilation increased significantly from 5.29±1.2 l to 5.47±1.2 l (P<0.05). Neither MIP nor MEP changed.
Pulmonary function parameters before (b) and after (a) 8 weeks, VC, vital capacity; ERV, expiratory reserve volume; FRC, functional residual capacity; TLC, total lung capacity; RV, residual volume. There were significant increases in all parameters; VC, P<0.001; ERV, P<0.01; FRC, P<0.001; RV, P<0.001; TLC, P<0.001.
After training, chest expansion increased significantly during maximal inhalation from RV to TLC and also on gulping to TLCGI; at the level of the xiphoid process, values increased from 3.1±1.2 cm to 4.3±1.3 cm (P<0.001) and up to 6.4±1.7 cm (P<0.001), respectively, and at the level of the fourth costae, from 3.6±1.1 cm to 4.3±1.3 cm (P<0.001) and up to 5.8±1.3 cm (P<0.001), respectively.
Some participants learned the GI technique immediately, whereas others took up to 3 weeks. Six participants used the nasal clip while training; four used it occasionally. Training compliance (self-reported) was 87%. The participants performed a mean of 10 GI cycles per training session, with each cycle consisting of an average of 14 gulps. The participants graded their perceived tension on the Borg CR-10 scale during GI, giving a median of 4 (range: 2–10). Participants occasionally reported that during, or shortly after performing GI, temporary symptoms such as dizziness (90%), local paresthesia (35%) and tension in the chest (25%) occurred. Three participants reported episodes of syncope during GI and two reported that they were close to syncope.
The participants significantly improved their rating of the two questions concerning cough function and ability to clear secretions. In answer to the former, the average reply moved from median 7 (range: 1.5–10; strongly affected) to 3.5 (range: 2–10; P<0.01; moderately affected), and the latter question's reply changed from median 7 (range: 0–10; strongly affected) to 4 (range: 1–9; P<0.01; moderately affected).
Discussion
The main findings of this study were that 20 of the 25 participants were able to adopt the GI technique and they increased most pulmonary function parameters significantly after the 8-week period. Participants were able to insufflate an additional 28% of their VC by GI, increasing chest expansion while doing so. Chest expansion without GI was also increased afterwards.
Chest expansion increased both during GI and after the training, which supports the increase in the pulmonary function parameters. GI will add a substantial volume of gas to the lungs; although some gas (up to 10%) may be compressed14 and some will enter the thorax where there is reduced blood volume, the major effect of the added gas is an expansion of the chest.8, 9 This chest expansion, beyond ‘normal’ TLC, results in a stretching effect of the respiratory system; this effect has been studied in healthy subjects8, 9 who increased their ability to expand their chest and VC after 5–6 weeks of training using the GI maneuvre. A study by Huldtgren et al.,15 in patients with CSCI, has shown that it is possible to maintain or restore optimal mobility of the chest and improve cough function using a manual resuscitator to reach the MIC.
The parameters VC, ERV, FRC and TLC increased significantly and thus participants were able to inhale and exhale more air. This is obviously of benefit, as patients with CSCI are characterized by a decrease in these parameters and an increase in RV; the treatment goal is to normalize all of these.1
In a study by Rutchik et al.,16 patients with CSCI participated in an 8-week resistive inspiratory muscle training program. They had similar increases after training in FVC, VC, TLC and FRC and also in MIP. However, in this study, MIP and MEP did not change. This was expected, as the training was aimed to stretch the chest wall alone. MEP and MIP tests were included in this study to control the participants' respiratory muscle strength. The increased RV in this study also supports the notion that we did not train the expiratory muscles.
We believe that the increases in pulmonary function seen in this study were because of increased chest wall compliance (not pulmonary compliance), thus increased FRC, and the ability to inhale a larger VC with unchanged respiratory muscle strength. To further elucidate the relative contribution of chest wall and lung tissue with compliance would require measurements of transpulmonary pressure.14
Studies have shown that the PCF increases more with GI than with other maximum inspiratory techniques.4 Kang and Bach4 also showed that VC and MIC correlated significantly with PCF, strengthening the results of the multiple regression (Figure 2) in our study. The participants had PEF and PCF values over 270 l min−1, which is enough for an effective cough, according to Bach and Saporito.17
Some of the participants reported temporary symptoms of faintness, and three went on to faint. Such results have been reported earlier,8, 18, 19 and considered to depend on a reduction in preload as a result of the increased intrathoracic pressure when the participants perform GI.14, 18 Collier et al.18 showed in a different group of patients, post-polio, that the arterial blood pressure fell slightly when they performed moderate GPB; no studies has yet been performed on patients with spinal cord injuries regarding arterial and esophageal pressure during GPB and GI. When a participant was asked to perform a maximal GPB (that is, similar to our GI maneuvers), arterial blood pressure fell to an extent where pulse pressure disappeared,18 corresponding to the increases in intrathoracic pressure. This finding was confirmed in healthy (diver) subjects studied by Novalija et al.19 as well as an increase in heart rate, which is a normal physiological response to a decrease in venous return.19 These divers could modify their GIV to avoid syncope, and we believe that most patients and healthy subjects may control their GIV to get the benefits by avoiding syncope. For some patients, it may be of value to perform this technique supine. Special consideration may be needed in patients with CSCI as they may have autonomic dysreflexia, as shown in some patients with complete lesion in Th6 or higher.20 They may have less ability to regulate peripheral resistance to maintain blood pressure and also heart rate.20 We did not measure arterial blood pressure or esophageal pressure during GI in this study, and we did not experience any reactions in our group that had not been described in earlier studies. Thus, we suggest that the instructor of GI should be well educated and aware of this possibility, and how to cope with such situations, as such a participant may be prone to syncope.
The participants notably improved the rating of their ability to cough and clear secretions after the GI intervention. These results might be because of the fact that once having learned the technique, they were able to use GI, as they felt necessary, increasing their lung volume and thus achieving a more effective cough and clearing secretions more effectively.
A limitation of the study was that the optimal study design might have been a randomized controlled study, but the participants were their own controls in this study. It was not expected that other factors should affect the physiological variables. A study on training effects of GI by Nygren-Bonnier et al.9 showed that there were no changes on VC in the control group, although they were controlled with the spirometer, once a week.
Another limitation was that the blood pressure, heart rate and oxygen saturation were only measured before and after the training period. In further studies, it would be interesting to measure during GI.
Conclusions
A total of 20 of the 25 study participants learned GI, and over 8 weeks they were able to improve their pulmonary function and chest expansion.
The GI technique can be difficult to learn, but once learned it is easy to perform.
Considering the symptoms and also the episodes of fainting, the respiratory therapist must be well educated. However, this method, if learned properly in a clinical setting by an educated instructor, should not entail any major risk.
References
Fugl-Meyer AR, Grimby G . Ventilatory function in tetraplegic patients. Scand J Rehabil Med 1971; 3: 151–160.
Goldman JM, Williams SJ, Denison DM . The rib cage and abdominal components of respiratory system compliance in tetraplegic patients. Eur Respir J 1988; 1: 242–247.
DeVivo MJ, Black KJ, Stover SL . Causes of death during the first 12 years after spinal cord injury. Arch Phys Med Rehabil 1993; 74: 248–254.
Kang SW, Bach JR . Maximum insufflation capacity: vital capacity and cough flows in neuromuscular disease. Am J Phys Med Rehabil 2000; 79: 222–227.
Homnick DN . Mechanical insufflation-exsufflation for airway mucus clearance. Respir Care 2007; 52: 1296–1305; discussion 1306–1307.
Dail CW . ‘Glossopharyngeal breathing’ by paralyzed patients; a preliminary report. Calif Med 1951; 75: 217–218.
Metcalf VA . Vital capacity and glossopharyngeal breathing in traumatic quadriplegia. Phys Ther 1966; 46: 835–838.
Nygren-Bonnier M, Gullstrand L, Klefbeck B, Lindholm P . Effects of glossopharyngeal pistoning for lung insufflation in elite swimmers. Med Sci Sports Exerc 2007; 39: 836–841.
Nygren-Bonnier M, Lindholm P, Markstrom A, Skedinger M, Mattsson E, Klefbeck B . Effects of glossopharyngeal pistoning for lung insufflation on vital capacity in healthy women. Am J Phys Med Rehabil 2007; 86: 290–294.
El Masry WS, Tsubo M, Katoh S, El Miligui YH, Khan A . Validation of the American Spinal Injury Association (ASIA) motor score and the National Acute Spinal Cord Injury Study (NASCIS) motor score. Spine 1996; 21: 614–619.
Standardization of Spirometry, 1994 Update. American Thoracic Society. Am J Respir Crit Care Med 1995; 152: 1107–1136.
Quanjer PH, Tammeling GJ, Cotes JE, Pedersen OF, Peslin R, Yernault JC . Lung volumes and forced ventilatory flows. Report Working Party Standardization of Lung Function Tests, European Community for Steel and Coal. Official Statement of the European Respiratory Society. Eur Respir J Suppl 1993; 16: 5–40.
Black LF, Hyatt RE . Maximal respiratory pressures: normal values and relationship to age and sex. Am Rev Respir Dis 1969; 99: 696–702.
Loring SH, O'Donnell CR, Butler JP, Lindholm P, Jacobson F, Ferrigno M . Transpulmonary pressures and lung mechanics with glossopharyngeal insufflation and exsufflation beyond normal lung volumes in competitive breath-hold divers. J Appl Physiol 2007; 102: 841–846.
Huldtgren AC, Fugl-Meyer AR, Jonasson E, Bake B . Ventilatory dysfunction and respiratory rehabilitation in post-traumatic quadriplegia. Eur J Respir Dis 1980; 61: 347–356.
Rutchik A, Weissman AR, Almenoff PL, Spungen AM, Bauman WA, Grimm DR . Resistive inspiratory muscle training in subjects with chronic cervical spinal cord injury. Arch Phys Med Rehabil 1998; 79: 293–297.
Bach JR, Saporito LR . Criteria for extubation and tracheostomy tube removal for patients with ventilatory failure. A different approach to weaning. Chest 1996; 110: 1566–1571.
Collier CR, Dail CW, Affeldt JE . Mechanics of glossopharyngeal breathing. J Appl Physiol 1956; 8: 580–584.
Novalija J, Lindholm P, Loring SH, Diaz E, Fox JA, Ferrigno M . Cardiovascular aspects of glossopharyngeal insufflation and exsufflation. Undersea Hyperb Med 2007; 34: 415–423.
Stjernberg L, Blumberg H, Wallin BG . Sympathetic activity in man after spinal cord injury. Outflow to muscle below the lesion. Brain 1986; 109 (Pt 4): 695–715.
Acknowledgements
We thank all the participants in the study. This study was supported by the Swedish Association of Survivors of Traffic Accidents and Polio, the Swedish Association of Persons with Neurological Disabilities, The Swedish Society of Medicine and the Health Care Sciences Postgraduate School.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nygren-Bonnier, M., Wahman, K., Lindholm, P. et al. Glossopharyngeal pistoning for lung insufflation in patients with cervical spinal cord injury. Spinal Cord 47, 418–422 (2009). https://doi.org/10.1038/sc.2008.138
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2008.138
Keywords
This article is cited by
-
Effects of glossopharyngeal insufflation on pulmonary function in cervical cord injury patients
Spinal Cord Series and Cases (2021)
-
The immediate effects of breathing with oscillated inspiratory and expiratory airflows on secretion clearance in intubated patients with cervical spinal cord injury
Spinal Cord (2019)
-
Ventilatory function in breath-hold divers: effect of glossopharyngeal insufflation
European Journal of Applied Physiology (2010)