Abstract
Study design:
Prospective clinical trial of consecutive tetraplegic and paraplegic cases.
Objectives:
The detection of the neurological level of paralysis by thermographic imaging.
Setting:
Spinal Cord Injury Center in Germany Halle (Saale) and Fraunhofer Institute for Mechanics of Materials in Halle (Saale).
Methods:
Twelve tetraplegic and 4 paraplegic patients (ASIA A–C) were examined by thermal imaging with a diagnosis of a temperature difference on the skin surface.
Results:
A new application of thermography for diagnostic purposes could be demonstrated, especially by the new methodical approaches to evaluate thermographic images.
Conclusion:
Thermography could prospectively be applied in the emergency diagnosis and therapy for accident victims as a supplement to existing diagnostic measures for spinal cord injury.
Similar content being viewed by others
Introduction
Modern infrared thermal imaging allows the detection of absolute surface temperatures at very high accuracy (<0.1 K). For this purpose, heat radiation of the human body is measured at a wavelength between 3.5 and 5 μm. The lateral resolution is dependent on the optical system. Modern thermographic recording systems are thereby capable of real-time recording. In summary, thermography provides a simple, non-invasive method for the detection of surface temperatures, which can be applied for medical diagnostics, particularly at intensive care units.
The first thermal camera was developed for medical purposes in 19671 and introduced in the 1970s; however, further improvements were necessary because of insufficient temperature resolution.2 Simultaneously, the first clinically supervised studies were carried out in dermatology,3 urology4 and sports medicine5 for measuring superficial circulation and temperature. Other medical applications opened up in the field of oral and facial surgery.6 Because of the continuously insufficient resolution, these examination methods had not yet become widely accepted. A new generation of thermal cameras, which were primarily developed for military and security purposes and are now applied in the field of medicine, have achieved an increasing range of applications with intraoperative indications.7, 8, 9 In the field of veterinary medicine, a study on horses showed that thermography was capable of diagnosing a paralysis of the hind legs.10 Until now, thermography has neither been applied for the detection of the level of paralysis, nor for the therapeutic evaluation of people suffering spinal cord injuries.
In this preliminary evaluation a direct correlation between the line of paralysis and the temperature difference on the skin surface could be proved to determine the level of injury (Table 2).
Materials and methods
Sixteen patients were examined with the method described below not later than 15 weeks after the onset of the paralysis. The study contained examinations of two groups of patients 12 tetraplegic patients and 4 paraplegic patients, injury levels were C4-C7 and TH6–TH12, respectively. Examinations of two healthy probands served as reference.
The age of the tetraplegic patients was 21.7±3.7 years, the interval between the onset of the paralysis and the examination was 8±2 weeks. The age of the paraplegic patients was 32.4±2.1 years, the interval between the onset of the paralysis and the thermographic examination was 12±3 weeks. The examination results are shown with the example of a tetraplegic patient subC4 (male, 25.7 years old, paralysis 7 weeks earlier), a paraplegic patient subTh5 (male, 28.5 years old, paralysis 13 weeks earlier) and a healthy test person (male, 17.2 years old). We certify that all applicable institutional and government regulations concerning the ethical use of human volunteers were followed during the course of this research.
Thermographic examinations
For the thermographic examinations, it was necessary to carry out the measurements at the highest possible reproducibility. Before the thermographic recording of the patient, the adjustment of the body temperature to the room atmosphere, as well as a constant room temperature and humidity had to be ensured. The influence of circadian changes in body temperature had also to be taken into account and integrated into the measurements.
To reach a high local resolution of the thermal images, different segments of interest were established on the patient's bodies and the images were taken in a defined order. For the positioning of the thermal camera above the patient's bed, a specific frame with two linear units was used, which also ensured a constant distance between the camera and the patient.
For the thermographic measurements a thermal camera from FLIR Systems was used. This camera detects infrared radiation at a wavelength range from 3.6 to 5 μm at a thermal resolution of 0.1 K and temperature accuracy of ±2 K. Due to the suspension of 1.4 m above the bedside, the lateral resolution for the construction in the clinic is approximately 1.6 mm.
Before taking the pictures, the camera was aligned with the frame, and internal temperature compensation was carried out. Then the bed with the patient was moved underneath the frame. The blanket and the clothes were removed and the patient remained on his or her back for 5 min with arms outstretched. During that time a build up of heat caused by clothing or blanket, disappeared and the patient adapted to the atmosphere in the room. After this adjustment the thermal images of the patient were taken. A total of 15 shots per patient were taken.
Results
Determining the line of paralysis with this kind of evaluation or representation was evidently complex. Therefore, it was preferred to evaluate the temperature distribution over different areas.
When evaluating thermal images on the basis of different areas, all temperature values of individual surface elements, which were measured within a predefined area, are shown in a frequency histogram. This method has the advantage of levelling out local changes in temperature. By fitting with a Gauss function, a sound mean value and a spread of the temperature is achieved. With the help of the histograms and the mean value, the temperature distributions of two areas can be compared with each other, to draw conclusions about varying intensities of the blood flow, for instance.
Figure 1 shows the histograms of temperature distribution in the two areas from Figure 1 (area A1 below and A2 above the line of paralysis). For this purpose, the areas were divided into surface elements (1 pixel ≈1.4 × 1.4 mm), and for each individual surface element the temperature was entered into the frequency diagram. By curve adjustment with the Gauss function, the parameters of the temperature spread (half-width of Gauss function) and the mean value of the temperature (maximum of Gauss function) were calculated. During the examination, the temperature mean value is Tm1=36.7 °C for area A1 and Tm2=38.1 °C for area A2, in Figure 1. The temperature spread TB is a measure for the variation of the temperature distribution within the evaluated area and it is for area A1 TB1=xx.x K and for A2 TB2=xx.x K. A high and narrow curve with a small spread shows an even temperature distribution.
To check the reproducibility, the described examinations were repeated with the same patient on five different days. Chart in Figure 2 shows the difference between the mean values of the temperature in the areas A1–A2. The difference of the temperature mean values was always higher than 0.5 K and can therefore be regarded as significant.
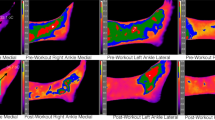
After this promising provisional result, the study was carried out with the described three groups of patients to detect the line of paralysis by means of thermography. Various skin surface areas were taken into consideration. Figures 2a–c shows the thermal images of one patient of each single group. In the paralyzed groups, the two areas A1 and A2 were selected covering the paralyzed as well as the non-paralyzed regions of the body; in the healthy group, two areas of approximately equal size were selected.
Chart in Figure 2 shows a noticeable difference of the temperature mean values between the two areas A1 and A2 (above and below the line of paralysis) with subC4 (+1.4 K) and subTh5 (−0.6 K) for the patients paralyzed. The healthy test person did not show a clear picture. The measured temperature difference varies at an interval of ±0.4 K.
In Tables 1 and 2 the results for the different groups are shown. One can see the number of patients, the number of cases with clear evidence of paralysis and the number of cases without considerable evidence. In 9 out of 12 patients suffering from tetraplegia the difference between the sensitive and the non-sensitive area could be evidently proved. Among the paraplegic group, the results were obvious proving the correct level of paralysis in all patients.
Discussion
Initially the evaluation of the thermal images was accomplished by using line profiles and histograms. Line profiles are used to show the temperature on the skin surface at a local resolution by manual setting of a line into the thermal image. With the help of this temperature profile, the basic course of the body temperature can be evaluated. The localization of temperature leaps caused by illness, which could for instance be attributed to circulatory problems, is (also) possible.
For the study at hand, we used thermography for determining a temperature difference on the skin surface with complete and incomplete (ASIA A–C)11 consecutively paralyzed patients. On the basis of clinical experience one could assume that the temperature difference of the skin surface would correlate with the sensitive level of paralysis. The diagnosis of an involvement of the spinal cord injury is not possible in all cases, especially when treating patients with an acute trauma of the spinal cord, who are unconscious because of additional brain injury or who have to be given artificial respiration due to polytrauma. There is a diagnostic window until the final examination of the neurological lesion after the completion of analgesic sedation. Neurophysiological examination methods, such as SEP, or MEP are hardly, or not at all applicable within the scope of intensive therapy because of deflection artefacts.
With the help of modern thermal cameras and a further development of recording and evaluation methods, the level of paralysis, or the neurological border between sensitive and non-sensitive body areas of paralyzed patients can be determined. In this context, it has been proven feasible to detect the temperature distribution and temperature mean values in areas that were selected with consideration of the paralysis level. To support the results of this study, it is necessary to examine an even larger group of patients.
Further measurements are planned in a future screening examination. While further refining the examination method, acutely injured intensive patients are to be examined and the question of an existing tetraplegia or paraplegia is to be answered by means of thermographic examination.
References
Bjork NA . AGA thermovision, a high speed infrared camera with instantaneous picture display. J Radiol Electrol Med Nucl 1967; 48: 30–33.
Vermeij GF . The pyroelectric vidicon camera as a medical thermograph. J Med Eng Technol 1979; 3: 5–11.
Hundhausen E, Theves B . Die Berechnung von thermisch bedingten Durchblutungsänderungen im Finger unter Benutzung thermographischer Hauttempteraturmessungen. Eur J Appl Physiol 1979; 40: 235–244.
Lewis RW, Harrison RM . Contact scrotal thermography: applications to problem of infertility. J Urol 1979; 122: 40–42.
Veghte JH, Adams WC, Bernauer EM . Temperature changes during exercise measured by thermography. Aviat Space Environ Med 1979; 50: 708–713.
Pogrel MA, Yen CK, Taylor RC . Infrared thermography in oral and maxillofacial surgery. Oral Surg Oral Med Oral Pathol 1989; 67: 126–131.
Okudera H, Kobayashi S, Toriyama T . Intraoperative regional and functional thermography during resection of cerebral arteriovenous malformation. Neurosurgery 1994; 34: 1065–1067.
Roberts WW, Dinkel TA, Schulam PG, Bonnell L, Kavoussi LR . Laparoscopic infrared imaging. Surg Endosc 1997; 11: 1221–1223.
Toda K, DiCorte CJ, McFadden PM . Assessment of thoracoscopic sympathectomy by infrared thermal imaging. Ann Thorac Surg 2000; 70: 983.
Weil M, Litzke LF, Fritsch R . Diagnostische Aussagekraft der Thermographie bei Lahmheiten des Pferdes. Tieraerztliche Praxis Ausgabe G Grosstiere Nutztiere 1998; 26: 346–354.
ASIA/IMSOP Scales of International Standards. Spinal Cord 1997; 35: 266–274.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Roehl, K., Becker, S., Fuhrmeister, C. et al. New, non-invasive thermographic examination of body surface temperature on tetraplegic and paraplegic patients, as a supplement to existing diagnostic measures. Spinal Cord 47, 492–495 (2009). https://doi.org/10.1038/sc.2008.128
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2008.128
Keywords
This article is cited by
-
Model smoke stream adsorption over cellulose acetate stick with three-dimensional temperature gradient by combining in-situ DRIFTS with infrared thermal imaging
Cellulose (2022)
-
Development of a high-resolution infrared thermographic imaging method as a diagnostic tool for acute undifferentiated limp in young children
Medical & Biological Engineering & Computing (2018)
-
Change in body surface temperature as an ancillary measurement to motor evoked potentials
Spinal Cord (2015)
-
Correlation between the changes in heat-induced digital infrared thermography imaging and body components in healthy volunteers
Toxicology and Environmental Health Sciences (2013)