Abstract
Electrochemical biosensors incorporate a recognition element and an electronic transducer for the highly sensitive detection of analytes in body fluids. Importantly, they can provide rapid readouts and they can be integrated into portable, wearable and implantable devices for point-of-care diagnostics; for example, the personal glucose meter enables at-home assessment of blood glucose levels, greatly improving the management of diabetes. In this Review, we discuss the principles of electrochemical biosensing and the design of electrochemical biosensor devices for health monitoring and disease diagnostics, with a particular focus on device integration into wearable, portable and implantable systems. Finally, we outline the key engineering challenges that need to be addressed to improve sensing accuracy, enable multiplexing and one-step processes, and integrate electrochemical biosensing devices in digital health-care pathways.
Key points
-
Electrochemical biosensors are self-contained, analytical devices, in which a biological recognition element is in direct contact with an electrochemcial transduction element to allow the sensitive and specific detection of analytes.
-
Depending on the design and sensor type, health-related and disease-related biomarkers, such as carbohydrates, proteins, nucleic acids and cells, can be rapidly analysed in different body fluids, including blood, saliva and tears.
-
Electrochemical biosensors, including amperometric, voltammetric, potentiometric, organic electrochemical transistor, photoelectrochemical and electrochemiluminescent sensors, can be integrated into wearable, portable and implantable devices to enable point-of-care diagnostics and health monitoring.
-
Commercialization and broad point-of-care applicability of integrated electrochemical biosensors will require improvements in stability, sensitivity, reproducibility, multiplexing, and digitalization and, importantly, low-cost materials and easy fabrication methods.
Similar content being viewed by others
Introduction
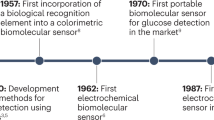
Biosensors have been widely applied in clinical, industrial, environmental and agricultural analyses since Leland Clark Jr introduced the amperometric glucose enzyme electrode in 1962 (ref. 1). According to the definition by the International Union of Pure and Applied Chemistry2, a biosensor is a self-contained, integrated, analytical device, in which a biological recognition element (biochemical receptors, including enzymes, antibodies, antigens, peptides, DNA, aptamers or living cells) is retained in direct spatial contact with a transduction element (such as electrochemical, optical and mechanical transducers). Biosensors were initially developed for point-of-care (POC) testing of biomolecular targets in the hope of extending clinical analysis from specialized laboratories to public settings, including hospitals, non-hospital nursing settings or home settings2. Although various biosensors have been developed for the sensitive and selective detection of a range of disease-related molecules, clinical translation of biosensors remains limited owing to difficulties in integrating and miniaturizing biosensors into portable devices.
Among the different biosensing platforms, electrochemical biosensors, which integrate the biorecognition element in an electrochemical transducer (for example, an electrode or field-effect transistor) are particularly suitable for device integration3,4,5 (Fig. 1a) because they can be easily miniaturized, batch fabricated and integrated with an electronic acquisition module on a single chip. In addition, electrochemical signals, such as electrical current and potential, can be collected by simple, portable and low-cost peripheral instruments with low power consumption. Moreover, the signal produced through affinity recognition of the target analyte by the biorecognition element can be amplified by physical, chemical or biological strategies, which greatly improves detection sensitivity. As such, electrochemical biosensors hold great promise for the development of POC diagnostic devices. The World Health Organization stipulates that POC biosensors should be affordable, sensitive, specific, user-friendly, rapid, robust, equipment free and deliverable to end users to enable on-site testing and diagnosis in the daily routines of individual patients and consumers. Thus, POC diagnostics are expected to play a key role in revolutionizing the diagnosis and treatment of major global diseases. For example, the electrochemical glucose meter, the most successful commercial POC biosensing device, has been widely used across the globe to help patients with diabetes.
a, Schematic representation of electrochemical biosensors based on different biochemical receptors and detection probes. b, Amperometric biosensing of metabolite targets based on an enzyme electrode, including the current–time (i–t) curve and the i signal for quantification. Voltammetric biosensing of proteins or nucleic acids using an antibody-modified or nucleic acid-modified electrode through multistep sandwich sensing, one-step binding-induced folding sensing or one-step proximity binding-based affinity sensing, including the current–potential (i–E) curve and i signal for target quantification. c, Ion-selective electrodes with three different structures, including recording of the potential (E) for target quantification. d, Two types of organic electrochemical transistor sensors prepared by immobilizing the recognition element on the channel surface or on the gate electrode (G) for sandwich immunoassays of proteins, including recording of the channel current (ichannel) for target quantification. e, Photoelectrochemistry biosensing based on a three-electrode system and a light source, including recording of the photoelectrode photocurrent (ipc) upon target recognition for quantification. f, Electrochemiluminescence biosensing of cells based on an aptamer-modified electrode through a sandwich-sensing format, including light intensity (IECL) at excited potential by a photomultiplier tube (PMT) or imaging using a camera for target quantification. g, Integration of electrochemical biosensors in portable, wearable and implantable devices. CE, counter electrode; D, drain electrode; Medox, oxidized form of mediator; Medred, reduced form of mediator; RE, reference electrode; S, source electrode; WE, working electrode.
However, the market for electrochemical biosensing devices is currently limited to the detection of some small molecules or ions (Supplementary Table 1), which can be detected directly by electrochemical signals through oxidation, reduction or affinity interactions at the electrode surface. By contrast, the detection of large biomarkers, such as proteins, nucleic acids, bacteria or cells, mainly relies on affinity recognition and, thus, requires multiple steps to produce a detectable signal. Several transduction principles may promote the integration of fully automated electrochemical biosensing devices for affinity biomarkers, including the relation of affinity recognition events with the generation and consumption of glucose6,7,8,9,10, one-step affinity-sensing mechanisms, such as binding-induced folding sensing and proximity binding-based affinity sensing11,12, and integration with automatic fluidic systems such as pump-assisted fluidics, paper-based microfluidics and polydimethylsiloxane (PDMS)-based microfluidics13,14,15. In addition, owing to the low concentration of disease markers in body fluids, in particular, in the early stages of disease (femtomolar or attomolar level), signal amplification strategies are required to increase detection sensitivity, which can be achieved by implementing nanotechnology-based and biotechnology-based strategies, such as amplification strategies based on nanotags, nanocatalysis, and nanocarriers and assembly-based and polymerase-based DNA amplification strategies16,17.
Efficient health-care management requires electrochemical biosensors to achieve minimally invasive or non-invasive continuous measurement of physiological molecules. Advances in microelectronic engineering, semiconductor precision-machining, flexible and stretchable bioelectronics and wireless communication technologies have spearheaded the integration of electrochemical biosensors in wearable and implantable devices18,19,20,21. To achieve long-term detection of molecules in different biofluids (for example, cerebrospinal fluid, interstitial fluid, sweat, saliva, tears and urine), electrochemical biosensors can also be integrated into flexible films, textiles, glasses, teeth and diapers. Furthermore, combining sensors with smartphones and other mobile devices allows continuous monitoring of dynamic physiological processes, and the integration of intelligent or digital processing modules into devices enables the connection of sensors to the Internet of Things and cloud computing for large-scale medical data mining.
In this Review, we discuss key innovations in electrochemical biosensing for preventive and personalized POC diagnostic devices. We discuss the design and integration of amperometric, voltammetric, potentiometric, organic electrochemical transistor (OECT), photoelectrochemical and electrochemiluminescent biosensors (Table 1) for disease diagnosis, health management, cell monitoring and neuroscience. In addition, we examine the fabrication, fluidic manipulation, signal amplification and readout, signal processing algorithms, and result visualization of integrated biosensors.
Electrochemical sensing of biomarkers
In electrochemical biosensors, the signal is typically triggered by electron or ion transfer on a conductive transducer through a biorecognition process. Signals can involve current (i), potential (E), impedance, conductivity, capacitance and light (I). Among these, impedimetric biosensors are theoretically favoured for POC diagnostics and device integration because they can directly detect biorecognition events by measuring the non-faradaic resistance and capacitance properties of the sensing electrode; however, their practical implementation suffers from non-specific binding of non-target compounds, which leads to low sensitivity and selectivity. In addition, although impedimetric biosensors have been greatly improved during the COVID-19 pandemic, for example, using molecular imprinting technology to fabricate virus-imprinted impedimetric biosensors for sensitive detection of whole virus particles22 or by applying a dielectrophoresis force to improve the detection sensitivity of impedimetric immunosensors fabricated on Au micro-interdigitated electrodes23, their proof-of-concept performance is often only demonstrated using artificial physiological samples instead of clinically relevant samples.
Amperometric and voltammetric biosensors
Amperometric and voltammetric biosensors are operated with a three-electrode system, which contains a biosensor as a working electrode (WE) for target recognition, a counter electrode as the current source, and a reference electrode to apply a stable potential. Current signals are generated by electrochemical reactions on the WE under an applied potential for target quantification. The difference between the two techniques is their applied potential, which is constant for amperometric measurements and variable for voltammetric detection. According to the potential change modes, the latter can be performed with various techniques, including cyclic voltammetry, differential pulse voltammetry, square wave voltammetry and anodic stripping voltammetry.
Amperometric biosensors are the most popular sensors for the detection of metabolites (for example, glucose, lactate and uric acid). In amperometric biosensors, a target-specific enzyme (for example, glucose oxidase (GOx), lactate oxidase or uricase) is immobilized on the WE to catalyze the oxidation of the target at a constant potential3; for example, glucose meters are typically constructed with amperometric biosensors that use GOx to catalyze the oxidation of glucose by a redox mediator (for example, ferricyanide, ferrocene derivative and transition-metal complexes) (Fig. 1b); alternatively, amperometric glucose sensors can rely on the enzymatic oxidation of glucose with natural oxygen to generate and detect hydrogen peroxide using a mediator such as Prussian blue24. Amperometric biosensors are simple to fabricate, and have high sensitivity and selectivity in target detection, making them suitable for wearable applications. As the concentration of metabolites in non-blood fluids is lower than that in blood (for example, the concentration of sweat glucose (10–200 μM) and tear glucose (0–2 mM) are, respectively, 100-fold and 10-fold lower than that of blood glucose (1–20 mM)), nanomaterials, such as metallic nanoparticles, carbon nanotubes and graphene, can be added to the biosensing interface to facilitate electron transfer to increase the sensitivity and decrease the detection limit25. For example, Au–Pt bimetallic nanocatalysts in combination with nanoporous hydrogels enable GOx immobilization and glucose detection with a sensitivity of 180 μA cm–2 mmol–1 and a detection limit of 0.01 mg dl−1 (0.56 μM), making such a biosensor suitable for integration with a smart contact lens for tear glucose measurement26. In addition, nanomaterials with enzymatic properties (that is, artificial nanoenzymes) can be implemented in amperometric biosensors to avoid denaturation of natural enzymes; for example, using a laser-induced graphene array, co-decorated with Cu2O and Au nanoparticles, a miniaturized, electrochemical, flexible, non-enzymatic biosensor was designed, offering stable sensing signals upon bending back-and-forth 25 times; its integration with a smartphone-based portable station for glucose monitoring has been verified with commercial blood testing devices27.
Metabolites can be detected by enzymatic recognition; by contrast, disease biomarkers, such as proteins and nucleic acids, are detected by affinity recognition, which cannot directly generate electron transfer on the biosensing surface. Thus, an additional electroactive label is needed for target sensing such as enzymes (for example, horseradish peroxidase and alkaline phosphatase), nanomaterials (for example, nanoparticles, nanotubes and quantum dots) and electroactive molecules (for example, ferrocene and methylene blue). These labels are typically detected by cyclic voltammetry, differential pulse voltammetry, square wave voltammetry and anodic stripping voltammetry, and therefore, most affinity sensors are voltammetric biosensors. Such sensors can be fabricated by immobilizing capture biomolecules (for example, antibodies, antigens, aptamers and DNA) on the WE to enable the detection of proteins or nucleic acids using a sandwich assay format (Fig. 1b). Here, sequential incubations with the target, detection molecules and electrochemical nanotags are required3,4, limiting device integration of affinity biosensors. To simplify this operation, automatic fluidic systems can be applied; for example, biosensors fabricated on screen-printed carbon electrodes can be coupled with a flow-injection system to automatically detect multiple protein biomarkers28,29,30. However, the large size and high cost of this apparatus may limit commercialization.
Microfluidics allows the manipulation of fluids in micrometre-scale channels by integrated fluidic control units such as microvalves, pumps and reactors31. Therefore, multistep liquid processing workflows can be integrated into a single chip for fully automated sample-to-answer analysis32,33. Coupling electrochemical biosensors with microfluidics enables continuous and high-throughput detection of multiple trace analytes in complex samples such as human serum and blood samples. Several electrochemical biosensing devices have been commercialized (for example, Cue Reader from Cue Health, ePlex RP2 from GenMark Diagnostics, Binx io from Binx Health) for chip-based or cartridge-based detection of SARS-CoV-2 nucleic acids, respiratory viral and bacterial organisms, and Chlamydia trachomatis based on the integration of digital microfluidics (such as electrowetting) with amperometric or voltammetric affinity biosensors (Supplementary Table 1). These products enable at-home testing of disease biomarkers but are very expensive. Alternatively, cheaper and highly sensitive electrochemical biosensing systems can be designed by combining amperometric or voltammetric biosensors with paper-based microfluidics with self-pumping ability. These systems can integrate multiplex sensing electrodes for differential pulse voltammetry or square wave voltammetry detection of protein and nucleic acid biomarkers13,15. For example, an origami paper-based aptamer and antibody biosensing chip enables simultaneous detection of C-reactive protein (CRP) and pre-albumin down to the picogram per millilitre level34. By integrating amperometric or voltammetric biosensors with PDMS-based microfluidics, which can be fabricated by high-precision micromachining technologies, including soft lithography, casting, imprinting, injection moulding and laser ablation, the automation, miniaturization and array size of devices can be improved35,36,37. For example, 16 three-electrode biosensors integrated with a PDMS chip with separate chambers and reservoirs of reagents and samples allow the high-throughput detection of three protein markers of breast cancer38.
Merging biosensors with automatic fluidic systems simplifies detection; however, device integration remains difficult owing to the requirement of pumps and reservoirs. One-step affinity sensors provide a simpler alternative; for example, a binding-induced folding electrochemical biosensor can be fabricated by site-specific modification of a redox-tagged probe DNA on the WE11. The detection of the target then relies on the binding-induced change in rigidity of the probe DNA (Fig. 1b), causing the redox tags to move close or away from the electrode surface, resulting in a respective increase or decrease of the current signal for target biosensing. Such binding-induced folding electrochemical biosensors can achieve sample-in-answer-out sensing of nucleic acids or sensing of some specific proteins using aptamer receptors; however, they suffer from low sensitivity. The signal can be amplified using DNA hybridization strategies39,40; for example, an electrochemical DNA sensor based on target-induced CRISPR–Cas12a cleaving of interfacial single-stranded DNA with methylene blue as the signal tag can detect human papillomavirus 16 (HPV16) and parvovirus B19 (PB19) down to the picomolar level41. The sensitivity of this DNA sensor can be further improved using a hairpin DNA probe42.
Proximity binding-based affinity electrochemical biosensors are particularly suited for protein biomarker detection because they can transfer a protein immunoassay to DNA detection12. In such biosensors, a pair of antibody-DNA affinity probes dually recognizes a target protein, which leads to the formation of proximity ligation products that initiate DNA assembly, causing the ‘on’ or ‘off’ state of the electroactive molecule-tagged probe DNA on the electrode surface (Fig. 1b). A wash-free and separation-free square wave voltammetry biosensor based on a proximity binding-induced ‘on’ state of methylene blue–DNA on the electrode surface allows direct detection of insulin43. By introducing uracils in the DNA sequence, this biosensor can be made reusable, enabling repeated protein quantitation within 3 min (ref. 44). The sensitivity of proximity binding-based affinity electrochemical biosensors can be further improved by DNA amplification strategies; for example, introducing an electrochemical ratiometric readout45,46, nuclease-mediated or DNAzyme-mediated cycle amplification47,48, surface programmatic chain reaction49, or DNA walker amplification50 enables the one-step detection of glycoprotein markers (for example, carcinoembryonic antigen (CEA), prostate-specific antigen (PSA) and thrombin) down to picogram per millilitre or sub-picomolar levels (Supplementary Table 2).
Potentiometric biosensors
Potentiometric biosensors are typically operated with a two-electrode system consisting of a sensing electrode and a reference electrode, allowing direct detection of targets by measuring the potential signal related to the change of surface charge upon target recognition on the sensing electrode. Typically, ion-selective electrodes made of ion-selective membranes and a liquid contact structure are used as potentiometric sensing electrodes (Fig. 1c). Glass membrane ion-selective electrodes (for example, pH electrode), solid membrane ion-selective electrodes (for example, crystalline membrane electrodes for F−, Ag+, Cl− and S2−), and liquid membrane ion-selective electrodes (for example, electrodes based on ionophores (selective host molecules) for H+, K+, Na+, NH4+, Ca2+) are commercially available. Solid and liquid membrane electrodes can further be integrated into clinical analyzers for the detection of blood electrolytes (for example, Na+, K+, Ca2+, H+ and Cl−). Enzymes, nucleic acids and proteins can be detected by integrating the biological element on the ion-selective electrode to catalyze the reaction that forms the ions or by combining the target biorecognition event with an ionic reaction51,52,53,54.
Solid-contact ion-selective electrodes, which can be made with solvent polymeric membranes, do not contain internal solutions (Fig. 1c) and benefit from ruggedness (thus, morphological diversity) and easy fabrication, modification and miniaturization. Solid-contact ion-selective electrodes allow protein and nucleic acid analysis through the detection of ions released from nanoparticle-tagged probes; for example, a miniaturized solid-contact Ag ion-selective electrode can detect DNA targets at the femtomolar level in microlitre-volume samples55. In addition, all-solid-state ion-selective electrodes can be made with conducting polymers or nanomaterials to establish a solid contact beneath the ion-selective and reference membranes (Fig. 1c). Such ion-selective electrodes have been implemented in two commercial portable devices for POC detection of electrolytes and blood gases (i-STAT from Abbott and BGA-102 from Wondfo Biotech) (Supplementary Table 1). A paper-based potentiometric biosensor based on an all-solid-state butyrylcholine-sensitive ion-selective electrode and a 3D origami paper-based fluidic system can detect butyrylcholinesterase activity and organophosphate pesticides and, by further integrating a USB-controlled miniaturized electrochemical analyzer, allows the design of a handheld potentiometric device56. All-solid-state ion-selective electrodes can also be integrated into wearable devices for ionic detection in biofluids18,19,20,21; for example, a wearable ‘smart wristband’ with Na+ and K+ ion-selective electrodes on a flexible sensing array enables in situ analysis of Na+ and K+ in sweat57.
Organic electrochemical transistor biosensors
OECT biosensors are organic thin-film transistors that consist of gate (G), drain (D) and source (S) electrodes, with an organic semiconductor film between the D and S electrodes. A change in the potential drop or capacitance of the gate–electrolyte or channel–electrolyte interface sensitively changes the channel current. Thus, OECT biosensors can be fabricated by immobilizing the recognition element on the G electrode or on the channel surface (Fig. 1d); here, the specific reactions of the OECT biosensor with the target influence the interface potential, resulting in a channel current response for target quantification.
OECT biosensors benefit from high sensitivity, low cost, flexibility, easy fabrication and low working voltage (<1 V), allowing the detection of both electroactive (for example, dopamine, glucose and epinephrine)58,59,60 and electro-inactive (for example, cortisol61, DNA62, proteins63,64, bacteria65, cells66 and glycans67,68,69,70) molecules or biomacromolecules through electrostatic interactions or affinity binding between targets and the sensing interface71.
OECT biosensors can be easily miniaturized, integrated into devices and designed as arrays because their detection performance does not degrade if their size is reduced at a fixed channel width per length ratio. For example, a ‘lab on a chip’ system based on an OECT biosensor integrated into a flexible microfluidic system allows label-free detection of DNA with a detection limit of 10 pM; here, the microfluidic device is deposited on a flexible substrate that contains a thiolated DNA probe immobilized on the Au gate electrode62. OECT microarrays can also be fabricated by solution processes for high-throughput sensing. The flexibility and robustness of OECT biosensors make them suitable for the non-invasive detection of biomolecules in wearable devices. For example, a fabric OECT biosensor, fabricated by weaving the sensor with cotton yarns, can be embedded in a diaper to monitor glucose in artificial urine, with the sensing signals collected on a mobile phone through Bluetooth72.
Photoelectrochemical biosensors
Photoelectrochemistry studies the effect of light on photoelectrodes or interfacial materials and the conversion of light energy into electrical power. Photoelectrochemical biosensing combines photoelectrochemistry with sensor-based bioanalysis; here, light serves as the excitation source and current as the readout. Photoelectrochemical biosensing systems typically consist of a three-electrode system and a light source (Fig. 1e). Detection is based on the change of photocurrent upon target recognition at the biosensor surface, which induces a charge or energy transfer owing to the photoelectrochemical reaction between an electron donor and acceptor, and a photoactive material on the electrode surface upon light irradiation73.
Photoelectrochemical biosensors combine the advantages of optical and electrochemical assays, in particular, for the detection of disease-related molecules such as glutathione, lactate, DNA, microRNA (miRNA), protein tumour markers and cells73. Light stimuli can be applied contactless rather than through bias voltage, making photoelectrochemical biosensors biocompatible and suitable for in vivo sensing. In addition, separation of the excitation source (light) and detection signal (electricity) and their different energy forms result in low background noise and high sensitivity. Therefore, photoelectrochemical microbiosensors allow in vivo or single-cell analysis74,75; for example, using a fluorescence resonance energy transfer (FRET) process, a photoelectrochemical microbiosensing system can selectively monitor SO2, a potential marker of cerebral ischaemia (reperfusion) and related brain injury, in the brain of living rats76. Here, FRET is implemented based on upconversion nanoparticles (UCNPs) as the energy donor and an organic dye as the energy acceptor. The biosensing interface is then constructed by co-immobilization of the UCNP and dye FRET pair, and CdTe quantum dots on a microelectrode. In the brain of a rat model of cerebral ischaemia-reperfusion and febrile seizure, the presence of SO2 blocks the FRET process and recovers UCNP emission, which, in turn, modulates the photocurrent of the photoactive material, allowing the detection of SO2.
Electrochemiluminescence biosensing and bioimaging
Electrochemiluminescence is an electrochemically triggered energy-relaxation process, in which a luminophore undergoes electron transfer reactions to form excited states that emit light. Electrochemiluminescence biosensing enables the quantitative detection of target molecules through electrochemiluminescence emission signals that are associated with a target biorecognition-induced change in electrochemiluminescence active species. Similar to amperometric and voltammetric biosensors, electrochemiluminescence biosensors also operate with a three-electrode system, in which the WE is modified with the recognition element to serve as the biosensing electrode (Fig. 1f). Owing to the combination of electrochemistry and spectroscopy, electrochemiluminescence biosensing does not require a light source and has negligible background noise, high sensitivity, good reproducibility, and high spatial and temporal control, making it a powerful analytical tool for the detection of a range of disease molecules, including DNA, miRNA, proteins and tumour cells77,78,79.
A commercialized microbead-based electrochemiluminescence biosensing system (that is, Elecsys 1010/2010/E170, Roche Diagnostics) is used as the gold-standard detection system in hospitals for many glycoprotein tumour markers79; however, this instrument is large and bulky. Alternatively, a portable electrochemiluminescence device, integrating a screen-printed carbon electrode-based electrochemiluminescence biosensor, paper microfluidics and a mobile phone camera, can detect 2-(dibutylamino)-ethanol and NADH80. A portable electrochemiluminescence biosensing system has also been designed for the detection of miRNA-21 by combining a magnetic bead-based switch-on electrochemiluminescence molecular beacon sensing strategy with a portable potentiostat and a mobile phone camera readout81.
Electrochemiluminescence biosensing strategies can be combined with a charge-coupled device camera and a conventional microscope for electrochemiluminescence bioimaging. This system allows simultaneous detection of multiple biomarkers through spatial or potential resolution; for example, a bead-based electrochemiluminescence immunosensing array enables simultaneous detection of three antigens by individually imaging the microbeads located in a microwell array82. Similarly, electrochemiluminescent polymer dots (Pdots), luminol-doped Pdots and diethylamine-coupled Pdots can be exploited for potential-resolved and colour-resolved electrochemiluminescence bioimaging for the high-throughput detection of miRNAs83. Here, luminol-doped Pdots show blue electrochemiluminescence emission at +0.6 V, whereas diethylamine-coupled Pdots show red electrochemiluminescence emission at +1.0 V. On the sensing array, the electrochemiluminescence of two Pdots is initially inhibited by quencher-labelled capture DNAs. After recognition of target miRNAs, the quencher is released through DNA cleaving, and the electrochemiluminescence of Pdots is recovered for target detection. Compared to potential-resolved electrochemiluminescence biosensors, this potential-resolved and colour-resolved bioimaging system prevents interference of the threshold produced by the low potential emitter at high potentials.
Electrochemiluminescence bioimaging is well suited for cell analysis because it can provide both morphological and quantitative information84. Electrochemiluminescence cell bioimaging strategies have been developed for different targets, including small molecules released from cells and membrane proteins on the cell surface. Electrochemiluminescence imaging of membrane proteins is typically achieved by labelling cells with electrochemiluminescence probes through affinity reactions. However, this approach only allows observation of the cell periphery in contact with the electrode or requires membrane permeability treatment. Alternatively, a dual-intramolecular electron transfer strategy can be applied; for example, co-reactant-embedded Pdots with strong electrochemiluminescence emission enable in situ imaging of the membrane protein human epidermal growth factor receptor 2 (HER2) on single living cells85. To quantify detection, the biosensing interface, that is, a Pdot-modified-indium tin oxide (ITO) glass electrode sheet, can be combined with a single-cell-capture microfluidic chip, enabling high-throughput quantification of dopamine secreted by a single cell86.
Device integration
Electrochemical biosensors can be integrated into portable, wearable or implantable devices (Table 1), including microfluidics, printed circuit boards, software, signal processing units, communication units and power units (Fig. 1g). Amperometric biosensors are the most developed and most commonly used sensors for metabolites. Owing to the specific enzyme reaction, they usually exhibit good selectivity. In addition, the enzymatic catalytic signal can be further enhanced by nanomaterials, leading to high sensitivity. Most importantly, these enzyme sensors can be prepared in batches with good reproducibility; however, enzyme activity can be affected by the environment. Thus, robust sensing electrodes are required for work in different environments. Potentiometric biosensors can be integrated for wearable sweat monitoring, in particular, for the detection of electrolytes. Using ion-selective membranes, potentiometric biosensors show good selectivity, reproducibility and stability; however, their sensitivity is low. Alternatively, a flexible, all-solid-state, wearable, ion-selective electrode could achieve continuous sweat monitoring. Voltammetric, OECT, photoelectrochemical and electrochemiluminescent biosensors allow the detection of proteins and nucleic acids, showing good selectivity and high sensitivity. However, such affinity biosensors typically require the specific assembly of bioreceptors on the electrode surface, making their fabrication more complicated than that of enzyme electrodes.
Portable electrochemical biosensing devices
Portable electrochemical sensors have initially been developed for the monitoring of blood glucose levels in patients with diabetes87. The personal glucose meter is a portable electrochemical biosensor that provides rapid quantification of blood glucose levels for personal glycaemic control. The glucose meter, which is typically an amperometric biosensor based on a redox enzyme, consists of a disposable test strip and a pocket-sized handheld electrochemical reader (Fig. 2a). The disposable test strips can be fabricated by printing and cutting at a large scale using low-cost materials such as plastics and conductive pastes; for example, the thin-film electrodes on the test strips can be produced by screen-printing technology, which allows mass production at low cost88. The sensing layer containing the enzyme and the electron mediator is immobilized on the WE for the detection of glucose. Once the blood sample is introduced to the small chamber (electrochemical cell) formed by the spacer layer on the test strip, blood glucose is oxidized by the redox mediator, which is catalyzed by GOx (Fig. 2a). The reduced mediator is then oxidized on the electrode, producing a measurable current signal89, which is converted to glucose concentration by a handheld detector. The personal glucose meter is a result of continuous engineering advances to increase its accuracy, reliability, user-friendliness and affordability90,91 since the first concept of glucose enzyme electrodes was proposed in the 1960s1.
a, Portable blood glucose meter consisting of a handheld electrochemical detector and disposable test strips. The test strip contains a bottom electrode layer, an adhesive spacer layer and a hydrophilic cover layer. The blood sample is introduced to the reaction chamber by capillary force. b, A paper-based microfluidic electrochemical biosensor for the detection of adenosine through aptamer-based affinity sensing. In one channel, adenosine is recognized by aptamer-functionalized microbeads (blue), resulting in the release of glucose oxidase-labelled DNA to catalyze the oxidation of glucose, which leads to the conversion of [Fe(CN)6]3− to [Fe(CN)6]4−. In the other channel, the microbeads are not functionalized (purple), allowing quantification of adenosine concentration. The current signal from the discharging of the capacitor is collected by a portable digital multimeter. ox, oxidation; red, reduction. Part b reprinted with permission from ref. 104, Wiley.
The personal glucose meter can also detect metal ions, drugs, organic metabolites, enzymes, proteins, DNA and influenza viruses by relating target recognition events with the generation or consumption of glucose92,93,94,95,96,97. For example, the personal glucose meter can quantify cocaine, adenosine and uranium in blood through the target-induced release of invertase, from a DNA–invertase conjugate, that catalyzes the conversion of sucrose to glucose92. Moreover, the device can quantitatively detect SARS-CoV-2 antigen in human saliva for COVID-19 screening97; here, antigen-binding events are translated into glucose signals using an aptamer-based competitive mechanism that leads to invertase release to catalyze sucrose hydrolysis. This on-site test can be accomplished within 1 h with a picomolar limit of detection.
For complex samples that require pre-treatment, signal amplification and continuous analysis, electrochemical biosensors can be combined with microfluidic systems98,99, for example, for the detection of SARS-CoV-2 RNA100. In this device, RNA is detected by a reconfigurable enzyme–DNA nanostructure, which comprises DNA strands with inhibitor and inverter sequences that are bound to a Taq DNA polymerase through a cascading molecular circuitry enhancement; here, the biorecognition of target RNA by inverter sequences activates polymerase activity for downstream DNA amplification, labelling and electrochemical detection. The entire assay is automatically completed by a pressure-actuated microfluidic device with embedded sensing electrodes. Electrochemical biosensors can also be integrated with paper microfluidic devices by directly printing electrodes on paper. Paper-based microfluidics is cheap, biodegradable, easy to fabricate and allows pumpless fluidic transport by capillary actions101,102. In addition, paper can be folded (origami) to assemble 3D devices and control fluidic and electrical connectivity for programmed analytical processes103,104,105; for example, paper with patterned fluidic channels and electrodes can be assembled into a 3D configuration by folding and lamination for the detection of adenosine104 (Fig. 2b). In this device, the adenosine sample is first split into two symmetrical channels. In one channel, adenosine binds an aptamer immobilized on microbeads, which causes the release of GOx-labelled DNA and leads to the conversion of [Fe(CN)6]3− to [Fe(CN)6]4−. In the other channel, the microbeads do not contain the aptamer, leading to different redox concentrations in the cells, allowing the quantitative analysis of adenosine in a portable digital multimeter.
Miniaturized electrochemical analyzers can also be connected to smartphones for powering, processing and storage of data and to display results106. In addition, the test results can be uploaded to mobile health services107. For example, an open-source portable electrochemical detector that can establish wireless communication with a smartphone can be combined with electrochemical biosensors106,108.
Integration into wearable devices
Wearable sensors can be integrated with smartwatches, bracelets and glasses for physiological monitoring, for example, of heart rate, electrocardiogram and electroencephalogram109. Such wearable biosensors also allow non-invasive and continuous monitoring of analytes in body fluids (Fig. 3a), providing invaluable data for diagnostics and health management109,110,111. For example, the concentrations of glucose in non-blood body fluids, such as sweat and tears, can be converted to their corresponding blood levels through a correlation coefficient obtained from a correlation study between glucose concentration in blood and non-blood biofluids26,112, considering time lags for glucose secretion in different biofluids113,114,115. Compared to portable electrochemical biosensors, of which some have already been commercialized (Supplementary Table 1), wearable electrochemical biosensors are not yet at the same development stage.
a, Wearable sensors can be applied to monitor health-related or disease-related analytes in different body fluids, including tears, saliva and sweat. b, Health management can be based on continuous monitoring using wearable devices, including electrochemical biosensors, power supply and wireless communication modules. BC, biocapacitor; BFC, biofuel cell; PENG, piezoelectric nanogenerator; TENG, triboelectric nanogenerator.
Thus far, wearable electrochemical biosensors have mainly been explored for glucose monitoring because glucose can be detected in sweat, saliva and tears116,117,118. Compared to the conventional finger-prick test, wearable glucose analysis allows non-invasive and continuous monitoring, even during sleep, enabling timely feedback for diabetes management. A wearable integrated sensing array allows multiplexed detection of sweat biomarkers, including metabolites and electrolytes (such as glucose, lactate, Na+ and K+); here, signal conditioning, processing and wireless data transmission for in situ sweat analysis are achieved by flexible printed circuit boards57. Such integrated wearable electrochemical biosensors allow non-invasive and dynamic monitoring of the health status at the molecular level, for example, for in situ monitoring of wound healing119, therapeutic drugs, drug abuse120, nutrition121 and the diagnosis of cystic fibrosis114. Wearable electrochemical biosensors can also be incorporated into robots to sense hazardous materials and pathogens for agriculture, security and public health applications122.
Sampling plays an important role in wearable biosensing. The concentration of biochemical analytes in secreted body fluids is affected by various factors, including reabsorption, evaporation, secretion rate, interfering substances and metabolism of the secretion glands109,113,123. Microfluidic devices can be applied for sample collection; for example, sweat can be enriched and transported to a sensor module in a microfluidic device, reducing sweat reabsorption and evaporation, and allowing real-time continuous monitoring. Moreover, a microfluidic sweat sampling device can be designed to collect small volumes of sweat, enabling continuous sweat monitoring at rest by entrapping thermoregulatory-generated sweat in a microfluidic channel124. This design may facilitate wearable sweat sensing platforms that do not require large sweat volumes, for example, during exercise or at high ambient temperatures, making sweat sensing compatible with daily activities. Microfluidic devices with fluidic valves further allow in situ manipulation of collected biofluids, for example, to achieve chrono-sampling of sweat for time-dependent analysis of biomarker variation125. An epidermal microfluidic device with thermo-responsive hydrogel valves enables active control of sweat126, that is, on-demand delivery of sweat to the sensing electrode, thereby eliminating the influence of flow rate variability on the sensor response and allowing scheduled sweat analysis. Although promising for on-body biofluid detection, electrochemical bioassays in this device remain difficult because they require multistep operations for incubation, amplification and washing, limiting its use to monitor protein and nucleic acid biomarkers in sweat. Therefore, innovative fluidic control units are needed to automate multistep bioassays.
A power source is indispensable for continuous electrochemical analysis in wearable devices. Self-powered devices can generate energy from human motion127,128,129 using a piezoelectric nanogenerator130,131 or a triboelectric nanogenerator132,133,134 that converts mechanical energy into electrical energy. For example, a self-powered wearable device based on a triboelectric nanogenerator printed on a flexible circuit board enables continuous monitoring of H+ and Na+ in sweat135; here, the output of the power source (~416 mW m–2) can power the multiplexed biosensor and the design allows miniaturization. A triboelectric self-powered sweat sensor based on nanocellulose hydrogels with self-healing ability can monitor ions (Na+, K+, Ca2+) in sweat136. Alternatively, biofuel cells can power wearable biosensors by harvesting energy from redox substances in biological fluids through bioelectrocatalytic reactions128,137,138; for example, using ascorbate in tears as the fuel, a self-powered contact lens can monitor tear glucose levels139. Similarly, a self-powered wireless sensing system based on glucose and lactate biofuel cells can monitor sweat glucose and lactate levels140. If a single power source is insufficient to power the device, a microgrid system incorporating biofuel cells, triboelectric generators and supercapacitors can provide higher power output141.
Long-term wearable electrochemical biosensors can be designed with flexible electrode materials (for example, metals, conductive polymers and low-dimensional materials) that resist mechanical deformation (for example, strain and bending) and that can be self-healing142. In addition, flexible, printed circuit boards that contain full-featured microcontrollers and other components, such as communication modules, can be designed by commercial software, such as the Altium Designer, and fabricated by commercially printed circuit board manufacturers143. Wireless information communication technologies, such as Bluetooth57,144 and near-field communication145,146, have low power consumption and acceptable communication distance, allowing sensing devices to communicate with remote electronic systems such as smartphones, which can analyze, display and store data (Fig. 3b).
However, the performance of wearable biosensors is limited by variations in connectivity and impedances caused by human physical activities that can lead to detection errors. Signal processing and calibration algorithms can be applied to correct for such artefacts147; for example, electrochemical signals that are affected by pH, temperature and flow rate can be calibrated by a multiplexed sensing strategy using lookup tables for real-time and automated calibration57. To reduce signal variation, an accelerometer can further be integrated and the signal can be filtered using short-time fast Fourier transform. More advanced frequency-domain algorithms, such as the wavelet-transform projection, can be employed to decouple motions from the electrochemical measurement148. Furthermore, the relative change in electrochemical signal (for example, Nernstian shift) can be used instead of the absolute signal value to decrease measurement errors149.
Integration into implantable devices
Finger-prick blood tests using portable electrochemical devices are usually highly accurate but require frequent, invasive sample collection150. Wearable electrochemical biosensing is non-invasive but suffers from low analytical accuracy, which is a particular concern in diagnostic applications151,152. Alternatively, implantable electrochemical biosensors combine the high accuracy of invasive finger-prick tests and the long-term monitoring capability of non-invasive wearable analysis153,154. Implantable electrochemical biosensors have been particularly explored for continuous glucose monitoring and in vivo monitoring of biomarkers, such as neurochemicals, in the brain155,156,157,158 (Fig. 4).
a, Microneedle-based implantable electrochemical biosensors for the monitoring of analytes in interstitial fluid. The working electrode is modified with multiple functional layers, including an inner sensing layer consisting of a redox polymer and an enzyme, a mass transport-limiting layer to improve stability, and an outer biocompatible layer to prevent fouling of the sensor. b, Implantable electrochemical biosensors allow continuous glucose monitoring and in vivo detection of neurochemicals in the brain.
In electrochemical biosensors, the detection reaction occurs on the surface of the electrodes and, thus, such sensors can easily be integrated with circuitry and incorporated into a small capsule for implantation159,160. Implantable electrochemical biosensors (for example, subcutaneous or intravascular) can provide dynamic information on glucose levels to guide therapy adjustments157,161,162,163. Similarly, spatiotemporal electrochemical sensing of neurochemicals, such as dopamine and acetylcholine, in the brain can indicate neuronal activity164,165,166.
Most implantable electrodes are made of Au, Pt and Ir, which are electrochemically stable and, in principle, biocompatible155,167,168. However, as foreign bodies, implantable devices are subject to biofouling and the foreign body response, compromising their analytical performance169. Therefore, the electrode has to be coated with multiple functional layers, including an inner sensing layer consisting of redox polymer and enzyme, a middle layer to improve stability, and an outer biocompatible layer to prevent fouling of the sensor170,171 (Fig. 4a). For example, NO-releasing polymer coatings can improve the biocompatibility of implantable biosensors (for example, intravascular sensors) because the endogenous gas molecule NO inhibits platelet adhesion and activation, inflammatory responses, and bacterial growth148,172. In addition, implantable devices need to be sterilized; thus, the coating layers need to withstand sterilization treatments such as irradiation173.
The mechanical mismatch between soft tissues and implantable electrodes may lead to inflammatory responses and/or device failure. Therefore, implantable electrodes should be soft and stretchable to seamlessly interface with soft tissues. For example, a soft implantable neurotransmitter sensor can monitor the dynamics of monoamine in the brain and gut of mice174; here, the soft, elastic and thin electrode is fabricated by embedding laser-induced graphene nanofibres in an elastomer matrix, minimizing damage to intestinal tissue and not disturbing the peristaltic movement of the gastrointestinal tract.
Implantable biosensors typically remain in the body for long time periods, which requires an adequate power supply175 with high volumetric energy density (that is, the energy stored per unit of volume) owing to the constraint of the device size152,155. Batteries have high energy densities but require periodic replacement, which may risk infection and additional costs176. Alternatively, implantable electrochemical biosensors could be made self-powered using piezoelectric materials, triboelectric materials or fuel cells156,177,178,179,180. In addition, near-field communication may enable wireless power generation and data transmission159,181.
Alternative to implantable devices that typically require surgery, partially implantable electrochemical biosensors have been commercialized (for example, Freestyle Libre from Abbott and G6 CGM system from Dexcom)154,182 (Supplementary Table 1). Such partially implantable biosensors only require subcutaneous insertion of a small probe (for example, a flexible needle) or a probe array, leaving most components, including the power source, readout circuitry and wireless communication modules, on the surface of the skin151,162. For example, minimally invasive biosensors for glucose detection allow continuous glucose monitoring for about 2 weeks and can then be replaced by the patient161,183. However, these glucose biosensors are limited to single analyte analysis and may cause discomfort owing to the long needles (5–11 mm) that need to be inserted to access interstitial fluid. To achieve multiplexed analysis of biomarkers and discomfort-free operation, an integrated microneedle array can be applied that allows continuous monitoring of two analytes (for example, lactate and glucose, or alcohol and glucose) in interstitial fluid184. This device integrates reusable electronics to acquire and wirelessly transmit the electrochemical signals to a smartphone for data analysis and visualization.
Outlook
Electrochemical biosensors are powerful tools to quantitatively analyze biochemical analytes in body fluids, providing digital data of dynamic physiological processes for fundamental research and health-care applications. The integration of electrochemical biosensors in portable, wearable and implantable devices enables decentralized POC detection185,186,187, which has the potential to revolutionize diagnostics and health management188, particularly in low-resource settings (Box 1). Batch fabrication and integration of disposable, flexible and multi-electrode electrochemical biosensors with different substrates, including plastics, flexible films, textiles and paper, can be achieved by printing (for example, screen28,29,30, inkjet122, roll-to-roll189 and transfer190 printing) and microfabrication (for example, photolithography57, evaporation124, electron beam evaporation114,119 and laser cutter121); however, engineering challenges remain to be addressed for integrated electrochemical biosensors to make a real impact in POC diagnostics; for example, signal transduction, conditioning (amplification and filtering), processing and wireless transmission need to be improved57; all functional controllers and modules should be integrated on one circuit board; packaging of soft electronics and chipsets needs to be optimized; and microminiaturization, networking and intellectualization of devices needs to be realized191 (Box 2).
Beyond glucose sensing, electrochemical biosensing devices could also allow the POC detection of proteins, nucleic acids, viruses and cells; however, this will require automated multistep and multisolution technology. Digital microfluidics may enable full-automatic on-chip measurements but requires high-precision instruments, limiting its applications in low-resource settings. Therefore, simple, cheap, robust and stable microfluidic systems need to be developed, for example, using paper or hydrophilic and hydrophobic polymers, which can be folded and/or printed into low-cost, disposable devices. Importantly, electrochemical biosensors need to be engineered that achieve one-step biosensing to avoid complex handling processes. In addition, although amperometric, voltammetric, potentiometric and electrochemiluminescent biosensor devices have been commercialized, these are often invasive portable devices rather than non-invasive wearable and implantable devices, in particular, OECT, photoelectrochemical and electrochemiluminescent bioimaging biosensors are still at an early stage. Thus, electrochemical sensors need to be developed according to their specific properties; for example, OECT sensors can be developed for miniaturized wearable devices and photoelectrochemical sensors can be developed for miniaturized composite implantable devices (Table 1).
Smartphones, 5G communication and cloud computing will allow the digitalization of health-related information obtained by integrated electrochemical biosensors. For example, physical sensors connected and/or integrated into smartphones, watches or wristbands allow the daily monitoring of vital signs such as heart rate, electrocardiogram and electroencephalogram. Similarly, electrochemical biosensors can be integrated into wearable devices for the non-invasive monitoring of specific analytes in body fluids related to health management.
Engineering efforts are often dedicated to improving the sensitivity, selectivity and multiplex capability of electrochemical biosensors, making these devices increasingly complex and prone to failure. However, detection sensitivity and selectivity mainly depend on the recognition reaction at the delicate electrolyte–electrode interface, which is affected by a range of factors, such as the friction between electrodes and tissues, and the dynamic change of pH, flow rate and temperature of the body fluid, particularly in wearable devices. Therefore, more robust and maintenance-free electrochemical biosensors need to be designed that allow long-term health monitoring; for example, enzyme-based sensing chemistry can be replaced by nanomaterial-based catalytic sensing chemistry, which is less influenced by environmental conditions such as temperature, pH and ionic strength. In addition, the accuracy and reliability of electrochemical biosensors could be improved by implementing biosensor arrays that enable multiple detections in different environmental conditions. Such arrays can be built using all-solid-state electrodes, which can easily be integrated into printed circuit boards. The convoluted signals measured by the array can then be deconvoluted using algorithms, such as Fourier and wavelet transformation, to achieve simultaneous, multiplex detection. Furthermore, sensing accuracy could be improved by applying techniques commonly used in electrocardiograms, electromyograms and magnetic resonance imaging; for example, compressed sensing, which enables sub-Nyquist processing of sparse signals192,193.
Commercialization and broad applicability of integrated electrochemical biosensors will require concerted efforts in refining sensing techniques and flexible materials and in consolidating electronics, wireless electronics, data processing and data mining.
References
Clark, L. C. Jr & Lyons, C. Electrode systems for continuous monitoring in cardiovascular surgery. Ann. NY Acad. Sci. 102, 29–45 (1962).
Lambrianou, A., Demin, S. & Hall, E. A. H. Biosensing for the 21st Century (eds Renneberg, R., & Lisdat, F.) 65–95 (Springer, 2007).
Labib, M., Sargent, E. H. & Kelley, S. O. Electrochemical methods for the analysis of clinically relevant biomolecules. Chem. Rev. 116, 9001–9090 (2016). This review introduces electrochemical sensors fabricated with different recognition elements for the detection of small molecules, nucleic acids and proteins.
Wu, J., Fu, Z. F., Yan, F. & Ju, H. X. Biomedical and clinical applications of immunoassays and immunosensors for tumor markers. Trends Anal. Chem. 26, 679–688 (2007).
Minteer, S. D. Advances in electroanalytical chemistry. J. Am. Chem. Soc. 140, 2701–2703 (2018).
Zhang, J. J., Xiang, Y., Wang, M., Basu, A. & Lu, Y. Dose-dependent response of personal glucose meters to nicotinamide coenzymes: applications to point-of-care diagnostics of many non-glucose targets in a single step. Angew. Chem. Int. Ed. 128, 742–746 (2016).
Das, A., Cui, X. K., Chivukula, V. & Iyer, S. S. Detection of enzymes, viruses, and bacteria using glucose meters. Anal. Chem. 90, 11589–11598 (2018).
Gong, S. H., Li, J. J., Pan, W., Li, N. & Tang, B. Duplex-specific nuclease-assisted CRISPR-Cas12a strategy for microRNA detection using a personal glucose meter. Anal. Chem. 93, 10719–10726 (2021).
Liu, R., Hu, Y. S., He, Y., Lan, T. & Zhang, J. J. Translating daily COVID-19 screening into a simple glucose test: a proof of concept study. Chem. Sci. 12, 9022–9030 (2021).
Cao, Y. Z. et al. Portable and sensitive detection of non-glucose target by enzyme-encapsulated metal-organic-framework using personal glucose meter. Biosens. Bioelectron. 198, 113819 (2022).
Lubin, A. A. & Plaxco, K. W. Folding-based electrochemical biosensors: the case for responsive nucleic acid architectures. Acc. Chem. Res. 43, 496–505 (2010). This review of folding-based electrochemical biosensors research opens up ways to fabricate one-step response affinity biosensors for nucleic acid and protein targets.
Zhang, H. Q., Li, F., Dever, B., Li, X. F. & Le, X. C. DNA-mediated homogeneous binding assays for nucleic acids and proteins. Chem. Rev. 113, 2812–2841 (2013). This review introduces proximity binding-based affinity sensing mechanisms for one-step, homogenous detection of nucleic acid and protein targets.
Liu, B. W., Du, D., Hua, X., Yu, X. Y. & Lin, Y. H. Paper-based electrochemical biosensors: from test strips to paper-based microfluidics. Electroanalysis 26, 1214–1223 (2014).
Sassa, F., Biswas, G. C. & Suzuki, H. Microfabricated electrochemical sensing devices. Lab Chip 20, 1358–1389 (2020).
Noviana, E., McCord, C. P., Clark, K. M., Jang, I. & Henry, C. S. Electrochemical paper-based devices: sensing approaches and progress toward practical applications. Lab Chip 20, 9–34 (2020).
Lei, J. P. & Ju, H. X. Signal amplification using functional nanomaterials for biosensing. Chem. Soc. Rev. 41, 2122–2134 (2012). This review introduces nanomaterial-based signal amplification strategies, including functionalization methods for nanoprobes and surfaces, the functions of nanomaterials and their applications for ultrasensitive biosensing of biomolecules.
Ju, H. X. Biosensors: signal amplification for highly sensitive bioanalysis based on biosensors or biochips. J. Biochips Tissue Chips 2, e114 (2012).
Heikenfeld, J. et al. Accessing analytes in biofluids for peripheral biochemical monitoring. Nat. Biotech. 37, 407–419 (2019).
Yu, Y., Nyein, H. Y. Y., Gao, W. & Javey, A. Flexible electrochemical bioelectronics: the rise of in situ bioanalysis. Adv. Mater. 32, 1902083 (2020).
Xu, C. H., Yang, Y. R. & Gao, W. Skin-interfaced sensors in digital medicine: from materials to applications. Matter 2, 1414–1445 (2020).
Song, Y., Min, J. H. & Gao, W. Wearable and implantable electronics: moving toward precision therapy. ACS Nano 13, 12280–12286 (2019).
Hussein, H. A. et al. SARS-CoV-2-impedimetric biosensor: virus-imprinted chips for early and rapid diagnosis. ACS Sens. 6, 4098–4107 (2021).
Zeng, J. et al. An impedimetric biosensor for COVID-19 serology test and modification of sensor performance via dielectrophoresis force. Biosen. Bioelectron. 213, 114476 (2022).
Karyakin, A. A., Gitelmacher, O. V. & Karyakina, E. E. Prussian blue-based first-generation biosensor: a sensitive amperometric electrode for glucose. Anal. Chem. 67, 2419–2423 (1995).
Ju, H. X., Zhang, X. J. & Wang, J. NanoBiosensing: Principles, Development and Application 85–102 (Springer, 2011).
Kim, S. K. et al. Bimetallic nanocatalysts immobilized in nanoporous hydrogels for long-term robust continuous glucose monitoring of smart contact lens. Adv. Mater. 34, 2110536 (2022).
Huang, Y. Z., Han, Y. K., Sun, J. Y., Zhang, Y. & Han, L. Dual nanocatalysts co-decorated three-dimensional, laser-induced graphene hybrid nanomaterials integrated with a smartphone portable electrochemical system for point-of-care non-enzymatic glucose diagnosis. Mater. Today Chem. 24, 100895 (2022).
Wu, J. et al. A disposable electrochemical immunosensor for flow injection immunoassay of carcinoembryonic antigen. Biosens. Bioelectron. 22, 102–108 (2006).
Wu, J., Yan, F., Tang, J. H., Zhai, C. & Ju, H. X. A disposable multianalyte electrochemical immunosensor array for automated simultaneous determination of tumor markers. Clin. Chem. 53, 1495–1502 (2007).
Wu, J. et al. Disposable reagentless electrochemical immunosensor array based on a biopolymer/sol-gel membrane for simultaneous measurement of several tumor markers. Clin. Chem. 54, 1481–1488 (2008).
Fernandez-la-Villa, A., Pozo-Ayuso, D. F. & Castano-Alvarez, M. Microfluidics and electrochemistry: an emerging tandem for next-generation analytical microsystems. Curr. Opin. Electrochem. 15, 175–185 (2019).
Kikkeri, K., Wu, D. & Voldman, J. A sample-to-answer electrochemical biosensor system for biomarker detection. Lab Chip 22, 100–107 (2022).
Koklu, A. et al. Microfluidic integrated organic electrochemical transistor with a nanoporous membrane for amyloid-beta detection. ACS Nano 15, 8130–8141 (2021).
Sun, S. et al. Multifunctional self-driven origami paper-based integrated microfluidic chip to detect CRP and PAB in whole blood. Biosens. Bioelectron. 208, 114225 (2022).
Feng, D. Z. et al. DNA tetrahedron-mediated immune-sandwich assay for rapid and sensitive detection of PSA through a microfluidic electrochemical detection system. Microsyst. Nanoeng. 7, 33 (2021).
Lee, G. H. et al. Single microfluidic electrochemical sensor system for simultaneous multi-pulmonary hypertension biomarker analyses. Sci. Rep. 7, 7545 (2017).
Pursey, J. P., Chen, Y., Stulz, E., Park, M. K. & Kongsuphol, P. Microfluidic electrochemical multiplex detection of bladder cancer DNA markers. Sens. Actuators B Chem. 251, 34–39 (2017).
Fragoso, A. et al. Integrated microfluidic platform for the electrochemical detection of breast cancer markers in patient serum samples. Lab Chip 11, 625–631 (2011).
Zhao, Y. X., Chen, F., Li, Q., Wang, L. H. & Fan, C. H. Isothermal amplification of nucleic acids. Chem. Rev. 115, 12491–12545 (2015).
Simmel, F. C., Yurke, B. & Singh, H. R. Principles and applications of nucleic acid strand displacement reactions. Chem. Rev. 119, 6326–6369 (2019).
Dai, Y. F. et al. Exploring the trans-cleavage activity of CRISPR-Cas12a (cpf1) for the development of a universal electrochemical biosensor. Angew. Chem. Int. Ed. 58, 17399–17405 (2019).
Zhang, D. C. et al. CRISPR/Cas12a-mediated interfacial cleaving of hairpin DNA reporter for electrochemical nucleic acid sensing. ACS Sens. 5, 557–562 (2020).
Hu, J. M., Wang, T. Y., Kim, J., Shannon, C. & Easley, C. J. Quantitation of femtomolar protein levels via direct readout with the electrochemical proximity assay. J. Am. Chem. Soc. 134, 7066–7072 (2012).
Hu, J. M. et al. A reusable electrochemical proximity assay for highly selective, real-time protein quantitation in biological matrices. J. Am. Chem. Soc. 136, 8467–8474 (2014).
Ren, K. W., Wu, J., Yan, F. & Ju, H. X. Ratiometric electrochemical proximity assay for sensitive one-step protein detection. Sci. Rep. 4, 4360 (2014).
Ren, K. W., Wu, J., Yan, F., Zhang, Y. & Ju, H. X. Immunoreaction-triggered DNA assembly for one-step sensitive ratiometric electrochemical biosensing of protein biomarker. Biosens. Bioelectron. 66, 345–349 (2015).
Ren, K. W., Wu, J., Zhang, Y., Yan, F. & Ju, H. X. Proximity hybridization regulated DNA biogate for sensitive electrochemical immunoassay. Anal. Chem. 86, 7494–7499 (2014).
Ren, K. W., Wu, J., Ju, H. X. & Yan, F. Target-driven triple-binder assembly of MNAzyme for amplified electrochemical immunosensing of protein biomarker. Anal. Chem. 87, 1694–1700 (2015).
Zhu, J., Gan, H. Y., Wu, J. & Ju, H. X. Molecular machine powered surface programmatic chain reaction for highly sensitive electrochemical detection of protein. Anal. Chem. 90, 5503–5508 (2018).
Man, Y. et al. An anchored monopodial DNA walker triggered by proximity hybridization for amplified amperometric biosensing of nucleic acid and protein. Anal. Chim. Acta 1107, 48–54 (2020).
Karimi-Maleh, H. et al. A critical review on the use of potentiometric based biosensors for biomarkers detection. Biosens. Bioelectron. 184, 113252 (2021).
Ding, J. W., Chen, Y., Wang, X. W. & Qin, W. Label-free and substrate-free potentiometric aptasensing using polycation-sensitive membrane electrodes. Anal. Chem. 84, 2055–2061 (2012).
Nurlely, A. M., Heng, L. Y. & Tan, L. L. Potentiometric enzyme biosensor for rapid determination of formaldehyde based on succinimide-functionalized polyacrylate ion-selective membrane. Measurement 175, 109112 (2021).
Özbek, O., Berkel, C., Isildak, Ö. & Isildak, I. Potentiometric urea biosensors. Clin. Chim. Acta 524, 154–163 (2022).
Wu, J. et al. Potentiometric detection of DNA hybridization using enzyme-induced metallization and a silver ion selective electrode. Anal. Chem. 81, 10007–10012 (2009).
Ding, J. W., Li, B. W., Chen, L. X. & Qin, W. A three-dimensional origami paper-based device for potentiometric biosensing. Angew. Chem. Int. Ed. 55, 13033–13037 (2016).
Gao, W. et al. Fully integrated wearable sensor arrays for multiplexed in situ perspiration analysis. Nature 529, 509–514 (2016). This article demonstrates a mechanically flexible and fully integrated wearable system for sweat metabolites and electrolytes as well as for skin temperature monitoring.
Tang, H., Yan, F., Lin, P., Xu, J. B. & Chan, H. L. W. Highly sensitive glucose biosensors based on organic electrochemical transistors using platinum gate electrodes modified with enzyme and nanomaterials. Adv. Funct. Mater. 21, 2264–2272 (2011).
Tang, H., Lin, P., Chan, H. L. W. & Yan, F. Highly sensitive dopamine biosensors based on organic electrochemical transistors. Biosens. Bioelectron. 26, 4559–4563 (2011).
Mak, C. H. et al. Highly-sensitive epinephrine sensors based on organic electrochemical transistors with carbon nanomaterial modified gate electrodes. J. Mater. Chem. C. 3, 6532–6538 (2015).
Parlak, O., Keene, S. T., Marais, A., Curto, V. F. & Salleo, A. Molecularly selective nanoporous membrane-based wearable organic electrochemical device for noninvasive cortisol sensing. Sci. Adv. 4, eaar2904 (2018).
Lin, P., Luo, X. T., Hsing, I. M. & Yan, F. Organic electrochemical transistors integrated in flexible microfluidic systems and used for label-free DNA sensing. Adv. Mater. 23, 4035–4040 (2011).
Fu, Y. et al. Highly sensitive detection of protein biomarkers with organic electrochemical transistors. Adv. Mater. 29, 1703787 (2017).
Kim, D. J. et al. Organic electrochemical transistor based immunosensor for prostate specific antigen (PSA) detection using gold nanoparticles for signal amplification. Biosens. Bioelectron. 25, 2477–2482 (2010).
He, R. X. et al. Detection of bacteria with organic electrochemical transistors. J. Mater. Chem. 22, 22072–22076 (2012).
Lin, B. P., Yan, F., Yu, J. J., Chan, H. L. W. & Yang, M. The application of organic electrochemical transistors in cell-based biosensors. Adv. Mater. 22, 3655–3660 (2010).
Chen, L. Z. et al. Organic electrochemical transistors for the detection of cell surface glycans. ACS Appl. Mater. Interfaces 10, 18470–18477 (2018).
Chen, L. Z., Wang, N. X., Wu, J., Yan, F. & Ju, H. X. Organic electrochemical transistor for sensing of sialic acid in serum samples. Anal. Chim. Acta 1128, 231–237 (2020).
Chen, L. Z., Wu, J., Yan, F. & Ju, H. X. A facile strategy for quantitative sensing of glycans on cell surface using organic electrochemical transistors. Biosens. Bioelectron. 175, 112878 (2021).
Chen, L. Z., Wu, J., Yan, F. & Ju, H. X. Monose-modified organic electrochemical transistors for cell surface glycan analysis via competitive recognition to enzyme-labeled lectin. Mikrochim. Acta 188, 1–7 (2021).
Wang, N., Yang, A., Fu, Y., Li, Y. & Yan, F. Functionalized organic thin film transistors for biosensing. Acc. Chem. Res. 52, 277–287 (2019).
Yang, A. N. et al. Fabric organic electrochemical transistors for biosensors. Adv. Mater. 30, 1800051 (2018).
Zang, Y., Lei, J. P. & Ju, H. X. Principles and applications of photoelectrochemical sensing strategies based on biofunctionalized nanostructures. Biosens. Bioelectron. 96, 8–16 (2017).
Ruan, Y. F. et al. An integrated photoelectrochemical nanotool for intracellular drug delivery and evaluation of treatment effect. Angew. Chem. Int. Ed. 133, 25966–25969 (2021).
Hu, F. X., Miao, J. W., Guo, C. X., Yang, H. B. & Liu, B. Real-time photoelectrochemical quantification of hydrogen peroxide produced by living cells. Chem. Eng. J. 407, 127203 (2021).
Ye, X. X. et al. FRET modulated signaling: a versatile strategy to construct photoelectrochemical microsensors for in vivo analysis. Angew. Chem. Int. Ed. 60, 11774–11778 (2021).
Qi, H. L. & Zhang, C. X. Electrogenerated chemiluminescence biosensing. Anal. Chem. 92, 524–534 (2020).
Chen, Y. H. & Ding, Z. F. Highly sensitive analysis strategies of microRNAs based on electrochemiluminescence. Curr. Opin. Electrochem. 32, 100901 (2022).
Miao, W. J. Electrogenerated chemiluminescence and its biorelated applications. Chem. Rev. 108, 2506–2553 (2008).
Delaney, J. L., Hogan, C. F., Tian, J. & Shen, W. Electrogenerated chemiluminescence detection in paper-based microfluidic sensors. Anal. Chem. 83, 1300–1306 (2011).
Kerr, E. et al. Amplification-free electrochemiluminescence molecular beacon-based microRNA sensing using a mobile phone for detection. Sens. Actuators B Chem. 330, 129261 (2021).
Deiss, F. et al. Multiplexed sandwich immunoassays using electrochemiluminescence imaging resolved at the single bead level. J. Am. Chem. Soc. 131, 6088–6089 (2009).
Wang, N. N., Chen, L. Z., Chen, W. W. & Ju, H. X. Potential-and color-resolved electrochemiluminescence of polymer dots for array imaging of multiplex microRNAs. Anal. Chem. 93, 5327–5333 (2021).
Ma, C., Cao, Y., Gou, X. D. & Zhu, J. J. Recent progress in electrochemiluminescence sensing and imaging. Anal. Chem. 92, 431–454 (2020).
Wang, N. N. et al. Dual intramolecular electron transfer for in situ coreactant‐embedded electrochemiluminescence microimaging of membrane protein. Angew. Chem. Int. Ed. 60, 197–201 (2021).
Wang, N. N. et al. Confined electrochemiluminescence imaging microarray for high-throughput biosensing of single cell-released dopamine. Biosens. Bioelectron. 201, 113959 (2022).
Teymourian, H., Barfidokht, A. & Wang, J. Electrochemical glucose sensors in diabetes management: an updated review (2010-2020). Chem. Soc. Rev. 49, 7671–7709 (2020).
Nagata, R., Yokoyama, K., Clark, S. A. & Karube, I. A glucose sensor fabricated by the screen printing technique. Biosens. Bioelectron. 10, 261–267 (1995).
Wang, J. Electrochemical glucose biosensors. Chem. Rev. 108, 814–825 (2008).
Tonyushkina, K. & Nichols, J. H. Glucose meters: a review of technical challenges to obtaining accurate results. J. Diabetes Sci. Technol. 3, 971–980 (2009).
Karon, B. S., Boyd, J. C. & Klee, G. G. Glucose meter performance criteria for tight glycemic control estimated by simulation modeling. Clin. Chem. 56, 1091–1097 (2010).
Xiang, Y. & Lu, Y. Using personal glucose meters and functional DNA sensors to quantify a variety of analytical targets. Nat. Chem. 3, 697–703 (2011). This article demonstrates a method based on the target-induced release of invertase from a functional DNA–invertase conjugate to enable the quantification of non-glucose targets using a commercial personal glucose metre.
Zhang, J. & Lu, Y. Biocomputing for portable, resettable, and quantitative point-of-care diagnostics: making the glucose meter a logic-gate responsive device for measuring many clinically relevant targets. Angew. Chem. Int. Ed. 57, 9702–9706 (2018).
Amalfitano, E. et al. A glucose meter interface for point-of-care gene circuit-based diagnostics. Nat. Commun. 12, 724 (2021).
Zhang, X. et al. Electrochemical assay to detect influenza viruses and measure drug susceptibility. Angew. Chem. Int. Ed. 54, 5929–5932 (2015).
Ahn, J. K., Kim, H. Y., Park, K. S. & Park, H. G. A personal glucose meter for label-free and washing-free biomolecular detection. Anal. Chem. 90, 11340–11343 (2018).
Singh, N. K. et al. Hitting the diagnostic sweet spot: point-of-care SARS-CoV-2 salivary antigen testing with an off-the-shelf glucometer. Biosens. Bioelectron. 180, 113111 (2021).
Rackus, D. G., Shamsi, M. H. & Wheeler, A. R. Electrochemistry, biosensors and microfluidics: a convergence of fields. Chem. Soc. Rev. 44, 5320–5340 (2015).
de Campos, R. P. S. et al. “Plug-n-Play” sensing with digital microfluidics. Anal. Chem. 91, 2506–2515 (2019).
Zhao, H. et al. Accessible detection of SARS-CoV-2 through molecular nanostructures and automated microfluidics. Biosens. Bioelectron. 194, 113629 (2021).
Gong, M. M. & Sinton, D. Turning the page: advancing paper-based microfluidics for broad diagnostic application. Chem. Rev. 117, 8447–8480 (2017).
Dungchai, W., Chailapakul, O. & Henry, C. S. Electrochemical detection for paper-based microfluidics. Anal. Chem. 81, 5821–5826 (2009).
Liu, H. & Crooks, R. M. Three-dimensional paper microfluidic devices assembled using the principles of origami. J. Am. Chem. Soc. 133, 17564–17566 (2011).
Liu, H., Xiang, Y., Lu, Y. & Crooks, R. M. Aptamer-based origami paper analytical device for electrochemical detection of adenosine. Angew. Chem. Int. Ed. 51, 6925–6928 (2012). This article reports a method to fabricate a self-powered origami paper analytical device with a simple digital multimetre for signal readout.
Chen, C. A. et al. An electricity- and instrument-free infectious disease sensor based on a 3D origami paper-based analytical device. Lab Chip 21, 1908–1915 (2021).
Su, J. et al. Smartphone-based electrochemical biosensors for directly detecting serum-derived exosomes and monitoring their secretion. Anal. Chem. 94, 3235–3244 (2022).
Guo, J. H. Smartphone-powered electrochemical biosensing dongle for emerging medical IoTs application. IEEE T. Ind. Inform. 14, 2592–2597 (2018).
Ainla, A. et al. Open-source potentiostat for wireless electrochemical detection with smartphones. Anal. Chem. 90, 6240–6246 (2018).
Kim, J., Campbell, A. S., de Avila, B. E. & Wang, J. Wearable biosensors for healthcare monitoring. Nat. Biotechnol. 37, 389–406 (2019). This review discusses the development of wearable biosensing systems for health-care monitoring, including their fundamental principles, prototypes and applications for different biological fluids.
Bariya, M., Nyein, H. Y. Y. & Javey, A. Wearable sweat sensors. Nat. Electron. 1, 160–171 (2018).
Park, J. et al. Soft, smart contact lenses with integrations of wireless circuits, glucose sensors, and displays. Sci. Adv. 4, eaap9841 (2018).
Moyer, J., Wilson, D., Finkelshtein, I., Wong, B. & Potts, R. Correlation between sweat glucose and blood glucose in subjects with diabetes. Diabetes Technol. Ther. 14, 398–402 (2012).
Baker, L. B. Physiology of sweat gland function: the roles of sweating and sweat composition in human health. Temperature 6, 211–259 (2019).
Emaminejad, S. et al. Autonomous sweat extraction and analysis applied to cystic fibrosis and glucose monitoring using a fully integrated wearable platform. Proc. Natl Acad. Sci. USA 114, 4625–4630 (2017).
Sonner, Z. et al. The microfluidics of the eccrine sweat gland, including biomarker partitioning, transport, and biosensing implications. Biomicrofluidics 9, 031301 (2015).
Lu, Y., Jiang, K., Chen, D. & Shen, G. Z. Wearable sweat monitoring system with integrated micro-supercapacitors. Nano Energy 58, 624–632 (2019).
Arakawa, T. et al. A wearable cellulose acetate-coated mouthguard biosensor for in vivo salivary glucose measurement. Anal. Chem. 92, 12201–12207 (2020).
Khalil, O. S. Noninvasive photonic-crystal material for sensing glucose in tears. Clin. Chem. 50, 2236–2237 (2004).
Gao, Y. et al. A flexible multiplexed immunosensor for point-of-care in situ wound monitoring. Sci. Adv. 7, eabg9614 (2021).
Teymourian, H. et al. Wearable electrochemical sensors for the monitoring and screening of drugs. ACS Sens. 5, 2679–2700 (2020).
Wang, M. Q. et al. A wearable electrochemical biosensor for the monitoring of metabolites and nutrients. Nat. Biomed. Eng. 6, 1225–1235 (2022).
Yu, Y. et al. All-printed soft human-machine interface for robotic physicochemical sensing. Sci. Robot. 7, eabn0495 (2022).
Quinton, P. M. Sweating and its disorders. Annu. Rev. Med. 34, 429–452 (1983).
Nyein, H. Y. Y. et al. A wearable patch for continuous analysis of thermoregulatory sweat at rest. Nat. Commun. 12, 1823 (2021).
Choi, J., Kang, D., Han, S., Kim, S. B. & Rogers, J. A. Thin, soft, skin-mounted microfluidic networks with capillary bursting valves for chrono-sampling of sweat. Adv. Healthc. Mater. 6, 1601355 (2017).
Lin, H. et al. A programmable epidermal microfluidic valving system for wearable biofluid management and contextual biomarker analysis. Nat. Commun. 11, 4405 (2020).
Manjakkal, L., Yin, L., Nathan, A., Wang, J. & Dahiya, R. Energy autonomous sweat-based wearable systems. Adv. Mater. 33, 2100899 (2021).
Chong, Y. W., Ismail, W., Ko, K. & Lee, C. Y. Energy harvesting for wearable devices: a review. IEEE Sens. J. 19, 9047–9062 (2019).
Lou, Z., Wang, L. L. & Shen, G. Z. Recent advances in smart wearable sensing systems. Adv. Mater. Technol. 3, 1800444 (2018).
Yang, P. et al. Monitoring the degree of comfort of shoes in-motion using triboelectric pressure sensors with an ultrawide detection range. ACS Nano 16, 4654–4665 (2022).
Yang, J. H. et al. Effect of garment design on piezoelectricity harvesting from joint movement. Smart Mater. Struct. 25, 035012 (2016).
Fu, K., Zhou, J., Wu, H. U. & Su, Z. Q. Fibrous self-powered sensor with high stretchability for physiological information monitoring. Nano Energy 88, 106258 (2021).
Hao, Y. et al. Self-rebound cambered triboelectric nanogenerator array for self-powered sensing in kinematic analytics. ACS Nano 16, 1271–1279 (2022).
Luo, X. X. et al. Tribovoltaic nanogenerators based on mxene-silicon heterojunctions for highly stable self-powered speed, displacement, tension, oscillation angle, and vibration sensors. Adv. Funct. Mater. 32, 2113149 (2022).
Song, Y. et al. Wireless battery-free wearable sweat sensor powered by human motion. Sci. Adv. 6, eaay9842 (2020).
Qin, Y. et al. Stretchable triboelectric self-powered sweat sensor fabricated from self-healing nanocellulose hydrogels. Adv. Funct. Mater. 32, 2201846 (2022).
Kim, J. et al. Wearable salivary uric acid mouthguard biosensor with integrated wireless electronics. Biosens. Bioelectron. 74, 1061–1068 (2015).
Jia, W., Valdes-Ramirez, G., Bandodkar, A. J., Windmiller, J. R. & Wang, J. Epidermal biofuel cells: energy harvesting from human perspiration. Angew. Chem. Int. Ed. 52, 7233–7236 (2013).
Falk, M., Andoralov, V., Silow, M., Toscano, M. D. & Shleev, S. Miniature biofuel cell as a potential power source for glucose-sensing contact lenses. Anal. Chem. 85, 6342–6348 (2013).
Huang, X. C. et al. Epidermal self-powered sweat sensors for glucose and lactate monitoring. Bio-Des. Manuf. 5, 201–209 (2022).
Yin, L. et al. A self-sustainable wearable multi-modular E-textile bioenergy microgrid system. Nat. Commun. 12, 1542 (2021).
Chen, Z., Xi, J., Huang, W. & Yuen, M. M. F. Stretchable conductive elastomer for wireless wearable communication applications. Sci. Rep. 7, 10958 (2017).
Takei, K. et al. Nanowire active-matrix circuitry for low-voltage macroscale artificial skin. Nat. Mater. 9, 821–826 (2010).
Nyein, H. Y. Y. et al. A wearable microfluidic sensing patch for dynamic sweat secretion analysis. ACS Sens. 3, 944–952 (2018).
Rose, D. P. et al. Adhesive RFID sensor patch for monitoring of sweat electrolytes. IEEE Trans. Biomed. Eng. 62, 1457–1465 (2015).
Keum, D. H. et al. Wireless smart contact lens for diabetic diagnosis and therapy. Sci. Adv. 6, eaba3252 (2020).
Lukocius, R., Vaitkunas, M., Virbalis, J. A., Dosinas, A. & Vegys, A. Physiological parameters monitoring system for occupational safety. Elektron. Elektrotech. 20, 57–60 (2014).
Lee, K. et al. Mechano-acoustic sensing of physiological processes and body motions via a soft wireless device placed at the suprasternal notch. Nat. Biomed. Eng. 4, 148–158 (2020).
Bujes-Garrido, J. & Arcos-Martínez, M. J. Development of a wearable electrochemical sensor for voltammetric determination of chloride ions. Sens. Actuators B Chem. 240, 224–228 (2017).
Vaddiraju, S., Burgess, D. J., Tomazos, I., Jain, F. C. & Papadimitrakopoulos, F. Technologies for continuous glucose monitoring: current problems and future promises. J. Diabetes Sci. Technol. 4, 1540–1562 (2010).
Zhang, J. et al. Wearable glucose monitoring and implantable drug delivery systems for diabetes management. Adv. Healthc. Mater. 10, 2100194 (2021).
Rodrigues, D. et al. Skin-integrated wearable systems and implantable biosensors: a comprehensive review. Biosensors 10, 79 (2020).
Bobrowski, T. & Schuhmann, W. Long-term implantable glucose biosensors. Curr. Opin. Electrochem. 10, 112–119 (2018).
Li, P. et al. From diagnosis to treatment: recent advances in patient-friendly biosensors and implantable devices. ACS Nano 15, 1960–2004 (2021).
Dalrymple, A. N. Implanted devices: the importance of both electrochemical performance and biological acceptance. Neural Regen. Res. 16, 1188–1189 (2021).
Kotanen, C. N., Moussy, F. G., Carrara, S. & Guiseppi-Elie, A. Implantable enzyme amperometric biosensors. Biosens. Bioelectron. 35, 14–26 (2012).
Li, C. M., Dong, H., Cao, X., Luong, J. H. & Zhang, X. Implantable electrochemical sensors for biomedical and clinical applications: progress, problems, and future possibilities. Curr. Med. Chem. 14, 937–951 (2007).
Wagner, J., Tennen, H. & Wolpert, H. Continuous glucose monitoring: a review for behavioral researchers. Psychosom. Med. 74, 356–365 (2012).
Xu, J. et al. Implantable platinum nanotree microelectrode with a battery-free electrochemical patch for peritoneal carcinomatosis monitoring. Biosens. Bioelectron. 185, 113265 (2021).
Singh, P. et al. Biomedical perspective of electrochemical nanobiosensor. Nanomicro Lett. 8, 193–203 (2016).
McGarraugh, G. The chemistry of commercial continuous glucose monitors. Diabetes Technol. Ther. 11, S17–S24 (2009).
Gross, T. M. et al. Performance evaluation of the MiniMed continuous glucose monitoring system during patient home use. Diabetes Technol. Ther. 2, 49–56 (2000).
Lee, H., Hong, Y. J., Baik, S., Hyeon, T. & Kim, D. H. Enzyme-based glucose sensor: from invasive to wearable device. Adv. Healthc. Mater. 7, 1701150 (2018).
Clark, J. J. et al. Chronic microsensors for longitudinal, subsecond dopamine detection in behaving animals. Nat. Methods 7, 126–129 (2010).
Tavakolian-Ardakani, Z., Hosu, O., Cristea, C., Mazloum-Ardakani, M. & Marrazza, G. Latest trends in electrochemical sensors for neurotransmitters: a review. Sensors 19, 2037 (2019).
Azzouz, A. et al. Nanomaterial-based electrochemical sensors for the detection of neurochemicals in biological matrices. Trends Anal. Chem. 110, 15–34 (2019).
Lei, L. J. et al. Nonenzymatic electrochemical sensor for wearable interstitial fluid glucose monitoring. Electroanalysis 34, 415–422 (2022).
Seaton, B. T. & Heien, M. L. Biocompatible reference electrodes to enhance chronic electrochemical signal fidelity in vivo. Anal. Bioanal. Chem. 413, 6689–6701 (2021).
Zhang, D. H. et al. Dealing with the foreign-body response to implanted biomaterials: strategies and applications of new materials. Adv. Funct. Mater. 31, 2007226 (2021).
Wickramasinghe, Y., Yang, Y. & Spencer, S. A. Current problems and potential techniques in in vivo glucose monitoring. J. Fluoresc. 14, 513–520 (2004).
Nichols, S. P., Koh, A., Storm, W. L., Shin, J. H. & Schoenfisch, M. H. Biocompatible materials for continuous glucose monitoring devices. Chem. Rev. 113, 2528–2549 (2013).
Malone-Povolny, M. J., Merricks, E. P., Wimsey, L. E., Nichols, T. C. & Schoenfisch, M. H. Long-term accurate continuous glucose biosensors via extended nitric oxide release. ACS Sens. 4, 3257–3264 (2019).
Hetrick, E. M. & Schoenfisch, M. H. Reducing implant-related infections: active release strategies. Chem. Soc. Rev. 35, 780–789 (2006).
Li, J. X. et al. A tissue-like neurotransmitter sensor for the brain and gut. Nature 606, 94–101 (2022). This article introduces a tissue-mimicking, stretchable, neurotransmitter sensor fabricated by laser patterning and demonstrates its application for in vivo real-time, multichannel and multiplexed monoamine sensing in the mouse brain.
Ben Amar, A., Kouki, A. B. & Cao, H. Power approaches for implantable medical devices. Sensors 15, 28889–28914 (2015).
Rebelo, R., Barbosa, A. I., Correlo, V. M. & Reis, R. L. An outlook on implantable biosensors for personalized medicine. Engineering 7, 1696–1699 (2021).
Yang, Y., Wei, X. J. & Liu, J. Suitability of a thermoelectric power generator for implantable medical electronic devices. J. Phys. D Appl. Phys. 40, 5790–5800 (2007).
Hwang, G. T. et al. Self-powered cardiac pacemaker enabled by flexible single crystalline PMN-PT piezoelectric energy harvester. Adv. Mater. 26, 4880–4887 (2014).
Zheng, Q. et al. In vivo powering of pacemaker by breathing-driven implanted triboelectric nanogenerator. Adv. Mater. 26, 5851–5856 (2014).
Simons, P., Schenk, S. A., Gysel, M. A., Olbrich, L. F. & Rupp, J. L. M. A ceramic-electrolyte glucose fuel cell for implantable electronics. Adv. Mater. 34, 2109075 (2022).
Scholten, K. & Meng, E. A review of implantable biosensors for closed-loop glucose control and other drug delivery applications. Int. J. Pharm. 544, 319–334 (2018).
Green, R. A., Lovell, N. H., Wallace, G. G. & Poole-Warren, L. A. Conducting polymers for neural interfaces: challenges in developing an effective long-term implant. Biomaterials 29, 3393–3399 (2008).
Kutner, N., Kunduru, K. R., Rizik, L. & Farah, S. Recent advances for improving functionality, biocompatibility, and longevity of implantable medical devices and deliverable drug delivery systems. Adv. Funct. Mater. 31, 2010929 (2021).
Tehrani, F. et al. An integrated wearable microneedle array for the continuous monitoring of multiple biomarkers in interstitial fluid. Nat. Biomed. Eng. 6, 1214–1224 (2022). This article reports the fabrication of a fully integrated prototype of a wearable sensor patch-based microneedle array and introduces its application for the wireless and continuous real-time sensing of two metabolites in the interstitial fluid.
Hsieh, K., Ferguson, B. S., Eisenstein, M., Plaxco, K. W. & Soh, H. T. Integrated electrochemical microsystems for genetic detection of pathogens at the point of care. Acc. Chem. Res. 48, 911–920 (2015).
Zhang, J., Lan, T. & Lu, Y. Translating in vitro diagnostics from centralized laboratories to point-of-care locations using commercially-available handheld meters. Trends Anal. Chem. 124, 115782 (2020).
Loncaric, C., Tang, Y. T., Ho, C., Parameswaran, M. A. & Yu, H. Z. A USB-based electrochemical biosensor prototype for point-of-care diagnosis. Sens. Actuators B Chem. 161, 908–913 (2012).
Tu, J. B., Torrente-Rodriguez, R. M., Wang, M. Q. & Gao, W. The era of digital health: a review of portable and wearable affinity biosensors. Adv. Funct. Mater. 30, 1906713 (2020).
Bariya, M. et al. Roll-to-roll gravure printed electrochemical sensors for wearable and medical devices. ACS Nano 12, 6978–6987 (2018). This article reports batch fabrication of flexible and robust electrode arrays by roll-to-roll gravure printing for a range of electrochemical sensing applications.
Tian, L. et al. Large-area MRI-compatible epidermal electronic interfaces for prosthetic control and cognitive monitoring. Nat. Biomed. Eng. 3, 194–205 (2019). This article reports materials, device structures, handing and mounting methods, and manufacturing approaches for the fabrication of large-area epidermal electronic interfaces.
Gordon, W. J. & Stern, A. D. Challenges and opportunities in software-driven medical devices. Nat. Biomed. Eng. 3, 493–497 (2019).
Liu, H. & Zhao, C. Wearable electrochemical sensors for noninvasive monitoring of health-a perspective. Curr. Opin. Electrochem. 23, 42–46 (2020).
Dixon, A. M., Allstot, E. G., Gangopadhyay, D. & Allstot, D. J. Compressed sensing system considerations for ECG and EMG wireless biosensors. IEEE Trans. Biomed. Circuits Syst. 6, 156–166 (2012).
Koh, A. et al. A soft, wearable microfluidic device for the capture, storage, and colorimetric sensing of sweat. Sci. Transl Med. 8, 366ra165 (2016).
Kamei, K. et al. 3D printing of soft lithography mold for rapid production of polydimethylsiloxane-based microfluidic devices for cell stimulation with concentration gradients. Biomed. Microdevices 17, 36 (2015).
Martin, A. et al. Epidermal microfluidic electrochemical detection system: enhanced sweat sampling and metabolite detection. ACS Sens. 2, 1860–1868 (2017).
Acknowledgements
The authors gratefully thank the National Natural Science Foundation of China (21827812, 21890741), the Science and Technology Project of Nanjing City (202110023) and the Independent Research Foundation from the State Key Laboratory of Analytical Chemistry for Life Science (5431ZZXM2006) for start-up supply. The authors are also grateful to Y. Lu in Fasteur Biotechnology for market information, to Q. Yu, Y.C. Chen and L.J. Lei for helpful comments.
Author information
Authors and Affiliations
Contributions
J.W., H.L. and H.X.J. arranged the sections of the Review. J.W., W.W.C. and H.X.J. wrote the introduction and the section on electrochemical biosensing of disease biomarkers, and H.L., B.M and H.X.J. wrote the sections on portable electrochemical biosensing devices, integration into wearable devices and integration into implantable devices. All authors discussed the outlook section and display items.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Bioengineering thanks Onur Parlak, Chung Chiun Liu, and Susana Campuzano for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wu, J., Liu, H., Chen, W. et al. Device integration of electrochemical biosensors. Nat Rev Bioeng 1, 346–360 (2023). https://doi.org/10.1038/s44222-023-00032-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s44222-023-00032-w
This article is cited by
-
An interfacial robust and entire self-healing ionogel-elastomer hybrid for elastic electronics enables discretionary assembly and reconfiguration
Science China Chemistry (2024)
-
State of the art and future research directions of materials science applied to electrochemical biosensor developments
Analytical and Bioanalytical Chemistry (2024)
-
Biosensor-Based Nanodiagnosis of Carcinoembryonic Antigen (CEA): an Approach to Classification and Precise Detection of Cancer Biomarker
BioNanoScience (2024)
-
Self-assembling biomolecules for biosensor applications
Biomaterials Research (2023)
-
Wearable flexible microfluidic sensing technologies
Nature Reviews Bioengineering (2023)