Abstract
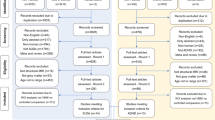
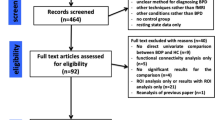
Individuals with disruptive behaviour disorders in youth and antisocial personality disorder and psychopathy as adults share some clinical characteristics, but also diverge in important ways. Existing meta-analyses of structural imaging studies suggest abnormalities within these disorders; however, so far none has examined the role of variability. Here we performed a systematic review and meta-analysis to examine both variability (coefficient of variation ratio) and magnitude of brain volume differences between antisocial groups and healthy controls (quantified using Hedges’ g). A comprehensive search was conducted of PubMed, EMBASE, Web of Science, Scopus and PsycINFO from inception to 31 January 2022 (pre-registered with PROSPERO, ID number CRD42021250980, registered 25 June 2021). We included studies which included individuals with disruptive behaviour disorder (± callous–unemotional traits) or antisocial personality disorder (± psychopathy), defined using standardized classificatory tools (Diagnostic and Statistical Manual of Mental Disorders or International Classification of Diseases criteria for disruptive behaviour disorders and antisocial personality disorder, Psychopathy Checklist: Revised or Psychopathy Checklist: Screening Version for psychopathy) and a healthy control group, and which had sufficient data to extract mean and standard deviations, or t or P values, for both groups. We measured the relative variability of brain regions in antisocial individuals compared with controls, by using the log coefficient of variability ratio. Between-group differences in mean volumes were quantified using standardized mean difference. Risk of bias was assessed using modified version of the Newcastle–Ottawa Scale for case–control studies. Twenty-three studies met inclusion criteria. In antisocial individuals, there was significantly increased variability for total grey matter (Z = −2.6581, P = 0.0079) and overall decreases in mean volume for total whole brain (g = −0.41; 95% confidence interval (CI) −0.67 to −0.15, P = 0.0016), total grey matter (g = −0.6; 95% CI −0.93 to −0.26, P = 0.004) and amygdala (g = −0.89; 95% CI −1.55 to −0.22, P = 0.009), compared with healthy controls. This suggests a key role for structural variability in clinical divergence within these disorders. The key limitations were lack of studies for some brain regions of interest, including insula, and inconsistent clinical phenotyping. Further studies should seek to specify how this neurobiological variability maps to clinical variability and whether this holds potential value as a biomarker to guide prognosis or treatment selection.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$59.00 per year
only $4.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Analysis data are available at https://github.com/JohnTullyPsych/AntisocialStructuralVariabilityMeta ref. 85, and data sources are all listed in AntisocialStructuralVariabilityMeta_Excel.csv.
Code availability
Analysis code is available at https://github.com/JohnTullyPsych/AntisocialStructuralVariabilityMeta ref. 85, and code sources are all listed in AntisocialStructuralVariabilityMeta_Excel.csv.
References
Falk, Ö. et al. The 1% of the population accountable for 63% of all violent crime convictions. Soc. Psychiatry Psychiatr. Epidemiol. 49, 559–571 (2014).
Piquero, A. R., & Moffitt, T. E. in Encyclopedia of Criminology and Criminal Justice (ed. Weisburd, D.) 3121–3127 (Springer, 2014).
Moffitt, T. E. Male antisocial behaviour in adolescence and beyond. Nat. Hum. Behav. 2, 177 (2018).
Viding, E. & McCrory, E. J. Genetic and neurocognitive contributions to the development of psychopathy. Dev. Psychopathol. 24, 969–983 (2012).
Lynam, D. R., Derefinko, K. J., Caspi, A., Loeber, R. & Stouthamer-Loeber, M. The content validity of juvenile psychopathy: an empirical examination. Psychol. Assess. 19, 363 (2007).
Forsman, M., Lichtenstein, P., Andershed, H. & Larsson, H. Genetic effects explain the stability of psychopathic personality from mid-to late adolescence. J. Abnorm. Psychol. 117, 606 (2008).
Kosson, D. S., Lorenz, A. R. & Newman, J. P. Effects of comorbid psychopathy on criminal offending and emotion processing in male offenders with antisocial personality disorder. J. Abnorm. Psychol. 115, 798 (2006).
Coid, J. & Ullrich, S. Antisocial personality disorder is on a continuum with psychopathy. Compr. Psychiatry 51, 426–433 (2010).
Frick, P. J., Ray, J. V., Thornton, L. C. & Kahn, R. E. Can callous-unemotional traits enhance the understanding, diagnosis, and treatment of serious conduct problems in children and adolescents? A comprehensive review. Psychol. Bull. 140, 1–57 (2014).
Guy, L. S., Edens, J. F., Anthony, C. & Douglas, K. S. Does psychopathy predict institutional misconduct among adults? A meta-analytic investigation. J. Consult. Clin. Psychol. 73, 1056 (2005).
Noordermeer, S. D. S., Luman, M. & Oosterlaan, J. A systematic review and meta-analysis of neuroimaging in oppositional defiant disorder (ODD) and conduct disorder (CD) taking attention-deficit hyperactivity disorder (ADHD) into account. Neuropsychol. Rev. 26, 44–72 (2016).
Rogers, J. C., De & Brito, S. A. Cortical and subcortical gray matter volume in youths with conduct problems a meta-analysis. JAMA Psychiatry. 73, 64–72 (2016).
Santana, E. J. The brain of the psychopath: a systematic review of structural neuroimaging studies. Psychol. Neurosci. 9, 420–443 (2016).
Anderson, N. E. & Kiehl, K. A. The psychopath magnetized: insights from brain imaging. Trends Cogn. Sci. 16, 52–60 (2012).
Harenski, C., Hare, R. D., & Kiehl, K. A. in Responsibility and Psychopathy: Interfacing Law, Psychiatry and Philosophy (eds Malatesti, L. & McMillan, J.) Ch. 8 (Oxford University Press, 2010).
De Brito, S. A., McDonald, D., Camilleri, J. A. & Rogers, J. C. Cortical and subcortical gray matter volume in psychopathy: a voxel-wise meta-analysis. J. Abnorm. Psychol. 130, 627 (2021).
Brugger, S. P. & Howes, O. D. Heterogeneity and homogeneity of regional brain structure in schizophrenia: a meta-analysis. JAMA Psychiatry 74, 1104–1111 (2017).
Rogdaki, M. et al. Magnitude and heterogeneity of brain structural abnormalities in 22q11.2 deletion syndrome: a meta-analysis. Mol. Psychiatry 25, 1704–1717 (2020).
Kaminski, J. et al. Glutamate in the dorsolateral prefrontal cortex in patients with schizophrenia: a meta-analysis of 1H-magnetic resonance spectroscopy studies. Biol. Psychiatry 89, 270–277 (2021).
Fairchild, G. et al. Decision making and executive function in male adolescents with early-onset or adolescence-onset conduct disorder and control subjects. Biol. Psychiatry 66, 162–168 (2009).
Fanti, K. A., Kimonis, E. R., Hadjicharalambous, M.-Z. & Steinberg, L. Do neurocognitive deficits in decision making differentiate conduct disorder subtypes? Eur. Child Adolesc. Psychiatry 25, 989–996 (2016).
Schwenck, C. et al. Empathy in children with autism and conduct disorder: group‐specific profiles and developmental aspects. J. Child Psychol. Psychiatry 53, 651–659 (2012).
Marsh, A. A. & Blair, R. J. R. Deficits in facial affect recognition among antisocial populations: a meta-analysis. Neurosci. Biobehav. Rev. 32, 454–465 (2008).
Dawel, A., O’Kearney, R., McKone, E. & Palermo, R. Not just fear and sadness: meta-analytic evidence of pervasive emotion recognition deficits for facial and vocal expressions in psychopathy. Neurosci. Biobehav. Rev. 36, 2288–2304 (2012).
Gregory, S. et al. The antisocial brain: psychopathy matters: a structural MRI investigation of antisocial male violent offenders. Arch. Gen. Psychiatry 69, 962–972 (2012).
Pappa, I. et al. A genome‐wide approach to children’s aggressive behavior: the EAGLE consortium. Am. J. Med. Genet. B 171, 562–572 (2016).
Tielbeek, J. J. et al. Unraveling the genetic etiology of adult antisocial behavior: a genome-wide association study. PLoS ONE 7, e45086 (2012).
Rautiainen, M. et al. Genome-wide association study of antisocial personality disorder. Transl. Psychiatry 6, e883 (2016).
Panizzon, M. S. et al. Distinct genetic influences on cortical surface area and cortical thickness. Cerebr. Cortex 19, 2728–2735 (2009).
Ecker, C. et al. Brain surface anatomy in adults with autism: the relationship between surface area, cortical thickness, and autistic symptoms. JAMA Psychiatry 70, 59–70 (2013).
Gudbrandsen, M. et al. Brain morphometry in 22q11.2 deletion syndrome: an exploration of differences in cortical thickness, surface area, and their contribution to cortical volume. Sci. Rep. 10, 1–12 (2020).
Pardini, D. A., Raine, A., Erickson, K. & Loeber, R. Lower amygdala volume in men is associated with childhood aggression, early psychopathic traits, and future violence. Biol. Psychiatry 75, 73–80 (2014).
Hofhansel, L. et al. Morphology of the criminal brain: gray matter reductions are linked to antisocial behavior in offenders. Brain Struct. Funct. 225, 2017–2028 (2020).
Schiffer, B. et al. Disentangling structural brain alterations associated with violent behavior from those associated with substance use disorders. Arch. Gen. Psychiatry 68, 1039–1049 (2011).
Yang, Y., Raine, A., Narr, K. L., Colletti, P. & Toga, A. W. Localization of deformations within the amygdala in individuals with psychopathy. Arch. Gen. Psychiatry 66, 986–994 (2009).
Yang, Y. et al. Volume reduction in prefrontal gray matter in unsuccessful criminal psychopaths. Biol. Psychiatry 57, 1103–1108 (2005).
Raine, A. et al. Corpus callosum abnormalities in psychopathic antisocial individuals. Arch. Gen. Psychiatry 60, 1134–1142 (2003).
Raine, A., Lencz, T., Bihrle, S., LaCasse, L. & Colletti, P. Reduced prefrontal gray matter volume and reduced autonomic activity in antisocial personality disorder. Arch. Gen. Psychiatry 57, 119–127 (2000).
Griem, J., Kolla, N. J. & Tully, J. Key challenges in neurocognitive assessment of individuals with antisocial personality disorder and psychopathy. Front. Behav. Neurosci. 16, 1007121 (2022).
Birbaumer, N. et al. Deficient fear conditioning in psychopathy: a functional magnetic resonance imaging study. Arch. Gen. Psychiatry 62, 799–805 (2005).
Gregory, S. et al. Punishment and psychopathy: a case–control functional MRI investigation of reinforcement learning in violent antisocial personality disordered men. Lancet Psychiatry 2, 153–160 (2015).
Decety, J., Skelly, L., Yoder, K. J. & Kiehl, K. A. Neural processing of dynamic emotional facial expressions in psychopaths. Soc. Neurosci. 9, 36–49 (2014).
Sebastian, C. L. et al. Neural responses to affective and cognitive theory of mind in children with conduct problems and varying levels of callous–unemotional traits. Arch. Gen. Psychiatry 69, 814–822 (2012).
Lockwood, P. L. et al. Association of callous traits with reduced neural response to others’ pain in children with conduct problems. Curr. Biol. 23, 901–905 (2013).
Walter, H. Social cognitive neuroscience of empathy: concepts, circuits, and genes. Emot. Rev. 4, 9–17 (2012).
Blair, R., Veroude, K. & Buitelaar, J. Neuro-cognitive system dysfunction and symptom sets: a review of fMRI studies in youth with conduct problems. Neurosci. Biobehav. Rev. 91, 69–90 (2018).
O’Doherty, J. P. Contributions of the ventromedial prefrontal cortex to goal‐directed action selection. Ann. N. Y. Acad. Sci. 1239, 118–129 (2011).
Hiser, J. & Koenigs, M. The multifaceted role of the ventromedial prefrontal cortex in emotion, decision making, social cognition, and psychopathology. Biol. Psychiatry 83, 638–47. (2018).
Finger, E. C. et al. Disrupted reinforcement signaling in the orbitofrontal cortex and caudate in youths with conduct disorder or oppositional defiant disorder and a high level of psychopathic traits. Am. J. Psychiatry 168, 152–162 (2011).
Decety, J., Michalska, K. J., Akitsuki, Y. & Lahey, B. B. Atypical empathic responses in adolescents with aggressive conduct disorder: a functional MRI investigation. Biol. Psychol. 80, 203–211 (2009).
Glenn, A. L., Raine, A., Yaralian, P. S. & Yang, Y. Increased volume of the striatum in psychopathic individuals. Biol. Psychiatry 67, 52–58 (2010).
Báez-Mendoza, R. & Schultz, W. The role of the striatum in social behavior. Front. Neurosci. 7, 233 (2013).
Wickens, J. R., Budd, C. S., Hyland, B. I. & Arbuthnott, G. W. Striatal contributions to reward and decision making. Ann. N. Y. Acad. Sci. 1104, 192–212 (2007).
Alegria, A. A., Radua, J. & Rubia, K. Meta-analysis of fMRI studies of disruptive behavior disorders. Am. J. Psychiatry 173, 1119–30. (2016).
Floresco, S. B., Montes, D. R., Maric, M. & van Holstein, M. Differential contributions of nucleus accumbens subregions to cue-guided risk/reward decision making and implementation of conditional rules. J. Neurosci. 38, 1901–14. (2018).
Sethi, A. et al. Emotional detachment in psychopathy: involvement of dorsal default-mode connections. Cortex 62, 11–19 (2015).
Craig, M. C. et al. Altered connections on the road to psychopathy. Mol. Psychiatry 14, 946–953 (2009).
Jones, A. P., Laurens, K. R., Herba, C. M., Barker, G. J. & Viding, E. Amygdala hypoactivity to fearful faces in boys with conduct problems and callous-unemotional traits. Am. J. Psychiatry 166, 95–102 (2009).
Lozier, L. M., Cardinale, E. M., VanMeter, J. W. & Marsh, A. A. Mediation of the relationship between callous-unemotional traits and proactive aggression by amygdala response to fear among children with conduct problems. JAMA Psychiatry 71, 627–636 (2014).
Viding, E. et al. Amygdala response to preattentive masked fear in children with conduct problems: the role of callous–unemotional traits. Am. J. Psychiatry 169, 1109–1116 (2012).
White, S. F. et al. Reduced activity within the dorsal endogenous orienting of attention network to fearful expressions in youth with disruptive behavior disorders and psychopathic traits. Dev. Psychopathol. 24, 1105–1116 (2012).
Passamonti, L. et al. Abnormal anatomical connectivity between the amygdala and orbitofrontal cortex in conduct disorder. PLoS ONE 7, e48789 (2012).
Cohn, M. D. et al. Fear conditioning, persistence of disruptive behavior and psychopathic traits: an fMRI study. Transl. Psychiatry 3, 89 (2013).
Rubia, K. et al. Disorder-specific dissociation of orbitofrontal dysfunction in boys with pure conduct disorder during reward and ventrolateral prefrontal dysfunction in boys with pure ADHD during sustained attention. Am. J. Psychiatry 166, 83–94 (2009).
Crowley, T. J. et al. Risky decisions and their consequences: neural processing by boys with Antisocial Substance Disorder. PLoS ONE 5, e12835 (2010).
Finger, E. C. et al. Disrupted reinforcement signaling in the orbitofrontal cortex and caudate in youths with conduct disorder or oppositional defiant disorder and a high level of psychopathic traits. Am. J. Psychiatry 168, 152–162 (2011).
Hosking, J. G. et al. Disrupted prefrontal regulation of striatal subjective value signals in psychopathy. Neuron 95, 221–31. e4 (2017).
Pujol, J., Batalla, I., et al. Breakdown in the brain network subserving moral judgment in criminal psychopathy. Soc. Cogn. Affect. Neurosci. 7, 917–923 (2012).
Contreras-Rodriguez, O. et al. Disrupted neural processing of emotional faces in psychopathy. Soc. Cogn. Affect. Neurosci. 9, 505–512 (2014).
Decety, J., Skelly, L. R. & Kiehl, K. A. Brain response to empathy-eliciting scenarios involving pain in incarcerated individuals with psychopathy. JAMA Psychiatry 70, 638–645 (2013).
Raine, A. Antisocial personality as a neurodevelopmental disorder. Annu. Rev. Clin. Psychol. 14, 259–89. (2018).
Lange, N., Froimowitz, M. P., Bigler, E. D., Lainhart, J. E. & Group, B. D. C. Associations between IQ, total and regional brain volumes, and demography in a large normative sample of healthy children and adolescents. Dev. Neuropsychol. 35, 296–317 (2010).
Shaw, P. et al. Intellectual ability and cortical development in children and adolescents. Nature 440, 676–679 (2006).
Cox, S. R., Ritchie, S. J., Fawns-Ritchie, C., Tucker-Drob, E. M. & Deary, I. J. Structural brain imaging correlates of general intelligence in UK Biobank. Intelligence 76, 101376 (2019).
Blair, R. Psychopathy: cognitive and neural dysfunction. Dialogues Clin. Neurosci. 15, 181–190 (2013).
Kong, X.-Z. et al. Individual differences in impulsivity predict head motion during magnetic resonance imaging. PLoS ONE 9, e104989 (2014).
Reuter, M. et al. Head motion during MRI acquisition reduces gray matter volume and thickness estimates. NeuroImage 107, 107–115 (2015).
Dosenbach, N. U. et al. Real-time motion analytics during brain MRI improve data quality and reduce costs. NeuroImage 161, 80–93 (2017).
Sui, Y., Afacan, O., Gholipour, A. & Warfield, S. K. SLIMM: slice localization integrated MRI monitoring. NeuroImage. 223, 117280 (2020).
D’Andrea, C. B. et al. Real-time motion monitoring improves functional MRI data quality in infants. Dev. Cogn. Neurosci. 55, 101116 (2022).
McCutcheon, R., Beck, K., Jauhar, S. & Howes, O. D. Defining the locus of dopaminergic dysfunction in schizophrenia: a meta-analysis and test of the mesolimbic hypothesis. Schizophr. Bull. 44, 1301–1311 (2018).
Hedges, L. V., & Olkin, I. Statistical Methods for Meta-analysis (Academic Press, 2014).
Higgins, J. P. et al. Cochrane Handbook for Systematic Reviews of Interventions (John Wiley & Sons, 2019).
Becker L. A. Effect size (ES). https://www.uv.es/~friasnav/EffectSizeBecker.pdf (2000).
Tully J. McCutcheon, RA. https://github.com/JohnTullyPsych/AntisocialStructuralVariabilityMeta (2022).
Barkataki, I., Kumari, V., Das, M., Taylor, P. & Sharma, T. Volumetric structural brain abnormalities in men with schizophrenia or antisocial personality disorder. Behav. Brain Res. 169, 239–247 (2006).
Boccardi, M. et al. Atypical nucleus accumbens morphology in psychopathy: another limbic piece in the puzzle. Int. J. Law Psychiatry 36, 157–167 (2013).
Budhiraja, M. et al. Brain structure abnormalities in young women who presented conduct disorder in childhood/adolescence. Cogn. Affect. Behav. Neurosci. 17, 869–885 (2017).
Dolan, M. C., Deakin, J. F. W., Roberts, N. & Anderson, I. M. Quantitative frontal and temporal structural MRI studies in personality-disordered offenders and control subjects. Psychiatry Res. Neuroimaging 116, 133–149 (2002).
Glenn, A. L., Yang, Y., Raine, A. & Colletti, P. No volumetric differences in the anterior cingulate of psychopathic individuals. Psychiatry Res. Neuroimaging 183, 140–143 (2010).
Huebner, T. et al. Morphometric brain abnormalities in boys with conduct disorder. J. Am. Acad. Child Adolesc. Psychiatry 47, 540–547 (2008).
Ibrahim, K. et al. Sex differences in medial prefrontal and parietal cortex structure in children with disruptive behavior. Dev. Cogn. Neurosci. 47, 100884 (2021).
Kaya, S., Yildirim, H. & Atmaca, M. Reduced hippocampus and amygdala volumes in antisocial personality disorder. J. Clin. Neurosci. 75, 199–203 (2020).
Kruesi, M. J., Casanova, M. F., Mannheim, G. & Johnson-Bilder, A. Reduced temporal lobe volume in early onset conduct disorder. Psychiatry Res. Neuroimaging 132, 1–11 (2004).
Kumari, V. et al. Reduced thalamic volume in men with antisocial personality disorder or schizophrenia and a history of serious violence and childhood abuse. Eur. Psychiatry 28, 225–234 (2013).
Laakso, M. P. et al. Prefrontal volumes in habitually violent subjects with antisocial personality disorder and type 2 alcoholism. Psychiatry Res. Neuroimaging 114, 95–102 (2002).
Narayan, V. M. et al. Regional cortical thinning in subjects with violent antisocial personality disorder or schizophrenia. Am. J. Psychiatry 164, 1418–1427 (2007).
Noordermeer, S. D. S. et al. Structural brain abnormalities of attention-deficit/hyperactivity disorder with oppositional defiant disorder. Biol. Psychiatry 82, 642–650 (2017).
Sebastian, C. L. et al. Grey matter volumes in children with conduct problems and varying levels of callous-unemotional traits. J. Abnorm. Child Psychol. 44, 639–649 (2016).
Tiihonen, J. et al. Brain anatomy of persistent violent offenders: more rather than less. Psychiatry Res. Neuroimaging 163, 201–212 (2008).
Vetter, N. C., Backhausen, L. L., Buse, J., Roessner, V. & Smolka, M. N. Altered brain morphology in boys with attention deficit hyperactivity disorder with and without comorbid conduct disorder/oppositional defiant disorder. Hum. Brain Mapp. 41, 973–983 (2020).
Wallace, G. L. et al. Cortical and subcortical abnormalities in youths with conduct disorder and elevated callous-unemotional traits. J. Am. Acad. Child Adolesc. Psychiatry 53, 456–465 (2014).
Acknowledgements
R.A.M.’s work is funded by a Wellcome Clinical Research Career Development Fellowship (224625/Z/21/Z). None of the other authors received funding towards this work.
Author information
Authors and Affiliations
Contributions
J.T. and R.A.M. conceived the idea. J.T., B.C. and B.G. performed the literature search and cross-checking of papers. J.T. performed the analyses, with input from R.A.M. J.T. wrote the initial draft. J.T., B.C., B.G., J.G., N.B., R.J.B. and R.A.M. all provided critical analysis on scientific content on this and further drafts.
Corresponding author
Ethics declarations
Competing interests
R.A.M. has received honoraria for educational talks from Otsuka and Janssen. None of the other authors has any conflict of interest, financial or otherwise, to disclose.
Peer review
Peer review information
Nature Mental Health thanks Nathaniel Anderson, Olivia Choy and Natalia Tesli for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
All supplementary text and figures.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tully, J., Cross, B., Gerrie, B. et al. A systematic review and meta-analysis of brain volume abnormalities in disruptive behaviour disorders, antisocial personality disorder and psychopathy. Nat. Mental Health 1, 163–173 (2023). https://doi.org/10.1038/s44220-023-00032-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s44220-023-00032-0