Abstract
The detection of pathogenic bacteria is essential to prevent and treat infections and to provide food security. Current gold-standard detection techniques, such as culture-based assays and polymerase chain reaction, are time-consuming and require centralized laboratories. Therefore, efforts have focused on developing point-of-care devices that are fast, cheap, portable and do not require specialized training. Paper-based analytical devices meet these criteria and are particularly suitable to deployment in low-resource settings. In this Review, we highlight paper-based analytical devices with substantial point-of-care applicability for bacteria detection and discuss challenges and opportunities for future development.
Similar content being viewed by others
Introduction
Despite usually being associated with infections, the majority of bacteria are harmless and perform vital functions in humans, animals, plants and the environment1. It is estimated that less than 1% of all bacteria are responsible for diseases2; however, they have a substantial impact on public health. The World Health Organization (WHO) estimates that 600 million people become ill every year after consuming unsafe food, most of which are caused by pathogenic bacteria, resulting in 420,000 deaths worldwide. Lower-respiratory-tract infections and diarrhoeal illnesses are among the top 10 global causes of death in 2019 and are often caused by bacteria. Bacterial infections are generally treated with antibiotics, which has led to one of the greatest threats to global health and food safety, that is, antimicrobial resistance3. It has been estimated that 4.95 million people died from illnesses associated with antimicrobial resistance in 2019 (refs. 4,5). Low-income regions, such as western sub-Saharan Africa, have reported the highest rates of deaths (27.3 per 100,000 people), whereas Australasia reported the lowest rate (6.5 deaths per 100,000 people). These high mortality rates in low-income countries have been associated with inadequate diagnostics tools6, highlighting the need for devices that can accessibly and accurately identify the cause of a disease, thereby decreasing the burden of infection in the developing world7.
In addition to the enzyme-linked immunosorbent assay (ELISA), polymerase chain reaction (PCR) and conventional culture-based assays8,9,10, common pathogen detection methods include biochemical techniques11, instrumental-based approaches, such as flow cytometry and gas chromatography12,13, as well as spectroscopy-based techniques, such as Fourier transform infrared spectroscopy (FTIR) and Raman spectroscopy14,15. Despite being accurate, robust and sensitive down to the single-cell level16, these techniques are costly and time-consuming (hours to days), requiring centralized laboratories, trained personnel, sample pre-treatment and multi-step processing. To overcome these issues, the WHO outlined a set of criteria, known as ASSURED, for an ideal diagnostics test in low-resource settings. Briefly, it needs to be affordable, sensitive, specific, user-friendly, rapid, equipment-free and deliverable17. With the recent advent of digital technologies and tele-health, the criteria were revised to include two additional characteristics: real-time connectivity and ease of specimen collection, leading to the new REASSURED benchmark18. In addition, point-of-care (POC) diagnostics should be able to analyse small volumes, be portable and disposable (owing to the hazardous nature of the sample), with few processing steps and minimal sample preparation. Importantly, they need to perform effectively in different environmental conditions without requiring a power source, and operate in the relevant (clinical and practical) concentration range19. Paper-based platforms, such as conventional immunochromatographic strips combined with immunoassays20, are excellent POC diagnostic candidates, because they meet several of the REASSURED criteria. Owing to paper’s abundance, disposability and, most importantly, low cost, paper-based sensors have long been used in various formats to detect pH, proteins and nucleic acids21,22 (Fig. 1). Moreover, paper is a versatile material that can be manufactured at large scale23; signal visibility can be tuned by paper thickness22; its white colour provides strong contrast for colorimetric platforms; and it is flexible, biocompatible and easy to transport and store. Therefore, paper-based sensors are widely used in clinical, food and environmental diagnostics24,25.
In this Review, we discuss paper-based platforms for bacteria detection, excluding other microbial pathogens such as viruses, parasites and fungi. Importantly, only studies in the fields of health diagnostics, food quality control and environmental monitoring that currently satisfy (or closely satisfy) the following criteria have been included: the sensor can evaluate untreated and unprocessed samples26, fulfils the REASSURED requirements for field-deployable POC diagnostics in low-resource settings and achieves a limit of detection (LOD) within the relevant practical range. For the latter criteria, a major focus will be placed on studies that achieve low LODs of <102 colony-forming units (CFU) ml–1. We conclude with the major challenges faced by paper-based platforms.
Paper-based sensing platforms
An important feature of paper-based sensors is that they can spontaneously transport liquid via capillary flow and, therefore, do not require pumps. In addition, the pore size of paper can easily be tuned to change the flow rate, and paper has a high surface-to-volume ratio, which allows for reagent immobilization and storage. The most popular paper-based platforms are colorimetric-based lateral flow assays (LFAs) (Fig. 2). Generally, LFAs consist of a sample pad, a conjugate pad, a detection pad and an absorbent pad. For a standard immune sandwich assay, the sample is first introduced onto the sample pad to initiate the absorption process. The sample then migrates towards the conjugate pad, where it interacts with labelled detection bioreceptors, usually nanoparticle-conjugated antibodies. Upon further migration, the sample reaches the detection pad, which contains a test line, where captured bioreceptors bind to the labelled analyte, and a control line. Finally, the absorbent pad absorbs the excess sample and dictates the volume of sample that the test requires. Microfluidic paper-based analytical devices follow a similar mechanism and benefit from design simplicity, low cost and a similar rapid response time of 5–30 minutes depending on the sample and application27,28. By contrast, despite comparable sensitivity, electrochemical-based techniques have seen a decline in research, probably owing to higher costs29,30. Different analytical methods are used to detect the response signal of paper-based platforms, including colorimetry, electrochemistry and luminescence (Table 1). Colorimetry is the most widely used technique, because it provides simple and portable operation, with good stability and low cost31. The majority of existing commercial kits require equipment and several consumables, such as media, agar and culture flasks. However, a number of companies and start-ups have developed bacteria detection kits that better satisfy the REASSURED criteria (Table 2). Interestingly, all these kits are colorimetric LFA-based assays, which, instead of detecting entire bacteria, detect their byproducts or metabolites (Fig. 3).
Paper-based analytical devices (PADs) on the market typically consist of a sample pad, a conjugate pad containing antibodies tagged with colour-generating materials, a membrane to induce capillary flow of the sample, an absorbent pad to capture excess sample and a laminated card to mount the membrane for structural rigidity. A sample containing the target analyte is introduced to the sample pad. In the presence of analytes, the antibody-conjugated tags specifically bind to the analyte. As the sample passes the test line, the antigens bind to the bioreceptors to form a sandwich structure, which subsequently changes the colour of the test line. The remaining conjugated antibodies bind to the bioreceptors in the control line and the excess sample is absorbed into the absorbent pad. In the absence of a target analyte, all antibody-conjugated tags accumulate in the control line, resulting in a single line that denotes a negative test. LFA, lateral flow assay.
a, Bacteria detection in paper-based sensors includes sampling, treatment, detection and signal output. Depending on the nature of the sample and the detection technique, different pre-treatment options are required. For example, solid-based samples require homogenization, centrifugation or dilution. Liquid-based samples require dilution to reduce the effect of complex media on the recognition element, although pre-treatment is becoming less common. Gaseous samples generally require a pre-concentration step because of the low concentration of analytes. Bacteria detection can be conducted either directly or indirectly. The former involves conjugating the bacteria with enzyme-tagged antibodies, which are then exposed to the paper-based substrate containing the corresponding substrate. The latter involves detecting byproducts or metabolites that indicate the presence or absence of the target bacteria. Nanoparticles and enzyme–substrate interactions convert bacteria detection into a measurable event, which can be detected using various analytical methods, including colorimetry, electrochemistry or luminescence. b, In a chromogenic array, volatile organic compounds (VOCs) emitted by microorganisms are exposed to a paper chromogenic array containing chromogenic dyes and dye combinations undergoing bacteria strain-specific colour changes. In immunomagnetic separation, magnetic beads are introduced into bacteria-containing samples to capture bacteria. The magnetic bead–bacteria complex is then separated using an external magnetic field and conjugated with horseradish peroxidase (HRP)-tagged antibodies (Ab). The complex is then exposed to paper disks containing pre-dried 3,3′,5,5′-tetramethylbenzidine (TMB, a substrate for HRP), producing a blue colour. In DNAzyme-based lateral flow assay (LFA), a bacteria-containing sample is introduced to the sensor zone, which activates an urease-containing DNAzyme, leading to the cleavage of the latter. Running buffer carries the released urease to the detection zone, causing a pH change and a resulting colour change. In a bacteria–particle aggregation pattern, peptides covalently conjugated to polystyrene particles aggregate to different degrees when exposed to specific bacterial suspensions. The resulting change in liquid surface tension and viscosity alters the flow velocity, leading to unique profiles for each bacterial species.
We note that different applications require distinct sampling methods (destructive or non-destructive), quality assurance and industrial standards. In solid food samples, for example, pathogens are not evenly distributed as in liquid specimens. Here, studies that closely satisfy the criteria of using unprocessed samples, POC applicability and demonstrating relevant LODs, are grouped according to the state of the specimen, that is, solid, aqueous and gaseous. Applications will range from clinical diagnosis to pathogen surveillance in food and the environment (Fig. 3).
Solid-based samples
Paper-based platforms for bacteria detection in solid samples (such as beef32, seafood33, bread34 and lettuce35) are mostly colorimetric-based LFAs36,37,38,39. These sensors are user-friendly and suitable for POC applications in low-resource settings. Several platforms have been designed based on LFAs in conjunction with amplification techniques, such as PCR40, surface enhanced Raman spectroscopy41 or immunomagnetic separation for bacteria detection42,43,44. Other approaches that use loop mediated isothermal amplification (LAMP) or paper-based ELISA have also been developed45,46,47. However, they require heating, centralized laboratories, and several processing steps and, despite the greater complexity, the sensitivity of these systems is not substantially lower than simpler alternatives (102–104 CFU ml–1). Although CRISPR–Cas paper-based assays for bacterial detection benefit from low LODs in solid-based samples (~1–102 CFU ml–1), they require recombinase polymerase amplification or recombinase-assisted amplification48,49. These steps take place at 37–42 °C, which is closer to room temperature compared to the 60 °C of LAMP; however, a power source is still required50,51. Moreover, amplification components (such as Cas proteins and primers) need to be stored at well below freezing temperature (–20 °C), meaning that LAMP- and CRISPR-based approaches, in their current state, do not meet all the REASSURED criteria (Boxes 1,2).
Colorimetric detection
Colorimetric sensors for pathogen detection have mainly suffered from high LODs (>104 CFU ml–1) when dealing with untreated or unprocessed samples52. Furthermore, complex food matrices are known to hinder colour development53. Consequently, techniques such as magnetic separation have been proposed to capture and concentrate target bacteria and improve signal readability54,55. For example, negatively charged Escherichia coli O157:H7 can be separated from sausage samples using positively charged magnetic beads under an external magnetic field. The bacteria–magnetic bead complex is conjugated to horseradish peroxidase (HRP)-tagged anti-E. coli O157:H7 antibodies, which, after being exposed to paper disks containing pre-dried 3,3′,5,5′-tetramethylbenzidine (TMB, a substrate for HRP), produces a blue colour (Fig. 3b). The entire process results in a LOD of 30 CFU ml–1 within 50 minutes56. However, long-term storage of the different assay components was not evaluated. In addition, this system requires substantial user interference and refrigerated storage of the nanoparticles.
Instead of directly detecting bacteria, specific biomarkers released by bacteria can be detected, including toxins57 or proteases58. For example, exposing a paper strip containing magnetic nanobead–peptide probes integrated with a gold sensing platform to Staphylococcus aureus-contaminated samples results in peptide cleavage by proteases and dissociation of the magnetic nanobeads from the sensor surface59. The exposed gold sensing platform enables qualitative detection of bacteria in pure broth culture, inoculated food products (ground beef, turkey sausage, lettuce and milk) and environmental samples (dust), resulting in LODs of 7, 40 and 100 CFU ml–1, respectively. The advantages of this assay is that it is label-free, cost-effective, rapid (within minutes), simple, suitable for other types of bacteria60, and stable for 6 months if refrigerated. However, the colours manifested are heterogeneous, and minor sample pre-treatment and refrigeration are needed.
Pathogens can also be identified by detecting emitted volatile organic compounds (VOCs)61,62,63. For example, a paper chromogenic array containing 23 chromogenic dyes and dye combinations undergo a colour change when exposed to VOCs from E. coli and Listeria monocytogenes in fresh-cut romaine lettuce64 (Fig. 3b). Furthermore, the colour changes can be digitalized to train a multi-layer neural network allowing automatic, high-throughput, accurate, non-destructive and strain-specific pathogen detection in food samples. This assay is cheap (<US$0.1), does not require enrichment, culturing, incubation or sample-preparation steps, and is thus highly attractive for POC applications. In addition, it also performs against background microflora65. This is important because VOCs can also be emitted by food products and non-pathogenic microorganisms. The potential of this platform to continuously and non-destructively monitor food samples throughout their lifecycle makes it a promising smart packaging material to prevent foodborne disease outbreaks.
Colorimetric paper-based sensors to detect bacteria in solid samples have also been developed for biomedical applications. For example, stool samples containing Helicobacter pylori can be exposed to LFA-based sensors with urease-containing DNAzymes immobilized on their surface. Exposure to the pathogen activates the DNAzyme, which in turn releases urease, causing a pH increase and consequently a colour change66 (Fig. 3b). This approach is highly selective against other bacterial species including H. pylori, E. coli, Clostridium difficile, L. monocytogenes, Bacillus subtilis, Salmonella typhimurium, Klebsiella pneumoniae, Fusobacterium nucleatum and Pseudomonas aeruginosa, resulting in a LOD of 104 CFU ml–1, which is within the clinically relevant range for stool samples. Furthermore, this system can detect H. pylori in 1 hour, with little user interference, minor sample pre-treatment and no loss of performance after 4 months of storage at room temperature in the dark — all highly attractive qualities for POC applications.
Other detection strategies
Bacteria-detection strategies in solid samples based on fluorescence, electrochemistry and chemiluminescence are currently not as field-deployable as colorimetric-based sensors because they require trained users, complex and expensive equipment, numerous processing steps and have comparatively higher LODs. For example, a fluorescent-based sandwich lateral flow immunoassay can detect E. coli O157:H7 in bread, milk and jelly at a visual LOD of 105 CFU ml–1, which can be decreased to 104 CFU ml–1 using a scanning reader67. Furthermore, pre-incubation of the food sample in broth for 8–10 hours results in a substantially improved LOD of 1 CFU ml–1. The assay is specific when tested against two other E. coli O157:H7 strains and 23 other foodborne strains and shows no decrease in detection performance after 20 weeks in the fridge. Fluorescent-based system can also be integrated with LAMP to improve visual LODs, as shown for shrimp68 and salmon69 samples. However, these techniques require specialized equipment (a heating source, for example) with several processing steps involved, and are therefore not suitable for low-resource settings.
An electrochemical example involves an impedimetric immunosensor based on gold nanoparticles grown on a modified graphene paper for label-free detection of E. coli O157:H770. Briefly, to quantitatively determine the LOD, Nyquist plots for different concentrations of E. coli O157:H7 are recorded. An increase in the semicircle diameters of the impedance spectra is observed after exposing ground beef and cucumber samples to increasing pathogen concentrations, resulting in LODs of 1.5 × 104 and 1.5 × 103 CFU ml–1, respectively. The immunosensor maintains stable performance for at least a month when refrigerated, and shows specificity against E. coli DH 5α, S. aureus and L. monocytogenes; however, the assay requires expensive instruments and is not portable.
To improve the sensitivity of DNA quantification techniques, chemiluminescence-based approaches have been developed71. For example, exposing Campylobacter spp. DNA, extracted from a chicken sample and immobilized onto a paper membrane, to biotinylated silica-nanoparticles, results in sample hybridization. This process can be detected using streptavidin conjugated to horseradish peroxidase (HRP) in the presence of luminol and H2O2. However, sample pre-treatment for DNA extraction, substantial user interference, lengthy procedure (24 h) and numerous processing steps, make this approach unsuitable for POC applications.
Aqueous-based samples
Similar to solid-based samples, bacteria in aqueous-based samples, such as serum72, milk73, water74,75, juice76 and powder infant formula77,78, are primarily detected using LFA-based colorimetric assays owing to their simplicity79,80,81. The majority of these assays rely on gold nanoparticles as signal probes82,83 but they are limited by high LODs84 (>103 CFU ml–1) or require sample pre-treatment85. To improve their performance, LFA-based assays have been integrated with amplification methods86 such as magnetic nanoparticles to allow for target analyte pre-concentration87,88, chromogenic substances89,90,91,92, enzymes93,94,95 or by implementing PCR96, LAMP97 or CRISPR–Cas-based approaches98,99. However, all these approaches suffer from one or more of the following limitations, including high temperatures100,101, long response times102, low sensitivity103, substantial sample preparation98,99 and amplification steps104,105,106,107.
Colorimetric detection
Paper-based colorimetric sensors commonly use antibody-conjugated gold nanoparticles for biomarker detection108. For example, an LFA-based nitrocellulose dipstick immunoassay with this design can detect Vibrio parahaemolyticus, a bacterial pathogen in oyster circulatory fluid, with a LOD of 4.66 × 105 CFU ml−1 in approximately 2 hours, which is below the infectious dose (ID50) of V. parahaemolyticus109. Although this system is robust, specific and does not require bacteria culture, it is limited by substantial user intervention and a lack of stability evaluation.
A similar colorimetric sandwich immunoassay uses immunomagnetic separation to detect Salmonella in milk and bird faeces110. A well-array format and ‘chemometer’ approach enable qualitative demonstration of the assay’s performance. For the former, wax printing is used to produce each well, which, upon exposure to increasing concentrations of the target pathogen, leads to distinct colour changes. For the latter, the length of the colour strip developed along the paper channel is proportional to the bacteria concentration, analogous to a thermometer. Detection relies on immunomagnetic separation to clean the sample and an enzymatic reaction that cleaves chlorophenol red-β-d-galactopyranoside to chlorophenol red, producing a yellow-to-red colour change. Building on this design, a reusable 3D-printed rotational manifold coupled with disposable paper-based layers allows semi-automated reagent delivery, washing and detection111. This device can specifically detect Salmonella with a LOD of 440 and 640 CFU ml–1 in growth media and milk samples, respectively. Importantly, to reduce user intervention, biotin-labelled Salmonella antibodies and streptavidin-conjugated β-galactosidase can be added and dried within reagent channels before running the assay. Although no long-term stability evaluation was reported on the pre-dried components, this sensitive assay shows great promise for POC applications, detecting the target analyte within 65 minutes. In addition, the manifold allows pipette-free reagent delivery and washing steps.
Paper-based colorimetric assays can also be designed to detect the VOCs of bacteria in aqueous solutions using metallic nanoparticles deposited on paper112,113,114. Here, the composition of the volatile metabolome of bacteria strains can be distinguished by the unique coloured pattern produced. This sensor can achieve LODs of 88, 94, 89 and 92 CFU ml–1 for S. aureus, L. monocytogenes, E. coli and Proteus mirabilis in spiked water samples, respectively112. Importantly, the same design can detect bacteria-specific urinary tract infections for 300 urine samples collected from volunteers with 100% accuracy when subjected to exploratory data analysis methods including principal component analysis and hierarchical cluster analysis (HCA). This approach does not require sample preparation and has a response time of less than 50 min for bacteria discrimination in human urine. Furthermore, it has a stable response even after 2.5 months of storage in a desiccator. However, the main limitation is the use of 37 °C incubators, which are needed to generate optimal VOC release from bacteria.
Fluorescent detection
Although not as popular as colorimetric-based platforms, several fluorescent-based assays with POC applicability for bacteria detection in aqueous samples have been developed115,116,117,118,119,120,121,122,123,124,125,126. For example, a paper-based fluorometric assay consisting of an array of six areas containing gold or copper nanoclusters, modified with pepsin, trypsin, ovalbumin and glutathione, can detect sepsis-causing bacteria within 15 seconds127. Specifically, upon exposure to human serum, each sensor element exhibits different quenching responses to the various targets, creating an exclusive pattern for each analyte after ultraviolet light irradiation. The fluorescence emission can be recorded using a smartphone, resulting in LODs of 43.0, 63.5, 26.0 and 47.0 CFU ml–1 for S. aureus, Streptococcus pyogenes, E. coli and P. aeruginosa, respectively. Furthermore, when tested on individuals suspected of having sepsis, the sensor detected 35 out of 40 infected samples, highlighting its accuracy. Although this device requires a dark-cabinet, an ultraviolet lamp and shows a gradual signal quenching after 25 days of storage, it does not require sample preparation.
Bacteria can also be sensitively detected through interaction of their enzymes with chromogenic substrates, as shown for E. coli128, L. monocytogenes129 and Cronobacter130. However, long pre-enrichment times (4–8 h) are required because of the low concentration of enzymes produced by bacteria. Combining immunomagnetic separation with enzyme-based signal amplification131,132 can overcome this issue; however, these methods suffer from high costs and short shelf-life owing to the low stability of enzymes. A method relying on immunomagnetic separation coupled with nanoparticle dissolution-triggered signal amplification can address these challenges133. In this case, E. coli O157:H7 from spiked milk samples are extracted using antibody-labelled immunomagnetic beads, which are labelled with silver nanoparticles, forming a sandwich structure. The addition of hydrogen peroxide (H2O2) causes the release of silver ions (Ag+), which results in signal amplification. Finally, inserting a quantum dot paper strip into the solution pushes the released ions to flow through capillary action, which quenches the fluorescence signal owing to the cation exchange reaction between Ag+ and the quantum dots. Exposure of the treated strip to ultraviolet light reveals the height of the quenched fluorescent band, which correlates with the concentration of the target bacteria. Here, the naked-eye LOD is 500 CFU ml–1 in spiked milk samples, which is lower than other fluorescent LFAs that use immunomagnetic separation (103–104 CFU ml–1)134,135. Moreover, this method is bacteria-specific; when evaluated against other strains, such as E. coli DH5α, S. typhimurium, L. monocytogenes and S. aureus, no quenching was observed. Although fast (15 min upon introduction of the quantum dot strip) and sensitive, this sensor is not portable, requires many processing steps and lacks a stability evaluation for the different components.
Electrochemical detection
Electrochemical methods for bacteria detection in aqueous food samples typically require dilution to reduce the media effect136, several processing steps137 and suffer from decreasing performance after long-term storage (>4 weeks)138. To overcome these issues, a disposable impedimetric sensor has been designed, consisting of two silver electrodes deposited on filter paper, and a polyaniline coating functionalized with glutaraldehyde. This sensor can detect total bacterial colonies in water samples139. The aldehyde groups on the sensor bind to the amine groups on bacterial walls, which results in a change in dielectric constant and therefore a capacitive effect between the electrodes. Moreover, bacterial metabolism affects medium conductivity, which leads to changes in medium resistance. These two effects can be measured using a frequency response analyser, which allows E. coli and P. aeruginosa detection in tap and grey water with LODs of 500 and 1,000 CFU ml–1, respectively. This assay does not rely on biological molecules, such as antibodies140,141, and is therefore less expensive and more stable. Furthermore, it is fast (20 min), user friendly, disposable and requires little sample pre-treatment. However, this sensor does not include specific receptors, and therefore detects any kind of Gram-positive or Gram-negative bacteria. To improve specificity, a similar label-free paper-based impedimetric sensor has been developed using a screen-printed graphene surface modified with graphene oxide and functionalized with lectin Concanavalin A (ConA)142. This assay demonstrates specific binding to mono- and oligosaccharides of E. coli (tested against Salmonella sp. and L. monocytogenes) in synthetic wastewater at a LOD of 10 CFU ml–1. Importantly, this low sensitivity is achieved without using chemical amplifications, such as PCR, and thus, the sensor does not require expensive equipment.
Other detection strategies
Photoluminescence143 or chemiluminescence144 paper-based sensors have also been used to detect bacteria in aqueous solutions. These sensors show high sensitivity (100 CFU ml–1 and 102–103 spores ml–1, respectively) and specificity, and require little to no sample pre-treatment; however, they need expensive instrumentation and have stability issues. Alternatively, glucose meters can be used to quantitatively detect bacteria in milk samples with low LOD (79 CFU mL–1), but are not yet suitable for POC applications due to their low mean recovery (87.5%)145,146. Instead, thread-based147 and distance-based assays148 can be applied for bacteria detection. For the former, textile-based microfluidic devices use cotton, silk or polyester–acrylic fibres rather than nitrocellulose paper to construct fluidic channels. Similar to paper, they are highly available, low-cost (<US$1), biodegradable and rely on capillary flow for fluid movement, but they have a higher mechanical strength, thereby avoiding the brittleness of wet LFA strips149. They have been used for bacteria detection in milk, juice and lettuce with medium-to-low LODs of 1,000, 1,000 and 5,000 CFU ml–1, respectively147.
Detection with distance-based devices relies on measuring the length of a colour developed after applying the sample of interest to a PAD. The length travelled is proportional to the concentration of the target analyte and can easily be measured with a ruler. This means they can provide a quantitative response in contrast to the semi-quantitative response of thread-based approaches150. This method can be further improved using smartphones. For example, a smartphone-based paper microfluidic device can be designed based on six different peptides sets covalently conjugated to polystyrene particles151. Loading the paper microfluidic chips with bacterial suspensions (E. coli K12, S. aureus, Salmonella enterica, Enterococcus faecium and P. aeruginosa) causes particle aggregation, which leads to alterations of surface tension and viscosity of the liquid, thereby affecting flow velocity. The latter is captured using a smartphone camera, generating unique profiles for each bacterial species, which are then classified using a support vector machine. This device allows bacterial species classification151 (Fig. 3b), functions entirely in a handheld manner and is not affected by light, humidity or temperature conditions. Furthermore, as opposed to antibodies, the peptide receptors make the device inherently more stable for long-term storage without compromising specificity. When tested on complex field water samples, the device detected E. coli and Salmonella at low concentrations of 220 and 33 CFU ml–1, respectively, highlighting its potential for POC applications. The growing smartphone market has been similarly exploited in mobile-phone-integrated colorimetric bacteria detection based on Mie scattering in urine152. This technique analyses photodiode readings at different detection and light angles, with the scatter being dependent on particle size, morphology, refractive index and concentration. Bacterial growth influences these factors, resulting in changes in scatter patterns153. Using this approach on urine samples, a LOD of 10 CFU ml–1 for E. coli and Neisseria gonorrhoeae can be obtained within 30 seconds, which is substantially lower compared to commercially available LFAs and nitrite strips (106 CFU ml–1).
Gaseous-based samples
Bacteria can also be found in air suspensions, known as bioaerosols. Because of the nature of the sample, assays typically consist of two main steps: collection and detection. Collection can be achieved by sedimentation, filtration, centrifugation, impaction, impingement or microfluidic chips154. For example, air samples with airborne bacteria can be passed through a porous sampling pad on a paper-based device155,156. The collected bacteria are then lysed using a dried lysis buffer on the sampling pad, releasing DNA molecules, which are then transported through water-mediated lateral flow to a binding pad. One limitation of this assay is that the resulting aliquot needs to be analysed using quantitative real-time PCR. Similarly, a paper-based sensor can be based on adenosine triphosphate (ATP)-driven luciferase d-luciferin photoemission157. Here, aerosolized E. coli samples, some of which include dust to simulate air environmental conditions, are concentrated, lysed and dropped onto paper disks to evaluate bioluminescence intensity. Using this approach, the extracted ATP can be detected at LODs as low as 1.17 × 103 CFU ml–1 in pure bacteria samples and 2.32 × 103 CFU ml–1 in bacteria samples containing dust (1 mg ml–1) in less than 10 minutes. Importantly, paper disks can be stored for up to 30 days at room temperature with negligible loss in performance. However, this device requires an energy source for lysis, expensive equipment for signal detection, several processing steps, experienced user interference and has low portability. Moreover, this model relies on ATP detection, which lacks selectivity and therefore can be used only for bacteria detection and not for identification.
To improve specificity, a label-free paper-based electrochemical sensor was fabricated using stencil-printed carbon paste for the working and counter electrodes, and Ag–AgCl for the reference electrode158. High-affinity B. subtilis spore-specific peptides were immobilized on the carbon paste electrode as the recognition element. The increased resistance to electron transfer caused by the interaction between the peptides and the bacteria spores correlates with increasing spore concentration. Using a differential pulse voltammetry technique, concentrations as low as 6.9 × 102 CFU ml–1 can be detected in 30 min with negligible decrease in performance after 4 weeks of refrigerated storage. However, this sensor is limited by the need for expensive equipment, trained personnel and lack of portability.
Outlook
The simplicity and low cost of paper-based analytical platforms have led to a plethora of studies on bacteria detection. The majority of these devices use colorimetry as the analytical technique, compared to electrochemistry, fluorescence or chemiluminescence methods. Such paper-based diagnostic tools have great potential for POC applicability, but several key challenges remain to be addressed in order to satisfy the REASSURED criteria. In particular, the LOD needs to be improved, taking into account specific bacteria and applications. Selectivity can be addressed by including interference experiments against target compounds often present in the sample; for example, for clinical diagnostics, the background microbiome and serum proteins should be used as control. In food samples, amino acids, proteins and fatty acids interfere with measurements, whereas in agriculture, soil and plant proteins can affect the assay. Moreover, most studies typically evaluate the selectivity of their platforms against other pathogenic bacteria. It is also important to assess selectivity at the level of the genus or strain to reduce false-positive results. Evolution of bacteria in response to environmental or physical stress can lead to changes to their phenotypic state or metabolic activity159,160. Therefore, future studies, particularly those relying on metabolically released byproducts like VOCs and antimicrobial-resistant strains, must be regularly calibrated to account for these variations and to avoid detection errors. In addition, to ensure the accuracy of measurements, protein levels, viscosity and pH need to be accounted for.
In this Review, we have not discussed studies that evaluated assaying with pristine samples, for example, pure bacteria in simple matrices, such as distilled water. Considering the great disparity between the number of field- and laboratory-tested POC platforms161, data on sensor performance to detect bacteria in their native conditions is essential to promote commercialization and encourage industry investment.
The requirement of sample pre-treatment substantially limits POC applicability. Future research should focus on the development of platforms that either do not require this step or that integrate sample treatment in the assay162. Furthermore, methods relying on DNA amplification are limited in their ability to differentiate between viable and nonviable cells130. An additional confounding factor is that, when exposed to stressful conditions, bacteria can enter a survival mode, in which they do not grow on routine culture media but are still alive and capable of resuming metabolic activity163. Furthermore, assays which require an amplification step, such as CRISPR–Cas systems, need an additional power source. Self-powered sensors that generate energy sustainably rather than requiring a power grid or batteries could help increase their POC applicability164. Enzymatic fuel cells, for example, have shown great promise by using redox enzymes to convert chemical energy stored in biomolecules to electrical energy, with fluctuations translating to output current changes. These devices can operate as self-powered amperometric sensors for target biomarkers using elements within the sample as fuel165. Even isothermal amplification methods, such as nucleic-acid-sequence-based amplification, LAMP, recombinase polymerase amplification or recombinase-assisted amplification, currently suffer from false-positive tendencies. In addition, they are insensitive to mutations, have limited amplification length, complex primer design and reaction composition, and they require refrigerated storage of reaction elements104. Importantly, although amplification-free CRISPR–Cas systems have been developed, they have been used mainly for virus detection166,167 thus far or are not paper-based168 and, therefore, outside the scope of this Review. This technology could also be adapted to detect bacteria.
In addition to these essential improvements, paper-based POC diagnostics should ideally be able to detect multiple compounds. However, platforms that depend on recognition elements, such as antibodies, enzymes and aptamers, are costly, complex and not as robust. Moreover, not all microbial species and strains are known when testing a sample, complicating the choice of the proper recognition element.
Choosing the proper paper material is another important parameter to consider, which depends on the volume and size of the analyte being detected169. For example, for micrometre-sized analytes (bacteria and cells), high-bed-volume materials, such as cellulose fibres (≥250 µm), should be used to facilitate flow of the analyte and buffer. Compared to low-bed-volume materials, cellulose is cheap and has higher tolerance against interfering chemicals. Furthermore, detection elements, such as nanoparticles, can be stored in cellulose, increasing sensitivity, although at the expense of weakened mechanical strength when wet. For analysis of small volumes of sample (~10 µl), materials with low-bed volumes (for example, woven meshes, such as glass fibres) are preferred. These materials are more expensive, but have good tensile strength and allow even distribution of the sample. Therefore, the choice of paper material is important to ensure optimal performance.
The versatility of paper-based analytical devices enables their integration into environmental, health surveillance or epidemiology programmes, to provide real-time continuous data as early warning systems, particularly in low-resource settings. For example, integration with quick response (QR) codes and smartphones offers rapid and decentralized monitoring of infection transmission with comparable processing capabilities and at a lower cost compared to ‘high-end’ desktop and notebook computers170,171. Furthermore, integrated paper-based devices improve inventory and supply chain management systems, while reducing clerical errors and workload172, particularly when assisted by machine-learning algorithms170. Implementation of the latter requires technical support, fast transmission and data storage for all the involved parties. Smartphones and advanced networks can reduce data collection and transmission costs. Therefore, online diagnostics combined with standardized epidemiological data collection could improve the speed and efficacy with which we monitor and manage epidemics.
Although challenging, implementing these criteria could promote commercialization and boost field deployment of paper-based analytical devices for POC applications to diagnose infections early and to monitor food and environmental contamination.
References
Gupta, A., Gupta, R. & Singh, R. L. in Principles and Applications of Environmental Biotechnology for a Sustainable Future (ed. Singh, R. L.) 43–84 (Springer, 2017).
Doron, S. & Gorbach, S. L. in International Encyclopedia of Public Health (ed. Heggenhougen, H. K.) 273–282 (Academic, 2008).
Thompson, T. et al. The staggering death toll of drug-resistant bacteria. https://doi.org/10.1038/d41586-022-00228-x (2022).
Vos, T. et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396, 1204–1222 (2020).
Murray, C. J. L. et al. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet 399, 629–655 (2022).
Baryeh, K., Takalkar, S., Lund, M. & Liu, G. in Medical Biosensors for Point of Care (POC) Applications (ed. Narayan, R. J.) 3–25 (Woodhead, 2017).
Mabey, D., Peeling, R. W., Ustianowski, A. & Perkins, M. D. Diagnostics for the developing world. Nat. Rev. Microbiol. 2, 231–240 (2004).
Nagaraj, S., Ramlal, S., Kingston, J. & Batra, H. V. Development of IgY based sandwich ELISA for the detection of staphylococcal enterotoxin G (SEG), an egc toxin. Int. J. Food Microbiol. 237, 136–141 (2016).
Saravanan, A. et al. Methods of detection of food-borne pathogens: a review. Environ. Chem. Lett. 19, 189–207 (2021).
Bordbar, M. M., Sheini, A., Hashemi, P., Hajian, A. & Bagheri, H. Disposable paper-based biosensors for the point-of-care detection of hazardous contaminations — a review. Biosensors 11, 316 (2021).
Iwase, T. et al. A simple assay for measuring catalase activity: a visual approach. Sci. Rep. 3, 3081–3081 (2013).
Saptalena, L. G., Kuklya, A. & Telgheder, U. Gas chromatography–differential mobility spectrometry and gas chromatography–mass spectrometry for the detection of coliform bacteria. Int. J. Mass. Spectrom. 388, 17–25 (2015).
Aebisher, D., Bartusik, D. & Tabarkiewicz, J. Laser flow cytometry as a tool for the advancement of clinical medicine. Biomed. Pharmacother. 85, 434–443 (2017).
Cheng, J. H. & Sun, D. W. Recent applications of spectroscopic and hyperspectral imaging techniques with chemometric analysis for rapid inspection of microbial spoilage in muscle foods. Compr. Rev. Food Sci. Food Saf. 14, 478–490 (2015).
Pahlow, S. et al. Isolation and identification of bacteria by means of Raman spectroscopy. Adv. Drug Deliv. Rev. 89, 105–120 (2015).
Dietvorst, J. et al. Bacteria detection at a single-cell level through a cyanotype-based photochemical reaction. Anal. Chem. 94, 787–792 (2022).
Urdea, M. et al. Requirements for high impact diagnostics in the developing world. Nature 444, 73–79 (2006).
Land, K. J., Boeras, D. I., Chen, X.-S., Ramsay, A. R. & Peeling, R. W. REASSURED diagnostics to inform disease control strategies, strengthen health systems and improve patient outcomes. Nat. Microbiol. 4, 46–54 (2019).
Lee, W. G., Kim, Y.-G., Chung, B. G., Demirci, U. & Khademhosseini, A. Nano/microfluidics for diagnosis of infectious diseases in developing countries. Adv. Drug Deliv. Rev. 62, 449–457 (2010).
Bradbury, D. W. et al. Automation of biomarker preconcentration, capture, and nanozyme signal enhancement on paper-based devices. Anal. Chem. 91, 12046–12054 (2019).
Ruecha, N., Yamada, K., Suzuki, K. & Citterio, D. in Materials for Chemical Sensing (eds Paixão, T. R. L. C. & Reddy, S. M.) 29–74 (Springer, 2017).
Han, S., Chopra, M., Rubino, I. & Choi, H.-J. in Paper-based Medical Diagnostic Devices: As a Part of Bioanalysis-advanced Materials, Methods, and Devices (ed. Lee, J. H.) 137–153 (Springer, 2021).
Snyder, S. A. et al. Lysis and direct detection of coliforms on printed paper-based microfluidic devices. Lab Chip 20, 4413–4419 (2020).
Liana, D. D., Raguse, B., Gooding, J. J. & Chow, E. Recent advances in paper-based sensors. Sensors 12, 11505–11526 (2012).
Yao, Z. et al. Paper-based sensors for diagnostics, human activity monitoring, food safety and environmental detection. Sens. Diagn. 1, 312–342 (2022).
Gooding, J. J. What Is a “real sample”? ACS Sens. 3, 1609–1609 (2018).
Cate, D. M., Adkins, J. A., Mettakoonpitak, J. & Henry, C. S. Recent developments in paper-based microfluidic devices. Anal. Chem. 87, 19–41 (2015).
Morbioli, G. G., Mazzu-Nascimento, T., Stockton, A. M. & Carrilho, E. Technical aspects and challenges of colorimetric detection with microfluidic paper-based analytical devices (μPADs) — a review. Anal. Chim. Acta 970, 1–22 (2017).
Akyazi, T., Basabe-Desmonts, L. & Benito-Lopez, F. Review on microfluidic paper-based analytical devices towards commercialisation. Anal. Chim. Acta 1001, 1–17 (2018).
Zhu, G. et al. Paper-based immunosensors: current trends in the types and applied detection techniques. Trends Anal. Chem. 111, 100–117 (2019).
Wang, K., Wang, Z., Zeng, H., Luo, X. & Yang, T. Advances in portable visual detection of pathogenic bacteria. ACS Appl. Bio Mater. 3, 7291–7305 (2020).
Cho, I.-H., Bhunia, A. & Irudayaraj, J. Rapid pathogen detection by lateral-flow immunochromatographic assay with gold nanoparticle-assisted enzyme signal amplification. Int. J. Food Microbiol. 206, 60–66 (2015).
Yan, J. et al. Effect of physiochemical property of Fe3O4 particle on magnetic lateral flow immunochromatographic assay. Sens. Actuators B 197, 129–136 (2014).
Song, C. et al. Development of a lateral flow colloidal gold immunoassay strip for the simultaneous detection of Shigella boydii and Escherichia coli O157:H7 in bread, milk and jelly samples. Food Control. 59, 345–351 (2016).
Shin, J. H. et al. Multiplexed detection of foodborne pathogens from contaminated lettuces using a handheld multistep lateral flow assay device. J. Agric. Food Chem. 66, 290–297 (2018).
Funes-Huacca, M. et al. Portable self-contained cultures for phage and bacteria made of paper and tape. Lab Chip 12, 4269–4278 (2012).
Liu, H. et al. Visual and sensitive detection of viable pathogenic bacteria by sensing of RNA markers in gold nanoparticles based paper platform. Biosens. Bioelectron. 62, 38–46 (2014).
Zhao, Y. et al. Rapid multiplex detection of 10 foodborne pathogens with an up-converting phosphor technology-based 10-channel lateral flow assay. Sci. Rep. 6, 21342 (2016).
He, D., Wu, Z., Cui, B., Xu, E. & Jin, Z. Establishment of a dual mode immunochromatographic assay for Campylobacter jejuni detection. Food Chem. 289, 708–713 (2019).
Zhang, H. et al. Rapid detection of methicillin-resistant Staphylococcus aureus in pork using a nucleic acid-based lateral flow immunoassay. Int. J. Food Microbiol. 243, 64–69 (2017).
Liu, H.-b, Du, X.-j, Zang, Y.-X., Li, P. & Wang, S. SERS-based lateral flow strip biosensor for simultaneous detection of Listeria monocytogenes and Salmonella enterica serotype Enteritidis. J. Agric. Food Chem. 65, 10290–10299 (2017).
Cui, X., Xiong, Q.-R., Xiong, Y.-H., Shan, S. & Lai, W.-H. Establishing of a method combined immunomagnetic separation with colloidal gold lateral flow assay and its application in rapid detection of Escherichia coli O157:H7. Chin. J. Anal. Chem. 41, 1812–1816 (2013).
Liu, Y. et al. A highly sensitive and flexible magnetic nanoprobe labeled immunochromatographic assay platform for pathogen Vibrio parahaemolyticus. Int. J. Food Microbiol. 211, 109–116 (2015).
Shi, L. et al. A novel method to detect Listeria monocytogenes via superparamagnetic lateral flow immunoassay. Anal. Bioanal. Chem. 407, 529–535 (2015).
Pang, B. et al. Development of a low-cost paper-based ELISA method for rapid Escherichia coli O157:H7 detection. Anal. Biochem. 542, 58–62 (2018).
Zhao, Y. et al. Rapid and accurate detection of Escherichia coli O157:H7 in beef using microfluidic wax-printed paper-based ELISA. Analyst 145, 3106–3115 (2020).
Trinh, T. N. D., Thai, D. A. & Lee, N. Y. Pop-up paper-based and fully integrated microdevice for point-of-care testing of vancomycin-resistant Enterococcus. Sens. Actuators B 345, 130362 (2021).
Zhuang, J. et al. SERS-based CRISPR/Cas assay on microfluidic paper analytical devices for supersensitive detection of pathogenic bacteria in foods. Biosens. Bioelectron. 207, 114167 (2022).
Zhou, B. et al. CRISPR/Cas12a based fluorescence-enhanced lateral flow biosensor for detection of Staphylococcus aureus. Sens. Actuators B 351, 130906 (2022).
Foo, P. C. et al. Loop-mediated isothermal amplification (LAMP) reaction as viable PCR substitute for diagnostic applications: a comparative analysis study of LAMP, conventional PCR, nested PCR (nPCR) and real-time PCR (qPCR) based on Entamoeba histolytica DNA derived from faecal sample. BMC Biotechnol. 20, 34 (2020).
Qiu, E. M. et al. CRISPR-based detection of Helicobacter pylori in stool samples. Helicobacter 26, e12828 (2021).
Seo, J. H. et al. Development of a high-throughput centrifugal loop-mediated isothermal amplification microdevice for multiplex foodborne pathogenic bacteria detection. Sens. Actuators B 246, 146–153 (2017).
Chen, S. et al. A novel AuNPs colorimetric sensor for sensitively detecting viable Salmonella typhimurium based on dual aptamers. Food Control. 115, 107281 (2020).
Yang, X., Zhou, X., Zhu, M. & Xing, D. Sensitive detection of Listeria monocytogenes based on highly efficient enrichment with vancomycin-conjugated brush-like magnetic nano-platforms. Biosens. Bioelectron. 91, 238–245 (2017).
Pang, B. et al. Colorimetric detection of Staphylococcus aureus using gold nanorods labeled with yolk immunoglobulin and urease, magnetic beads, and a phenolphthalein impregnated test paper. Microchim. Acta 186, 611 (2019).
You, S.-M. et al. Paper-based colorimetric detection of pathogenic bacteria in food through magnetic separation and enzyme-mediated signal amplification on paper disc. Anal. Chim. Acta 1151, 338252 (2021).
Mazur, F., Tran, H., Kuchel, R. P. & Chandrawati, R. Rapid detection of listeriolysin O toxin based on a nanoscale liposome–gold nanoparticle platform. ACS Appl. Nano Mater. 3, 7270–7280 (2020).
Alhogail, S., Suaifan, G. A. R. Y. & Zourob, M. Rapid colorimetric sensing platform for the detection of Listeria monocytogenes foodborne pathogen. Biosens. Bioelectron. 86, 1061–1066 (2016).
Suaifan, G. A. R. Y., Alhogail, S. & Zourob, M. Rapid and low-cost biosensor for the detection of Staphylococcus aureus. Biosens. Bioelectron. 90, 230–237 (2017).
Suaifan, G. A. R. Y., Alhogail, S. & Zourob, M. Paper-based magnetic nanoparticle-peptide probe for rapid and quantitative colorimetric detection of Escherichia coli O157:H7. Biosens. Bioelectron. 92, 702–708 (2017).
Janzen, M. C., Ponder, J. B., Bailey, D. P., Ingison, C. K. & Suslick, K. S. Colorimetric sensor arrays for volatile organic compounds. Anal. Chem. 78, 3591–3600 (2006).
Carey, J. R. et al. Rapid identification of bacteria with a disposable colorimetric sensing array. J. Am. Chem. Soc. 133, 7571–7576 (2011).
Chen, Q., Li, H., Ouyang, Q. & Zhao, J. Identification of spoilage bacteria using a simple colorimetric sensor array. Sens. Actuators B 205, 1–8 (2014).
Yang, M. et al. Machine learning-enabled non-destructive paper chromogenic array detection of multiplexed viable pathogens on food. Nat. Food 2, 110–117 (2021).
Jia, Z. et al. Nondestructive multiplex detection of foodborne pathogens with background microflora and symbiosis using a paper chromogenic array and advanced neural network. Biosens. Bioelectron. 183, 113209 (2021).
Ali, M. M. et al. A DNAzyme-based colorimetric paper sensor for Helicobacter pylori. Angew. Chem. Int. Ed. 58, 9907–9911 (2019).
Song, C., Liu, J., Li, J. & Liu, Q. Dual FITC lateral flow immunoassay for sensitive detection of Escherichia coli O157:H7 in food samples. Biosens. Bioelectron. 85, 734–739 (2016).
Pang, B. et al. Development of a self-priming PDMS/paper hybrid microfluidic chip using mixed-dye-loaded loop-mediated isothermal amplification assay for multiplex foodborne pathogens detection. Anal. Chim. Acta 1040, 81–89 (2018).
Pisamayarom, K., Suriyasomboon, A. & Chaumpluk, P. Simple screening of Listeria monocytogenes based on a fluorescence assay via a laminated lab-on-paper chip. Biosensors 7, 56 (2017).
Wang, Y., Ping, J., Ye, Z., Wu, J. & Ying, Y. Impedimetric immunosensor based on gold nanoparticles modified graphene paper for label-free detection of Escherichia coli O157:H7. Biosens. Bioelectron. 49, 492–498 (2013).
Vizzini, P. et al. Highly sensitive detection of Campylobacter spp. in chicken meat using a silica nanoparticle enhanced dot blot DNA biosensor. Biosens. Bioelectron. 171, 112689 (2021).
Preechakasedkit, P. et al. Development of a one-step immunochromatographic strip test using gold nanoparticles for the rapid detection of Salmonella Typhi in human serum. Biosens. Bioelectron. 31, 562–566 (2012).
Cho, I.-H. & Irudayaraj, J. Lateral-flow enzyme immunoconcentration for rapid detection of Listeria monocytogenes. Anal. Bioanal. Chem. 405, 3313–3319 (2013).
Bisha, B. et al. Colorimetric paper-based detection of Escherichia coli, Salmonella spp., and Listeria monocytogenes from large volumes of agricultural water. J. Vis. Exp. 88, 51414 (2014).
Singh, J., Sharma, S. & Nara, S. Nanogold based lateral flow assay for the detection of Salmonella Typhi in environmental water samples. Anal. Methods 7, 9281–9288 (2015).
Hossain, S. M. Z. et al. Multiplexed paper test strip for quantitative bacterial detection. Anal. Bioanal. Chem. 403, 1567–1576 (2012).
Zhang, L. et al. Ultrasensitive detection of viable Enterobacter sakazakii by a continual cascade nanozyme biosensor. Anal. Chem. 89, 10194–10200 (2017).
Pan, R. et al. Gold nanoparticle-based enhanced lateral flow immunoassay for detection of Cronobacter sakazakii in powdered infant formula. J. Dairy Sci. 101, 3835–3843 (2018).
Choi, J. R. et al. An integrated paper-based sample-to-answer biosensor for nucleic acid testing at the point of care. Lab Chip 16, 611–621 (2016).
Han, J. et al. Nanozyme-based lateral flow assay for the sensitive detection of Escherichia coli O157:H7 in milk. J. Dairy Sci. 101, 5770–5779 (2018).
Fu, J. et al. Dramatically enhanced immunochromatographic assay using cascade signal amplification for ultrasensitive detection of Escherichia coli O157:H7 in milk. J. Agric. Food Chem. 68, 1118–1125 (2020).
Chen, M. et al. Dual gold nanoparticle lateflow immunoassay for sensitive detection of Escherichia coli O157:H7. Anal. Chim. Acta 876, 71–76 (2015).
Wang, J.-Y. et al. Development of colloidal gold immunochromatographic signal-amplifying system for ultrasensitive detection of Escherichia coli O157:H7 in milk. RSC Adv. 5, 62300–62305 (2015).
Lu, C., Gao, X., Chen, Y., Ren, J. & Liu, C. Aptamer-based lateral flow test strip for the simultaneous detection of Salmonella Typhimurium, Escherichia coli O157:H7 and Staphylococcus aureus. Anal. Lett. 53, 646–659 (2020).
Ren, W., Cho, I.-H., Zhou, Z. & Irudayaraj, J. Ultrasensitive detection of microbial cells using magnetic focus enhanced lateral flow sensors. Chem. Commun. 52, 4930–4933 (2016).
Wu, W. et al. A sensitive lateral flow biosensor for Escherichia coli O157:H7 detection based on aptamer mediated strand displacement amplification. Anal. Chim. Acta 861, 62–68 (2015).
Hwang, J., Kwon, D., Lee, S. & Jeon, S. Detection of Salmonella bacteria in milk using gold-coated magnetic nanoparticle clusters and lateral flow filters. RSC Adv. 6, 48445–48448 (2016).
Xia, S., Yu, Z., Liu, D., Xu, C. & Lai, W. Developing a novel immunochromatographic test strip with gold magnetic bifunctional nanobeads (GMBN) for efficient detection of Salmonella Choleraesuis in milk. Food Control. 59, 507–512 (2016).
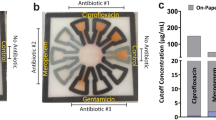
Xu, B. et al. Simultaneous identification and antimicrobial susceptibility testing of multiple uropathogens on a microfluidic chip with paper-supported cell culture arrays. Anal. Chem. 88, 11593–11600 (2016).
Kim, H. J., Kwon, C. & Noh, H. Paper-based diagnostic system facilitating Escherichia coli assessments by duplex coloration. ACS Sens. 4, 2435–2441 (2019).
Kim, H. J., Kwon, C., Lee, B. S. & Noh, H. One-step sensing of foodborne pathogenic bacteria using a 3D paper-based device. Analyst 144, 2248–2255 (2019).
Wang, C., Gao, X., Wang, S. & Liu, Y. A smartphone-integrated paper sensing system for fluorescent and colorimetric dual-channel detection of foodborne pathogenic bacteria. Anal. Bioanal. Chem. 412, 611–620 (2020).
Kim, J.-Y. & Yeo, M.-K. A fabricated microfluidic paper-based analytical device (μPAD) for in situ rapid colorimetric detection of microorganisms in environmental water samples. Mol. Cell. Toxicol. 12, 101–109 (2016).
Ren, W., Liu, W. & Irudayaraj, J. A net fishing enrichment strategy for colorimetric detection of E. coli O157:H7. Sens. Actuators B 247, 923–929 (2017).
Sun, J., Huang, J., Li, Y., Lv, J. & Ding, X. A simple and rapid colorimetric bacteria detection method based on bacterial inhibition of glucose oxidase-catalyzed reaction. Talanta 197, 304–309 (2019).
Li, D. et al. A multiplex PCR method to detect 14 Escherichia coli serogroups associated with urinary tract infections. J. Microbiol. Methods 82, 71–77 (2010).
Lee, J. W., Nguyen, V. D. & Seo, T. S. Paper-based molecular diagnostics for the amplification and detection of pathogenic bacteria from human whole blood and milk without a sample preparation step. BioChip J. 13, 243–250 (2019).
Mukama, O. et al. An ultrasensitive and specific point-of-care CRISPR/Cas12 based lateral flow biosensor for the rapid detection of nucleic acids. Biosens. Bioelectron. 159, 112143 (2020).
Qian, J. et al. A portable CRISPR Cas12a based lateral flow platform for sensitive detection of Staphylococcus aureus with double insurance. Food Control. 132, 108485 (2022).
Lafleur, L. K. et al. A rapid, instrument-free, sample-to-result nucleic acid amplification test. Lab Chip 16, 3777–3787 (2016).
Tang, R. et al. A fully disposable and integrated paper-based device for nucleic acid extraction, amplification and detection. Lab Chip 17, 1270–1279 (2017).
Noiphung, J. & Laiwattanapaisal, W. Multifunctional paper-based analytical device for in situ cultivation and screening of Escherichia coli infections. Sci. Rep. 9, 1555 (2019).
Wang, W. et al. Gold nanoparticle-based paper sensor for multiple detection of 12 Listeria spp. by P60-mediated monoclonal antibody. Food Agric. Immunol. 28, 274–287 (2017).
Wang, L. et al. A lateral flow strip combined with Cas9 nickase-triggered amplification reaction for dual food-borne pathogen detection. Biosens. Bioelectron. 165, 112364 (2020).
Li, H. B. et al. High concentration of Cas12a effector tolerates more mismatches on ssDNA. FASEB J. 35, e21153 (2021).
You, Y. et al. Highly specific and sensitive detection of Yersinia pestis by portable Cas12a-UPTLFA platform. Front. Microbiol. 12, 700016 (2021).
Wang, H. et al. CRISPR/Cas9 bridged recombinase polymerase amplification with lateral flow biosensor removing potential primer-dimer interference for robust Staphylococcus aureus assay. Sens. Actuators B 369, 132293 (2022).
Wang, W. et al. Identification and quantification of eight Listeria monocytogene serotypes from Listeria spp. using a gold nanoparticle-based lateral flow assay. Microchim. Acta 184, 715–724 (2017).
Rodriguez-Quijada, C. et al. Optimization of paper-based nanoparticle immunoassays for direct detection of the bacterial pathogen V. parahaemolyticus in oyster hemolymph. Anal. Methods 12, 3056–3063 (2020).
Srisa-Art, M., Boehle, K. E., Geiss, B. J. & Henry, C. S. Highly sensitive detection of Salmonella Typhimurium using a colorimetric paper-based analytical device coupled with immunomagnetic separation. Anal. Chem. 90, 1035–1043 (2018).
Carrell, C. S. et al. Rotary manifold for automating a paper-based Salmonella immunoassay. RSC Adv. 9, 29078–29086 (2019).
Bordbar, M. M., Tashkhourian, J., Tavassoli, A., Bahramali, E. & Hemmateenejad, B. Ultrafast detection of infectious bacteria using optoelectronic nose based on metallic nanoparticles. Sens. Actuators B 319, 128262 (2020).
Lim Sung, H. et al. Colorimetric sensor array allows fast detection and simultaneous identification of sepsis-causing bacteria in spiked blood culture. J. Clin. Microbiol. 52, 592–598 (2014).
Bordbar, M. M., Tashkhourian, J. & Hemmateenejad, B. Structural elucidation and ultrasensitive analyses of volatile organic compounds by paper-based nano-optoelectronic noses. ACS Sens. 4, 1442–1451 (2019).
Fronczek, C. F., Park, T. S., Harshman, D. K., Nicolini, A. M. & Yoon, J.-Y. Paper microfluidic extraction and direct smartphone-based identification of pathogenic nucleic acids from field and clinical samples. RSC Adv. 4, 11103–11110 (2014).
Kang, D.-K. et al. Rapid detection of single bacteria in unprocessed blood using integrated comprehensive droplet digital detection. Nat. Commun. 5, 5427 (2014).
Tram, K., Kanda, P., Salena, B. J., Huan, S. & Li, Y. Translating bacterial detection by DNAzymes into a litmus test. Angew. Chem. Int. Ed. 53, 12799–12802 (2014).
Huang, Z., Cui, X., Xie, Q.-Y., Liu, D.-F. & Lai, W.-H. Short communication: a novel method using immunomagnetic separation with a fluorescent nanobeads lateral flow assay for the rapid detection of low-concentration Escherichia coli O157:H7 in raw milk. J. Dairy Sci. 99, 9581–9585 (2016).
Seok, Y. et al. A paper-based device for performing loop-mediated isothermal amplification with real-time simultaneous detection of multiple DNA targets. Theranostics 7, 2220–2230 (2017).
Luo, K. et al. Comparison of 4 label-based immunochromatographic assays for the detection of Escherichia coli O157:H7 in milk. J. Dairy Sci. 100, 5176–5187 (2017).
Ali, M. M. et al. A printed multicomponent paper sensor for bacterial detection. Sci. Rep. 7, 12335–12335 (2017).
Trinh, T. N. D. & Lee, N. Y. A rapid and eco-friendly isothermal amplification microdevice for multiplex detection of foodborne pathogens. Lab Chip 18, 2369–2377 (2018).
Xing, K.-Y. et al. Novel immunochromatographic assay based on Eu (III)-doped polystyrene nanoparticle-linker-monoclonal antibody for sensitive detection of Escherichia coli O157:H7. Anal. Chim. Acta 998, 52–59 (2018).
Ahn, H., Batule, B. S., Seok, Y. & Kim, M.-G. Single-step recombinase polymerase amplification assay based on a paper chip for simultaneous detection of multiple foodborne pathogens. Anal. Chem. 90, 10211–10216 (2018).
Na, M. et al. Determination of pathogenic bacteria–Bacillus anthrax spores in environmental samples by ratiometric fluorescence and test paper based on dual-emission fluorescent silicon nanoparticles. J. Hazard. Mater. 386, 121956 (2020).
Zhang, M. et al. A newly developed paper embedded microchip based on LAMP for rapid multiple detections of foodborne pathogens. BMC Microbiol. 21, 197 (2021).
Sheini, A. A point-of-care testing sensor based on fluorescent nanoclusters for rapid detection of septicemia in children. Sens. Actuators B 328, 129029 (2021).
Adkins, J. A. et al. Colorimetric and electrochemical bacteria detection using printed paper- and transparency-based analytic devices. Anal. Chem. 89, 3613–3621 (2017).
Jokerst, J. C. et al. Development of a paper-based analytical device for colorimetric detection of select foodborne pathogens. Anal. Chem. 84, 2900–2907 (2012).
Sun, L. et al. A novel, simple and low-cost paper-based analytical device for colorimetric detection of Cronobacter spp. Anal. Chim. Acta 1036, 80–88 (2018).
Ilhan, H. et al. The coupling of immunomagnetic enrichment of bacteria with paper-based platform. Talanta 201, 245–252 (2019).
Schaumburg, F., Carrell, C. S. & Henry, C. S. Rapid bacteria detection at low concentrations using sequential immunomagnetic separation and paper-based isotachophoresis. Anal. Chem. 91, 9623–9630 (2019).
Qiao, Z., Cai, Q., Fu, Y., Lei, C. & Yang, W. Visual and quantitative detection of E. coli O157:H7 by coupling immunomagnetic separation and quantum dot-based paper strip. Anal. Bioanal. Chem. 413, 4417–4426 (2021).
Yu, J., Su, J., Zhang, J., Wei, X. & Guo, A. CdTe/CdS quantum dot-labeled fluorescent immunochromatography test strips for rapid detection of Escherichia coli O157:H7. RSC Adv. 7, 17819–17823 (2017).
Hu, J. et al. Colorimetric-fluorescent-magnetic nanosphere-based multimodal assay platform for Salmonella detection. Anal. Chem. 91, 1178–1184 (2019).
Bhardwaj, J., Devarakonda, S., Kumar, S. & Jang, J. Development of a paper-based electrochemical immunosensor using an antibody-single walled carbon nanotubes bio-conjugate modified electrode for label-free detection of foodborne pathogens. Sens. Actuators B 253, 115–123 (2017).
Silva, N. F. D. et al. Development of a disposable paper-based potentiometric immunosensor for real-time detection of a foodborne pathogen. Biosens. Bioelectron. 141, 111317 (2019).
Khan, M. S. et al. Electrically-receptive and thermally-responsive paper-based sensor chip for rapid detection of bacterial cells. Biosens. Bioelectron. 110, 132–140 (2018).
Mondal, D., Binish, R., Samanta, S., Paul, D. & Mukherji, S. Detection of total bacterial load in water samples using a disposable impedimetric sensor. IEEE Sens. J. 20, 1712–1720 (2020).
Muhammad-Tahir, Z. & Alocilja, E. C. Fabrication of a disposable biosensor for Escherichia coli O157:H7 detection. IEEE Sens. J. 3, 345–351 (2003).
Lin, Y.-H. et al. Disposable amperometric immunosensing strips fabricated by Au nanoparticles-modified screen-printed carbon electrodes for the detection of foodborne pathogen Escherichia coli O157:H7. Biosens. Bioelectron. 23, 1832–1837 (2008).
Karuppiah, S., Mishra, N. C., Tsai, W.-C., Liao, W.-S. & Chou, C.-F. Ultrasensitive and low-cost paper-based graphene oxide nanobiosensor for monitoring water-borne bacterial contamination. ACS Sens. 6, 3214–3223 (2021).
Morales-Narváez, E., Naghdi, T., Zor, E. & Merkoçi, A. Photoluminescent lateral-flow immunoassay revealed by graphene oxide: highly sensitive paper-based pathogen detection. Anal. Chem. 87, 8573–8577 (2015).
Han, S.-M. et al. Performance characterization of two-dimensional paper chromatography-based biosensors for biodefense, exemplified by detection of Bacillus anthracis spores. BioChip J. 12, 59–68 (2018).
Gumustas, A. et al. Paper based lateral flow immunoassay for the enumeration of Escherichia coli in urine. Anal. Methods 10, 1213–1218 (2018).
Huang, F., Zhang, H., Wang, L., Lai, W. & Lin, J. A sensitive biosensor using double-layer capillary based immunomagnetic separation and invertase-nanocluster based signal amplification for rapid detection of foodborne pathogen. Biosens. Bioelectron. 100, 583–590 (2018).
Choi, J. R., Nilghaz, A., Chen, L., Chou, K. C. & Lu, X. Modification of thread-based microfluidic device with polysiloxanes for the development of a sensitive and selective immunoassay. Sens. Actuators B 260, 1043–1051 (2018).
Klug, K. E., Reynolds, K. A. & Yoon, J.-Y. A capillary flow dynamics-based sensing modality for direct environmental pathogen monitoring. Chem. A Eur. J. 24, 6025–6029 (2018).
Weng, X., Kang, Y., Guo, Q., Peng, B. & Jiang, H. Recent advances in thread-based microfluidics for diagnostic applications. Biosens. Bioelectron. 132, 171–185 (2019).
Alsaeed, B. & Mansour, F. R. Distance-based paper microfluidics; principle, technical aspects and applications. Microchem. J. 155, 104664 (2020).
Kim, S. et al. Human sensor-inspired supervised machine learning of smartphone-based paper microfluidic analysis for bacterial species classification. Biosens. Bioelectron. 188, 113335 (2021).
Cho, S., Park, T. S., Nahapetian, T. G. & Yoon, J.-Y. Smartphone-based, sensitive µPAD detection of urinary tract infection and gonorrhea. Biosens. Bioelectron. 74, 601–611 (2015).
Sweeney, R. E., Budiman, E. & Yoon, J.-Y. Mie scatter spectra-based device for instant, contact-free, and specific diagnosis of bacterial skin infection. Sci. Rep. 7, 4801 (2017).
Li, M., Wang, L., Qi, W., Liu, Y. & Lin, J. Challenges and perspectives for biosensing of bioaerosol containing pathogenic microorganisms. Micromachines 12, 798 (2021).
Seok, Y., Lee, J. & Kim, M.-G. Paper-based airborne bacteria collection and DNA extraction kit. Biosensors 11, 375 (2021).
Seok, Y., Jang, H., Oh, J., Joung, H.-A. & Kim, M.-G. A handheld lateral flow strip for rapid DNA extraction from Staphylococcus aureus cell spiked in various samples. Biomed. Phys. Eng. Express 5, 035035 (2019).
Nguyen, D. T., Kim, H. R., Jung, J. H., Lee, K.-B. & Kim, B. C. The development of paper discs immobilized with luciferase/D-luciferin for the detection of ATP from airborne bacteria. Sens. Actuators B 260, 274–281 (2018).
Park, C., Lee, J., Lee, D. & Jang, J. Paper-based electrochemical peptide sensor for label-free and rapid detection of airborne Bacillus anthracis simulant spores. Sens. Actuators B 355, 131321 (2022).
Garland, T. Jr & Kelly, S. A. Phenotypic plasticity and experimental evolution. J. Exp. Biol. 209, 2344–2361 (2006).
Matuła, K. et al. Phenotypic plasticity of Escherichia coli upon exposure to physical stress induced by ZnO nanorods. Sci. Rep. 9, 8575 (2019).
Kumar, A. A. et al. From the bench to the field in low-cost diagnostics: two case studies. Angew. Chem. Int. Ed. 54, 5836–5853 (2015).
Sena-Torralba, A. et al. Paper-based electrophoretic bioassay: biosensing in whole blood operating via smartphone. Anal. Chem. 93, 3112–3121 (2021).
Pan, H. et al. Quantitative detection of viable but nonculturable state Escherichia coli O157:H7 by ddPCR combined with propidium monoazide. Food Control. 112, 107140 (2020).
Gonzalez-Solino, C. & Lorenzo, M. D. Enzymatic fuel cells: towards self-powered implantable and wearable diagnostics. Biosensors 8, 11 (2018).
Escalona-Villalpando, R. A. et al. Improving the performance of lactate/oxygen biofuel cells using a microfluidic design. J. Power Sources 342, 546–552 (2017).
Fozouni, P. et al. Amplification-free detection of SARS-CoV-2 with CRISPR–Cas13a and mobile phone microscopy. Cell 184, 323–333 (2021).
Pang, Y. et al. CRISPR–Cas12a mediated SERS lateral flow assay for amplification-free detection of double-stranded DNA and single-base mutation. Chem. Eng. J. 429, 132109 (2022).
Suea-Ngam, A., Howes, P. D. & deMello, A. J. An amplification-free ultra-sensitive electrochemical CRISPR/Cas biosensor for drug-resistant bacteria detection. Chem. Sci. 12, 12733–12743 (2021).
Parolo, C. et al. Tutorial: design and fabrication of nanoparticle-based lateral-flow immunoassays. Nat. Protoc. 15, 3788–3816 (2020).
Khanal, B., Pokhrel, P., Khanal, B. & Giri, B. Machine-learning-assisted analysis of colorimetric assays on paper analytical devices. ACS Omega 6, 33837–33845 (2021).
Ding, X., Mauk, M. G., Yin, K., Kadimisetty, K. & Liu, C. Interfacing pathogen detection with smartphones for point-of-care applications. Anal. Chem. 91, 655–672 (2019).
Estcourt, C. S. et al. The eSexual Health Clinic system for management, prevention, and control of sexually transmitted infections: exploratory studies in people testing for Chlamydia trachomatis. Lancet Public Health 2, e182–e190 (2017).
Carlisle, R. Scientific American Inventions and Discoveries: All the Milestones in Ingenuity — From the Discovery of Fire to the Invention of the Microwave Oven (Wileys, 2004).
Maumené, M. On a new reagent for ascertaining the presence of sugar in certain liquids. Phil. Mag. Ser. 36, 482–482 (1850).
Comer, J. P. Semiquantitative specific test paper for glucose in urine. Anal. Chem. 28, 1748–1750 (1956).
Free, A. H., Adams, E. C., Kercher, M. L., Free, H. M. & Cook, M. H. Simple specific test for urine glucose. Clin. Chem. 3, 163–168 (1957).
Hawkes, R., Niday, E. & Gordon, J. A dot-immunobinding assay for monoclonal and other antibodies. Anal. Biochem. 119, 142–147 (1982).
Martinez, A. W., Phillips, S. T., Butte, M. J. & Whitesides, G. M. Patterned paper as a platform for inexpensive, low-volume, portable bioassays. Angew. Chem. Int. Ed. 46, 1318–1320 (2007).
Dungchai, W., Chailapakul, O. & Henry, C. S. Electrochemical detection for paper-based microfluidics. Anal. Chem. 81, 5821–5826 (2009).
Castro Arnold, R. et al. Novel point-of-care test for simultaneous detection of nontreponemal and treponemal antibodies in patients with syphilis. J. Clin. Microbiol. 48, 4615–4619 (2010).
World Health Organization Regional Office for Europe. Circular economy and health: opportunities and risks (WHO, 2018).
Corona, B., Shen, L., Reike, D., Rosales Carreón, J. & Worrell, E. Towards sustainable development through the circular economy — a review and critical assessment on current circularity metrics. Resour. Conserv. Recycl. 151, 104498 (2019).
Arruda, E. H., Melatto, R. A. P. B., Levy, W. & Conti, D. D. M. Circular economy: a brief literature review (2015–2020). Sustain. Oper. Comput. 2, 79–86 (2021).
Hofstetter, J. S. et al. From sustainable global value chains to circular economy — different silos, different perspectives, but many opportunities to build bridges. Circ. Econ. Sust. 1, 21–47 (2021).
Street, A., Vernooij, E. & Rogers, M. H. Diagnostic waste: whose responsibility? Global. Health 18, 30 (2022).
Parashar, N. & Hait, S. Plastics in the time of COVID-19 pandemic: protector or polluter? Sci. Total Environ. 759, 144274 (2021).
Acknowledgements
R.C. acknowledges support from the National Health and Medical Research Council Emerging Leadership Investigator Grant (NHMRC APP1173428) and the UNSW Scientia Fellowship.
Author information
Authors and Affiliations
Contributions
F.M. conceptualized the content, investigated the literature, analysed the data, wrote and revised the manuscript and designed the figures. A.D.T. investigated the literature, analysed the data, wrote the manuscript and designed the figures. Y.Z. investigated the literature, analysed the data and wrote the manuscript. Y.G. investigated the literature, analysed the data and wrote the manuscript. R.C. conceptualized the content, investigated the literature, revised the manuscript and supervised the project.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Bioengineering thanks Boce Zhang, Jeong-Yeol Yoon and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
COVID-19 rapid antigen test: https://asm.org/Articles/2020/August/How-the-SARS-CoV-2-EUA-Antigen-Tests-Work
National policy targets: https://www.epa.nsw.gov.au/your-environment/recycling-and-reuse/response-to-china-national-sword/circular-economy-policy
Top 10 global causes of death in 2019: https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates
Unsafe food: https://www.who.int/NEWS-ROOM/FACT-SHEETS/DETAIL/FOOD-SAFETY
WHO-UNICEF: https://apps.who.int/iris/handle/10665/331499
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mazur, F., Tjandra, A.D., Zhou, Y. et al. Paper-based sensors for bacteria detection. Nat Rev Bioeng 1, 180–192 (2023). https://doi.org/10.1038/s44222-023-00024-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s44222-023-00024-w
This article is cited by
-
Bioengineering for low-resource settings
Nature Reviews Bioengineering (2023)
-
Wearable flexible microfluidic sensing technologies
Nature Reviews Bioengineering (2023)