Abstract
Study design:
Cross-sectional, observational study.
Objective:
Estimate prevalence of inadequate dietary intakes in community-dwelling men and women with chronic spinal cord injury (SCI).
Setting:
Ontario, Canada.
Methods:
In-home interviewer administered multiple-pass 24-h recalls were collected at baseline (n=77) and at 6 months (n=68). Dietary intake (adjusted to remove intra-individual variation) was compared with the dietary reference intakes (DRIs), specifically the estimated average requirement, adequate intake (AI) and acceptable macronutrient distribution ranges (AMDR).
Results:
Macronutrient intakes, as percentages of daily energy, for men (16% protein, 52% carbohydrate, 30% fat) and women (17% protein, 53% carbohydrate, 28% fat) were within the AMDR. Despite this, inadequate intakes for men (n=63) and women (n=14) were determined for vitamin A (92 and 57%), magnesium (89 and 71%), folate (75 and 79%), zinc (71 and 29%), vitamin C (52 and 14%), thiamine (22 and 14%), vitamin B12 (6 and 29%), riboflavin (5% men) and vitamin B6 (24% men). Mean usual intakes of fiber, vitamin D, calcium and potassium fell below the AI for men and women. In all, 53% of participants consumed a micronutrient supplement in the previous 24 h at baseline and at 6 months—specifically, calcium (29, 19%), multivitamin (26, 25%), vitamin D (22, 12%) and vitamin C (9, 6%).
Conclusion:
Our results show numerous nutrient inadequacies, relative to the DRIs, for men and women with SCI. This study has important implications for clinical dietetic practice in the SCI population.
Sponsorship:
Canadian Institutes of Health Research.
Similar content being viewed by others
Introduction
Approximately 50 000 Canadians currently live with chronic spinal cord injury (SCI).1 Although improvements in medical management of traumatic SCI have resulted in increased survival and lifespan, cardiovascular diseases have become one of the leading causes of death in people living with SCI.2 In addition, the prevalence of obesity,3, 4 hyperlipidemia, hypertension, diabetes mellitus and hyperinsulinemia5 is greater in the SCI vs able-bodied population. Also, early persistent bone loss that occurs in limbs below the injury is known to lead to fractures.6, 7 Despite our knowledge of the increased risk of these chronic diseases and conditions in this population, and that many of these conditions may be managed or prevented by nutrition, little is known about the dietary intake or adequacy among people with SCI.
The prevalence of inadequate intakes and the risk of chronic disease development for a particular group can be estimated by comparing 24-h recall data (adjusted to remove intra-individual variation) with the dietary reference intakes (DRIs).8 Three SCI studies4, 9, 10 have reported intakes of selected nutrients, but they did not assess intake adequacy, making it difficult to interpret the findings, and only two SCI studies have reported intake adequacy. Levine et al.11 compared the dietary data of 33 men with paraplegia or tetraplegia with the recommended daily allowances (no longer recognized as an acceptable cut-point as it overestimates the requirements of individuals within a population8), and a recent study by Tomey et al.12 compared macronutrients and a few selected micronutrients consumed by 95 men with paraplegia with the DRIs. Although both found a number of dietary inadequacies, the findings are limited by the small sizes of the samples that excluded women and by the outdated definitions of dietary adequacy.
With these limitations in mind, the objective of this study was to assess dietary intake adequacy, by comparing dietary intakes with the DRIs, in a representative sample of community-dwelling men and women with chronic SCI.
Materials and methods
Participants
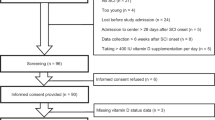
Participants were enrolled in the Study of Health and Activity in People with Spinal Cord Injury (SHAPE SCI), a multicenter study of health and activity, in over 700 individuals with SCI and for which complete methods are described elsewhere.13 Participants were residents of Ontario, Canada, ⩾18 years old, used assistance (wheelchair, walker, braces, cane) for their primary mode of mobility, were proficient enough in English to understand the interview questions and acquired SCI by trauma at least 12 months before enrolment. Participants were excluded if they self-reported cognitive or memory impairment. The data reported herein were collected on a subset of SHAPE SCI participants living within a 200 km radius of McMaster University (Hamilton, Ontario, Canada).
This study was approved by the Research Ethics Boards at McMaster University and the University of Guelph (Guelph, Ontario, Canada). Participants provided informed consent before data collection.
Methods
Data were collected within the participants’ home at baseline and at 6 months by a kinesiologist trained in phlebotomy and a research assistant. Demographic information, including sex, age, ethnicity, location and completeness of injury, and brief personal and family health histories were collected using a structured questionnaire. Each anthropometric measure was performed twice and averaged; if measures differed by >5%, a third measure was completed and the two closest measures were averaged. Participants were weighed in light clothing without shoes, using a digital wheelchair scale (Health O Meter 2450KL, Brooklyn, NY, USA). Two measures were taken, one of the participant and the wheelchair, and the other of the empty wheelchair; the participant's weight was calculated as the difference between the averages of both the measures. Length was measured from the bottom of the right heel to the crown of the head while the participant was lying supine on a spine board (National Lifesaving Society item EQ-10, Edmonton, AB, Canada), with feet in dorsal flexion, trunk straight, and head in Frankfurt plane. For the participants with contractures, length was measured and marked on their right side from the bottom of the heel to the knee, knee to hip, and hip to crown.
Twenty-four hour dietary recalls were collected at baseline and at 6 months using the multiple-pass method.14 During the first pass, a complete list of all the foods and beverages consumed during the previous 24 h was recorded, followed by detailed descriptions of cooking methods, brand names, time and location of all foods and beverages consumed. On the third pass, participants were prompted to estimate the amounts of all the foods and beverages consumed; graduated and plastic food models were introduced to help estimate portion sizes. Finally, the 24-h recall was read back to the participant to ensure that all items were recorded correctly, and the participant was asked whether the recall represented a typical day. Participants were asked to report any supplements consumed on the previous day.
Data analysis
Dietary data were entered into the Food Processor SQL Nutrition Analysis Software, Version 10.1.1 (ESHA Research, Salem, OR, USA), updated with the 2007 Canadian Nutrient File,15 USDA Standard Reference database,16 selected items from the Continuing Survey of Food Intake of Individuals (CSFII) survey database17 and manufacturers’ and fast food company data.
Before comparing the group intake data with the DRIs, within-individual variation must be removed from the actual intake distribution to obtain an estimate of the usual group intake. This procedure reduces the error when estimating the proportion of the population at risk of inadequate dietary intakes. Within-individual variation was removed following statistical methods developed by the National Research Council.18
The mean usual intake of macronutrients (as a percentage of energy), including carbohydrate, fat and protein, was compared with the acceptable macronutrient distribution ranges (AMDR). Inadequacy was determined as the proportion of the group with usual intakes above or below the AMDR as both indicate inadequate consumption and a potential risk of chronic disease.8 Micronutrient intakes were compared with the estimated average requirement (EAR); if no EAR had been established, micronutrients were compared with the adequate intake (AI). Micronutrient inadequacies were determined using the EAR cut-point method, in which the percentage of the population with usual intakes below the EAR estimates the prevalence of inadequacy.8 For nutrients with an AI, the median usual intake that meets or exceeds the AI indicates a low prevalence of inadequacy; if the median usual intake falls below the AI, no assessment of adequacy can be inferred.8
All statistical analyses were completed using SPSS Version 15.0. Descriptive statistics are presented as means, standard deviations and medians. A P-value ⩽0.05 indicated statistical significance. Independent sample t-tests were conducted to determine significant differences in the actual intake for the level of lesion (paraplegia vs tetraplegia) and completeness (complete vs incomplete injury).
We certify that all applicable institutional and governmental regulations regarding the ethical use of human volunteers were followed during the course of this study.
Results
Baseline background characteristics, including age (years), length (m), weight (kg), body mass index (BMI) (kg/m2) and duration (years); level of lesion; and completeness of injury are presented in Table 1.
Twenty-four hour recalls were completed by 77 participants at baseline and by 68 participants at 6 months. We obtained duplicate 24-h recalls for 90% of men and 79% of women. The mean usual energy intake (±s.d.) was 2096±420 kcal d−1 (52% carbohydrate, 16% protein, 30% fat) for men and 1711±152 kcal d−1 (53% carbohydrate, 17% protein, 28% fat) for women (Figure 1). In all, 9.5% of men and 7.1% of women consumed inadequate carbohydrate intake, and 7.1% of women consumed inadequate fat intake.
The median intakes for nutrients with an AI are presented in Table 2. For both men and women of all selected age groups, the median usual intakes of fiber, vitamin D, calcium and potassium fell below the AI, whereas sodium intakes met or exceeded the AI.
Nutrient inadequacies, expressed as the proportion of our population with usual intakes below the EAR, are shown in Figure 2. Nutrient intakes that met or exceeded the EAR included protein (g), carbohydrate (g), niacin (mg), phosphorus (mg) and iron (mg) for men and women, and riboflavin (mg) and vitamin B6 (mg) for women.
Nutritional supplement consumption was reported by 53% of the total population at both baseline and 6 months. Of particular interest were the micronutrient supplements; at each visit, respectively, multivitamins were consumed by 26 and 25%, calcium by 29 and 19%, vitamin D by 22 and 12% and vitamin C by 9 and 6%.
Sub-group analyses showed no significant differences in the actual intake of nutrients between individuals with paraplegia (n=38) vs tetraplegia (n=39). Individuals with a complete injury (n=28) consumed significantly more calcium (947±449 mg) than those with an incomplete injury (n=48, 758±348 mg, P<0.05); no other dietary differences were found by completeness of lesion. In the group as a whole, there were no significant differences in the actual intakes of energy or macronutrients between baseline (n=77) and 6 months (n=68).
Discussion
This is the first study to compare the usual dietary intakes with the nationally accepted DRIs in a representative sample of community-dwelling individuals with chronic SCI. The most important findings were that our participants consumed a diet apparently adequate in energy and macronutrients, but inadequate in several micronutrients, including vitamin A, magnesium, folate, zinc, vitamin C, thiamine, vitamin B12, riboflavin and vitamin B6. Median intakes of a further four nutrients (fiber, calcium, vitamin D and potassium) were below the AI.
The mean usual intake of energy (±s.d.) was 2096±420 kcal for men and 1711±152 kcal for women. Often, energy intake adequacy of a group is assessed as the proportion of the group with a BMI below, within or above the normal range (18.5–25 kg/m2), reflecting inadequate, adequate and excessive energy intakes,8 respectively. However, BMI underestimates overweight and obesity in individuals with SCI,3, 4 and therefore this approach risks overestimating the proportion of people with adequate energy intakes. The alternative method is to calculate the estimated energy requirement (EER) of that group;8 however, the equations are intended for healthy able-bodied individuals and likely overestimate the energy needs of people with SCI. Nonetheless, energy intakes of our participants were reasonably consistent with the EER (men: 2462 kcal d−1; women: 1945 kcal d−1) and mean BMI was within the overweight category (men: 26±5 kg/m2; women: 26±7 kg/m2). These findings indicate apparently adequate energy intakes, especially given that we cannot discount the possibility of under-reporting of energy intakes. Although we took steps to avoid this, under-reporting is commonly seen in dietary literature.8
Macronutrient intakes were within the AMDR, with only a few participants falling above or below. Consistent with our findings, Edwards et al.4 reported intakes of 51% carbohydrate, 15% protein and 34% fat of total energy (2079 kcal d−1) in their study of 15 men and women with SCI. Tomey et al.12 reported intakes of 49% carbohydrate, 14.5% protein and 36% of total energy (2370 kcal d−1) in their study of 95 men with paraplegia. We conclude from these combined findings that people with chronic SCI seem to consume an adequate balance of macronutrients.
Despite balanced macronutrient consumption, we identified a number of micronutrient inadequacies, including vitamin A, magnesium, folate, zinc, vitamin C, thiamine, vitamin B12, riboflavin and vitamin B6 (the latter two in men only). In addition, the mean usual intakes of fiber, calcium, vitamin D and potassium were below the AI for men and women. Tomey et al.12 used the EAR cut-point method and median intakes below 67% of the AI as a means to determine the inadequacies for vitamin C (∼25%), folate (∼30%), fiber (∼88%) and calcium (∼43%) intakes. Altogether, our findings are important given the high prevalence of secondary complications in the SCI population that may increase nutrient requirements to levels above the DRIs. In addition to many other factors, inadequate intakes of magnesium, calcium and vitamin D may be of concern, as maintaining bone health is of particular interest to the SCI population, which is at a risk of severe bone mineral losses secondary to immobilization, reduced muscle function and/or weight-bearing activity.6, 7 Respiratory and urinary tract infections and pressure ulcers are also common in this population,19 all of which may increase the nutritional needs.
Just over 50% of participants reported consuming a nutritional (micronutrient or other) supplement in the previous 24 h. Our 24-h recall procedure did not address the frequency or reasons for usage, and therefore we were unable to quantify the contribution of these supplements to the overall dietary adequacy of individuals with SCI.
The AIs for fiber are based on intake levels that protect against cancers and coronary heart disease,8 which are among the five leading causes of death beyond the first year after SCI.2 In addition, there is a high prevalence of gastrointestinal complaints (for example, distension, impaction, constipation, diarrhea),20 making fiber intake particularly relevant in this population. High-fiber diets (20–30 g d−1) have been recommended for people with SCI, but these may result in increased amount and frequency of stools.20 A diet containing no less than 15 g of fiber is therefore recommended.20 The median fiber intake of our sample, although below the AI, did exceed 15 g.
Strengths and limitations
Perhaps the most important strength of our study—unique in the SCI literature—was the method of collecting dietary data. As we recognize that 24-h recalls are subject to respondent biases, memory lapses and incorrect estimation of portion sizes,14 we took many precautions to ensure the greatest degree of accuracy possible. In addition to excluding people with self-reported cognitive or memory impairment, two trained interviewers followed the Institute of Medicine standard multiple-pass protocol14 and used graduated food models to help the participants estimate portion sizes. By conducting the interview within the home, the participants were able to confirm brand names and recipes of foods consumed, further increasing the accuracy. Importantly, we obtained duplicate records on the vast majority of participants (90% men, 79% women), increasing the accuracy of usual intakes. We used a research-quality nutrient analysis program updated with the 2007 Canadian Nutrient File,15 USDA Standard Reference database,16 selected items from the CSFII survey database,17 manufacturers’ data and fast food company data. We are therefore confident that the dietary data were carefully collected and represented usual intakes. We do caution readers, however, when interpreting the adequacy of protein, carbohydrate, niacin, phosphorus and iron in this population as the DRIs are intended for healthy able-bodied persons, and meeting the recommended intakes for nutrients does not necessarily provide enough for individuals with acute or chronic disease.8
Finally, our sample characteristics mirrored the Canadian SCI population with respect to gender, age and level of injury.1 Therefore, we feel our results are generalizable to the larger Canadian SCI population.
Conclusions
This study provides preliminary evidence of dietary intake inadequacies and will act as a benchmark for identifying those aspects of dietary intake that are most in need of change, and thus for developing and measuring the effects of future dietary interventions. Our results will inform dietetic practice and researchers charged with improving the health of people with SCI. Future research should determine the biochemical and/or clinical implications of nutrient inadequacies. In addition, research on inadequacy in relation to food groups, dietary patterns and eating behaviours, and effect of supplement use on nutritional status is warranted.
References
Canadian Paraplegic Association. Spinal cord injury in Canada. Retrieved 13 May 2004, from http://canparaplegic.org/national/level2.tpl?var1=story&var2=20001027122552 2000.
DeVivo MJ, Krause JS, Lammertse DP . Recent trends in mortality and causes of death among persons with spinal cord injury. Arch Phys Med Rehabil 1999; 80: 1411–1419.
Spungen AM, Adkins RH, Stewart CA, Wang J, Pierson RN, Waters RL et al. Factors influencing body composition in persons with spinal cord injury: a cross-sectional study. J Appl Physiol 2003; 95: 2398–2407.
Edwards LA, Bugaresti JM, Buchholz AC . Visceral adipose tissue and the ratio of visceral to subcutaneous adipose tissue are greater in adults with than in those without spinal cord injury, despite matching waist circumferences. Am J Clin Nutr 2008; 87: 600–607.
Bauman WA, Kahn NN, Grimm DR, Spngen AM . Risk factors for atherogenesis and cardiovascular autonomic function in persons with spinal cord injury. Spinal Cord 1999; 37: 601–616.
Zehnder Y, Luthi M, Michel D, Knecht H, Perrelet R, Neto I et al. Long-term changes in bone metabolism, bone mineral density, quantitative ultrasound parameters, and fracture incidence after spinal cord injury: a cross-sectional observational study in 100 paraplegic men. Osteoporos Int 2004; 15: 180–189.
Ashe MC, Craven C, Krassioukov A, Eng JJ . Bone health following spinal cord injury. In: Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Aubut J, Abramson C, Hsieh JTC, Connolly S (eds). Spinal Cord Injury Rehabilitation Evidence. Vancouver, Canada, 2006, 9.1–9.18 (http://www.icord.org/scire/pdf/SCIRE_CH9.pdf).
Institute of Medicine. Dietary Reference Intakes: The Essential Guide to Nutrient Requirements. National Academy Press: Washington, DC, 2006.
Zlotolow SP, Levy E, Bauman WA . The serum lipoprotein profile in veterans with paraplegia: the relationship to nutritional factors and body mass index. J Am Paraplegia Soc 1992; 15: 158–162.
Moussavi RM, Ribas-Cardus F, Rintala DH, Rodriguez GP . Dietary and serum lipids in individuals with spinal cord injury living in the community. J Rehabil Res Dev 2001; 38: 225–233.
Levine AM, Nash MS, Green BA, Shea JD, Aronica M . An examination of dietary intakes and nutritional status of chronic healthy spinal cord injured individuals. Paraplegia 1992; 30: 880–889.
Tomey KM, Chen DM, Wang X, Braunschweig CL . Dietary intake and nutritional status of urban community-dwelling men with paraplegia. Arch Phys Med Rehabil 2005; 86: 664–671.
Martin Ginis KA, Latimer AE, Buchholz AC, Bray SR, Craven BC, Hayes KC et al. Establishing evidence-based physical activity guidelines: methods for the Study of Health and Activity in People with Spinal Cord Injury (SHAPE SCI). Spinal Cord 2008; 46: 216–221.
Institute of Medicine. Dietary Reference Intakes: Application in Dietary Assessment. National Academy Press: Washington, DC, 2001.
Canadian Nutrient File, Compilation of Canadian Food Composition Data, Nutrition Research Division and Biostatistics and Computer Application Division, Health Protection Branch, Health Canada: Canada 2007.
United States Department of Agriculture, Agricultural Research Service. USDA National Nutrient Database for Standard Reference, Release 20 (SR 20) http://www.nal.usda.gov/fnic/foodcomp Nutrient Data Laboratory USDA: Riverdale, MD, 2007.
United States Department of Agriculture, Agricultural Research Service USDA 1994–1996 Continuing Survey of Food Intakes By Individuals—1994–1996 Diet & Health Knowledge Survey—Food Code & Nutrient Database For CSFII 1994–1996 (CD Rom).
National Research Council. Nutrient Adequacy: Assessment Using Food Consumption Surveys. National Academy Press: Washington, DC, 1986.
Wolfe DL, Hsieh JTC . Rehabilitation practices and associated outcomes following spinal cord injury. In: Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Aubut J, Abramson C, Hsieh JTC, Connolly S (eds). Spinal Cord Injury Rehabilitation Evidence. Vancouver, Canada, 2006, 3.1–3.44 (http://www.icord.org/scire/pdf/SCIRE_CH3.pdf).
Consortium for Spinal Cord Medicine. Clinical Practice Guidelines: Neurogenic Bowel Management in Adults with Spinal Cord Injury. Paralyzed Veterans of America, Washington, DC, 1998.
Acknowledgements
We gratefully acknowledge the participants of SHAPE SCI and Rebecca Bassett and Iwona Chudzik for their help with data collection. In addition, we thank Amy E Latimer, PhD, Queen's University, School of Kinesiology and Health Studies, Kingston, Ontario, Canada and Keith C Hayes, PhD, Department of Physical Medicine & Rehabilitation, University of Western Ontario, London, Ontario, Canada for their feedback on early drafts of this manuscript. This study was funded by the Canadian Institutes for Health Research.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Walters, J., Buchholz, A. & Martin Ginis, K. Evidence of dietary inadequacy in adults with chronic spinal cord injury. Spinal Cord 47, 318–322 (2009). https://doi.org/10.1038/sc.2008.134
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2008.134
Keywords
This article is cited by
-
A national survey of physical activity after spinal cord injury
Scientific Reports (2022)
-
National survey of mental health and suicidal thoughts in people with spinal cord injury
Spinal Cord (2022)
-
The effects of a high-fat/high-carbohydrate meal on leukocyte populations in adults with chronic spinal cord injury
Spinal Cord Series and Cases (2021)
-
All-cause and cause-specific mortality following non-traumatic spinal cord injury: evidence from a population-based cohort study in Switzerland
Spinal Cord (2020)
-
Vitamin D, diet, and lifestyle in a chronic SCI population
Spinal Cord (2019)