Abstract
Acute myocardial infarction (MI) can be triggered by heat exposure, but it remains unknown whether patients taking certain cardiovascular medications have elevated vulnerability. Based on a validated and complete registration of all 2,494 MI cases in Augsburg, Germany, during warm seasons (May to September) from 2001 to 2014, here we show that heat-related non-fatal MI risk was elevated among users of anti-platelet medication and beta-receptor blockers, respectively, but not among non-users, with significant differences between users and non-users. We also found that these effect modifications were stronger among younger patients (25–59 years), who had a lower prevalence of pre-existing coronary heart disease (CHD, a potential confounder by indication), than among older patients (60–74 years), who had a higher prevalence of pre-existing CHD. Users of these medications may be more vulnerable than non-users to non-fatal MI risk due to heat exposure. Further research is needed to disentangle effect modification by medication use from effect modification by pre-existing CHD.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
All data needed to evaluate the conclusions in the paper are included in the paper. Data were collected within the MONICA/KORA MI registry and cannot be made publicly available because the patient consent did not include such an agreement. However, data may be made available for selected research questions and researchers upon reasonable request to the authors. The timeframe for response to requests from the authors is 4 weeks. Please contact C.M. by email: christine.meisinger@med.uni-augsburg.de. The homepage of the Chair of Epidemiology is http://www.uni-augsburg.de/med/epidemiologie.
Code availability
R code for this analysis is available at https://github.com/CHENlab-Yale/Heat_MI_Medication.
References
Chen, K. et al. Temporal variations in the triggering of myocardial infarction by air temperature in Augsburg, Germany, 1987–2014. Eur. Heart J. 40, 1600–1608 (2019).
Claeys, M. J., Rajagopalan, S., Nawrot, T. S. & Brook, R. D. Climate and environmental triggers of acute myocardial infarction. Eur. Heart J. 38, 955–960 (2017).
Wolf, K. et al. Air temperature and the occurrence of myocardial infarction in Augsburg, Germany. Circulation 120, 735–742 (2009).
Schneider, A., Rückerl, R., Breitner, S., Wolf, K. & Peters, A. Thermal control, weather, and aging. Curr. Environ. Health Rep. 4, 21–29 (2017).
Liu, L. et al. Associations between air temperature and cardio-respiratory mortality in the urban area of Beijing, China: a time-series analysis. Environ. Health 10, 51 (2011).
Kalisch Ellett, L. M., Pratt, N. L., Le Blanc, V. T., Westaway, K. & Roughead, E. E. Increased risk of hospital admission for dehydration or heat-related illness after initiation of medicines: a sequence symmetry analysis. J. Clin. Pharm. Ther. 41, 503–507 (2016).
Hajat, S., O’Connor, M. & Kosatsky, T. Health effects of hot weather: from awareness of risk factors to effective health protection. Lancet 375, 856–863 (2010).
Son, J., Liu, J. C. & Bell, M. L. Temperature-related mortality: a systematic review and investigation of effect modifiers. Environ. Res. Lett. 14, 073004 (2019).
Chen, K. et al. Projection of temperature-related myocardial infarction in Augsburg, Germany. Dtsch. Arztebl. Int. 116, 521–527 (2019).
De Blois, J. et al. The effects of climate change on cardiac health. Cardiology 131, 209–217 (2015).
Bruning, R. S., Dahmus, J. D., Kenney, W. L. & Alexander, L. M. Aspirin and clopidogrel alter core temperature and skin blood flow during heat stress. Med. Sci. Sports Exerc. 45, 674–682 (2013).
Argaud, L. et al. Short- and long-term outcomes of heatstroke following the 2003 heat wave in Lyon, France. Arch. Intern. Med. 167, 2177–2183 (2007).
Kuch, B. Der Einfluss des Klimawandels auf das Auftreten von Herz-Kreislauf-Erkrankungen. Handlungsansätze und die besondere Herausforderung durch Arzneimittel-wechselwirkungen. In Versorgungs-Report: Klima und Gesundheit (eds Günster, C., et al.) (Medizinisch Wissenschaftliche Verlagsgesellschaft, 2021).
Löwel, H., Meisinger, C., Heier, M. & Hörmann, A. The population-based acute myocardial infarction (AMI) registry of the MONICA/KORA study region of Augsburg. Gesundheitswesen 67, 31–37 (2005).
Kuch, B. et al. 20-year trends in clinical characteristics, therapy and short‐term prognosis in acute myocardial infarction according to presenting electrocardiogram: the MONICA / KORA AMI Registry (1985–2004). J. Intern. Med. 264, 254–264 (2008).
Acknowledgements
This work was supported by the Deutsche Stiftung für Herzforschung (German Foundation of Heart Research) (grant no. F/51/15). The KORA study was initiated and financed by the Helmholtz Zentrum München–German Research Center for Environmental Health, which is funded by the German Federal Ministry of Education and Research (BMBF) and by the State of Bavaria. This research also received support from the Faculty of Medicine, University of Augsburg, and University Hospital Augsburg. Since 2000, the MI data collection has been co-financed by the German Federal Ministry of Health to provide population-based MI morbidity data for the official German Health Report (https://www.gbe-bund.de/gbe/). A.P. was supported by the German Centre for Cardiovascular Research (DZHK) and by the BMBF. A.S. was supported by the European Union’s Horizon 2020 Project EXHAUSTION (grant agreement No. 820655). R.D. received funding support from the High Tide Foundation.
Author information
Authors and Affiliations
Consortia
Contributions
K.C. and A.S. conceived the study design. K.C. performed the formal analysis, investigation and drafting of the manuscript. R.D., S.B., B.K., C.M. and A.S. contributed to manuscript preparation and editing. R.D., S.B., K.W. and A.S. assisted with the statistical methodology. J.L., T.S., M.H., W.v.S., B.K., C.M. and A.P. contributed to data collection and management. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Cardiovascular Research thanks Francesco Sera, Sadeer Al-Kindi and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
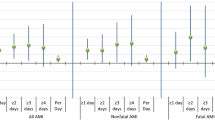
Extended Data Fig. 1 Heat-related risks of non-fatal myocardial infarction (MI) stratified by intake/non-intake of both antiplatelet medication and beta-receptor blockers (both versus neither) in Augsburg, Germany, during the warm seasons from 2001 to 2014.
The odds ratio (OR) for heat exposure, which is defined as the 95th percentile of temperature (24.2 °C) relative to the minimum MI risk temperature (7.5 °C) (n = 1,911). Data are presented as point estimates of OR ± 1.96 standard error (that is, 95% confidence intervals). Asterisk indicates statistical significance (two-sided p-value =0.011; multiple comparisons were not adjusted) of the differences in risk estimates between users and non-users, based on the z score calculated using the coefficients and standard errors for users and non-users. Participants taking only one of these medications were excluded from this analysis; (b) Exposure-response curves for the temperature-MI relationship stratified by intake/non-intake of both antiplatelet and beta-receptor blockers. Solid lines represent the point estimates of OR; shaded areas represent the 95% confidence intervals. Solid vertical line is the MMIT and dashed vertical line is the 95th percentile of temperature.
Extended Data Fig. 2 Sensitivity analysis of heat-related risks of non-fatal myocardial infarction (MI) stratified by medication intake in Augsburg, Germany, during the warm seasons from 2001 to 2014.
The odds ratio (OR) is for the 95th percentile of temperature (24.2 °C) relative to the minimum MI risk temperature (MMIT; 7.5 °C). Data are presented as point estimates of OR ± 1.96 standard error (that is, 95% confidence intervals). (a) Using the 90th percentile temperature to define heat exposure (n = 2,494). Asterisks indicate statistical significance (two-sided p-value = 0.032 and 0.035 for antiplatelet and beta-receptor blockers intake, respectively; multiple comparisons were not adjusted) of the differences in risk estimates between users and non-users of a specific medication, based on the z score calculated using the coefficients and standard errors for users and non-users. (b) Using the 97.5th percentile temperature to define heat exposure (n = 2,494). Asterisks indicate statistical significance (two-sided p-value = 0.017 for beta-receptor blockers intake; multiple comparisons were not adjusted). (c) Controlling for relative humidity nonlinearly using a natural cubic spline with 3 degrees of freedom (df) (n = 2,494). Asterisks indicate statistical significance (two-sided p-value = 0.043 and 0.019 for antiplatelet and beta-receptor blockers intake, respectively; multiple comparisons were not adjusted). (d) Additionally adjusting for current day PM10 (inhalable particulate matter) concentration (n = 1,729). Asterisks indicate statistical significance (two-sided p-value = 0.014 and 0.011 for antiplatelet and beta-receptor blockers intake, respectively; multiple comparisons were not adjusted). (e) Additionally adjusting for current day NO2 (nitrogen dioxide) concentration (n = 2,118). Asterisks indicate statistical significance (two-sided p-value = 0.021 and 0.011 for antiplatelet and beta-receptor blockers intake, respectively; multiple comparisons were not adjusted). The 90th, 95th, and 97.5th represents the 90th, 95th, and 97.5th percentile of temperature, respectively.
Extended Data Fig. 3 Sensitivity analysis of heat-related risks of non-fatal myocardial infarction (MI) at a maximum lag of 3 days stratified by medication intake in Augsburg, Germany, during the warm seasons from 2001 to 2014.
(a) Effect modification by six medication types with more than 10% of intake frequency among the MI survivors (n = 2,124). The odds ratio (OR) is for the 95th percentile of temperature (95th; 24.2 °C) relative to the minimum MI risk temperature (MMIT; 7.5 °C). Data are presented as point estimates of OR ± 1.96 standard error (that is, 95% confidence intervals). Two-sided P-value (0.060 and 0.028 for antiplatelet and beta-receptor blockers intake, respectively; multiple comparisons were not adjusted) indicates the statistical significance of the difference in risk estimates between users and non-users of a specific medication, based on the z score calculated using the coefficients and standard errors for users and non-users. (b) Exposure-response curves for the temperature-MI relationship stratified by antiplatelet or beta-receptor blockers intake. Solid lines represent the point estimates of OR; shaded areas represent the 95% confidence intervals. Solid vertical lines are the minimum MI temperatures (MMIT; 7.5 °C) and dashed vertical lines are the 95th percentile of temperature (24.2 °C).
Extended Data Fig. 4 Lag-response curves for heat-related risks of non-fatal myocardial infarction stratified by antiplatelet and beta-receptor blockers intake.
The odds ratio (OR) is for the 95th percentile of temperature (24.2 °C) relative to the minimum MI risk temperature (MMIT; 7.5 °C). Solid lines represent the point estimates of OR; shaded areas represent the 95% confidence intervals.
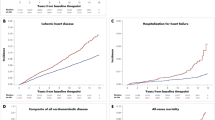
Extended Data Fig. 5 Heat-related risks of non-fatal myocardial infarction (MI) stratified by history of diabetes, hypertension, or pre-existing coronary heart disease in Augsburg, Germany, during the warm seasons from 2001 to 2014.
The odds ratio (OR) is for the 95th percentile of temperature (95th; 24.2 °C) relative to the minimum MI risk temperature (MMIT; 7.5 °C) (n = 2,136). Data are presented as point estimates of OR ± 1.96 standard error (that is, 95% confidence intervals). Asterisk indicates statistical significance (two-sided p-value = 0.001 for patients with pre-existing coronary heart disease; multiple comparisons were not adjusted) of the difference in risk estimates between users and non-users of a specific medication, based on the z score calculated using the coefficients and standard errors for users and non-users.
Supplementary information
Supplementary Information
Notes on the consortium members
Source data
Source Data Fig. 1
Statistical source data.
Source Data Fig. 2
Statistical source data.
Source Data Extended Data Fig. 1
Statistical source data.
Source Data Extended Data Fig. 2
Statistical source data.
Source Data Extended Data Fig. 3
Statistical source data.
Source Data Extended Data Fig. 5
Statistical source data.
Rights and permissions
About this article
Cite this article
Chen, K., Dubrow, R., Breitner, S. et al. Triggering of myocardial infarction by heat exposure is modified by medication intake. Nat Cardiovasc Res 1, 727–731 (2022). https://doi.org/10.1038/s44161-022-00102-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s44161-022-00102-z
This article is cited by
-
Hitze und kardiovaskuläres Risiko
Die Kardiologie (2024)
-
Racial/ethnic disparities in PM2.5-attributable cardiovascular mortality burden in the United States
Nature Human Behaviour (2023)
-
Diabetes and climate change: current evidence and implications for people with diabetes, clinicians and policy stakeholders
Diabetologia (2023)