Abstract
The heart is a highly metabolic organ that uses multiple energy sources to meet its demand for ATP production. Diurnal feeding–fasting cycles result in fluctuations in substrate availability, which, together with increased energetic demand during the active period, impose a need for rhythmic cardiac metabolism. The nuclear receptors REV-ERBα and REV-ERBβ are essential repressive components of the molecular circadian clock and major regulators of metabolism. To investigate their role in the heart, here we generated mice with cardiomyocyte (CM)-specific deletion of both Rev-erb genes (Nr1d1/2), which died prematurely due to dilated cardiomyopathy. Loss of REV-ERBs markedly downregulated expression of fatty acid-oxidation genes before overt pathology, which was mediated by induction of the transcriptional repressor E4BP4, a direct target of cardiac REV-ERBs. E4BP4 directly controls circadian expression of Nampt and its biosynthetic product NAD+ via distal cis regulatory elements. Thus, REV-ERB-mediated E4BP4 repression is required for Nampt expression and NAD+ production by the salvage pathway. Together, these results highlight the indispensable role of circadian REV-ERBs in cardiac gene expression, metabolic homeostasis and function.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
The authors declare that the data supporting the findings of this study are available within the paper and its Supplementary Information. The RNA-seq, Cut&Run and ChIP–seq datasets reported in this paper have been deposited in the Gene Expression Omnibus under the accession number GSE153014. Source data are provided with this paper.
References
Kummitha, C. M., Kalhan, S. C., Saidel, G. M. & Lai, N. Relating tissue/organ energy expenditure to metabolic fluxes in mouse and human: experimental data integrated with mathematical modeling. Physiol. Rep. 2, e12159 (2014).
Cederroth, C. R. et al. Medicine in the fourth dimension. Cell Metab. 30, 238–250 (2019).
Dierickx, P., van Laake, L. W. & Geijsen, N. Circadian clocks: from stem cells to tissue homeostasis and regeneration. EMBO Rep. 19, 18–28 (2017).
Dierickx, P. et al. Circadian rhythms in stem cell biology and function. In Stem Cells and Cardiac Regeneration 57–78 (Springer, 2015).
Crnko, S., Pré, Du,B. C., Sluijter, J. P. G. & van Laake, L. W. Circadian rhythms and the molecular clock in cardiovascular biology and disease. Nat. Rev. Cardiol. 16, 437–447 (2019).
Rana, S., Prabhu, S. D. & Young, M. E. Chronobiological influence over cardiovascular function: the good, the bad, and the ugly. Circ. Res. 126, 258–279 (2020).
Ramsey, K. M. et al. Circadian clock feedback cycle through NAMPT-mediated NAD+ biosynthesis. Science 324, 651–654 (2009).
Nakahata, Y., Sahar, S., Astarita, G., Kaluzova, M. & Sassone-Corsi, P. Circadian control of the NAD+ salvage pathway by CLOCK–SIRT1. Science 324, 654–657 (2009).
Imai, S.-I. & Guarente, L. It takes two to tango: NAD+ and sirtuins in aging/longevity control. NPJ Aging Mech. Dis. 2, 16017 (2016).
Rudic, R. D. et al. BMAL1 and CLOCK, two essential components of the circadian clock, are involved in glucose homeostasis. PLoS Biol. 2, e377 (2004).
Young, M. E. et al. Cardiomyocyte-specific BMAL1 plays critical roles in metabolism, signaling, and maintenance of contractile function of the heart. J. Biol. Rhythms 29, 257–276 (2014).
Schroder, E. A. et al. The cardiomyocyte molecular clock, regulation of Scn5a, and arrhythmia susceptibility. Am. J. Physiol. Cell Physiol. 304, C954–C965 (2013).
Lefta, M., Campbell, K. S., Feng, H.-Z., Jin, J.-P. & Esser, K. A. Development of dilated cardiomyopathy in Bmal1-deficient mice. Am. J. Physiol. Heart Circ. Physiol. 303, H475–H485 (2012).
Bass, J. & Lazar, M. A. Circadian time signatures of fitness and disease. Science 354, 994–999 (2016).
Hoon Kim, Y. & Lazar, M. A. Transcriptional control of circadian rhythms and metabolism: a matter of time and space. Endocr. Rev. 41, 707–732 (2020).
Yin, L. & Lazar, M. A. The orphan nuclear receptor Rev-erbα recruits the N-CoR/histone deacetylase 3 corepressor to regulate the circadian Bmal1 gene. Mol. Endocrinol. 19, 1452–1459 (2005).
Stujanna, E. N. et al. Rev-erb agonist improves adverse cardiac remodeling and survival in myocardial infarction through an anti-inflammatory mechanism. PLoS ONE 12, e0189330 (2017).
Alibhai, F. J. et al. Disrupting the key circadian regulator CLOCK leads to age-dependent cardiovascular disease. J. Mol. Cell. Cardiol. 105, 24–37 (2017).
Zhang, L. et al. REV-ERBα ameliorates heart failure through transcription repression. JCI Insight 2, e95177 (2017).
Dierickx, P. et al. SR9009 has REV-ERB-independent effects on cell proliferation and metabolism. Proc. Natl Acad. Sci. USA 3, 12147–12152 (2019).
Agah, R. et al. Gene recombination in postmitotic cells. Targeted expression of Cre recombinase provokes cardiac-restricted, site-specific rearrangement in adult ventricular muscle in vivo. J. Clin. Invest. 100, 169–179 (1997).
Guan, D. et al. The hepatocyte clock and feeding control chronophysiology of multiple liver cell types. Science 369, 1388–1394 (2020).
Zhang, Y. et al. Gene regulation. Discrete functions of nuclear receptor Rev-erbα couple metabolism to the clock. Science 348, 1488–1492 (2015).
Zhang, R., Lahens, N. F., Ballance, H. I., Hughes, M. E. & Hogenesch, J. B. A circadian gene expression atlas in mammals: implications for biology and medicine. Proc. Natl Acad. Sci. USA 111, 16219–16224 (2014).
McGinnis, G. R. et al. Genetic disruption of the cardiomyocyte circadian clock differentially influences insulin-mediated processes in the heart. J. Mol. Cell. Cardiol. 110, 80–95 (2017).
Meyer-Roxlau, S. et al. Differential regulation of protein phosphatase 1 (PP1) isoforms in human heart failure and atrial fibrillation. Basic Res. Cardiol. 112, 43 (2017).
Skene, P. J. & Henikoff, S. An efficient targeted nuclease strategy for high-resolution mapping of DNA binding sites. eLife 6, e21856 (2017).
Creyghton, M. P. et al. Histone H3K27ac separates active from poised enhancers and predicts developmental state. Proc. Natl Acad. Sci. USA 107, 21931–21936 (2010).
Rada-Iglesias, A. et al. A unique chromatin signature uncovers early developmental enhancers in humans. Nature 470, 279–283 (2011).
Madsen, J. G. S. et al. Integrated analysis of motif activity and gene expression changes of transcription factors. Genome Res. 28, 243–255 (2018).
Mei, S. et al. Cistrome Data Browser: a data portal for ChIP–seq and chromatin accessibility data in human and mouse. Nucleic Acids Res. 45, D658–D662 (2017).
Oakley, R. H. et al. Cardiomyocyte glucocorticoid and mineralocorticoid receptors directly and antagonistically regulate heart disease in mice. Sci. Signal. 12, eaau9685 (2019).
Preitner, N. et al. The orphan nuclear receptor REV-ERBα controls circadian transcription within the positive limb of the mammalian circadian oscillator. Cell 110, 251–260 (2002).
Rey, G. et al. Genome-wide and phase-specific DNA-binding rhythms of BMAL1 control circadian output functions in mouse liver. PLoS Biol. 9, e1000595 (2011).
Mia, S. et al. Differential effects of REV-ERBα/β agonism on cardiac gene expression, metabolism, and contractile function in a mouse model of circadian disruption. Am. J. Physiol. Heart Circ. Physiol. 318, H1487–H1508 (2020).
Weng, Y.-J. et al. E4BP4 is a cardiac survival factor and essential for embryonic heart development. Mol. Cell. Biochem. 340, 187–194 (2010).
Monnier, V. et al. dJun and Vri/dNFIL3 are major regulators of cardiac aging in Drosophila. PLoS Genet. 8, e1003081 (2012).
Walker, M. A. & Tian, R. Raising NAD in heart failure: time to translate? Circulation 137, 2274–2277 (2018).
Rosa-Garrido, M. et al. High-resolution mapping of chromatin conformation in cardiac myocytes reveals structural remodeling of the epigenome in heart failure. Circulation 136, 1613–1625 (2017).
Yoshitane, H. et al. Functional D-box sequences reset the circadian clock and drive mRNA rhythms. Commun. Biol. 2, 300 (2019).
Covarrubias, A. J., Perrone, R., Grozio, A. & Verdin, E. NAD+ metabolism and its roles in cellular processes during ageing. Nat. Rev. Mol. Cell Biol. 22, 119–141 (2021).
Koronowski, K. B. et al. Defining the independence of the liver circadian clock. Cell 177, 1448–1462 (2019).
Nakao, T. et al. Impact of heart-specific disruption of the circadian clock on systemic glucose metabolism in mice. Chronobiol. Int. 35, 499–510 (2018).
Durgan, D. J. et al. Evidence suggesting that the cardiomyocyte circadian clock modulates responsiveness of the heart to hypertrophic stimuli in mice. Chronobiol. Int. 28, 187–203 (2011).
Kohsaka, A. et al. The circadian clock maintains cardiac function by regulating mitochondrial metabolism in mice. PLoS ONE 9, e112811 (2014).
Bray, M. S. et al. Disruption of the circadian clock within the cardiomyocyte influences myocardial contractile function, metabolism, and gene expression. Am. J. Physiol. Heart Circ. Physiol. 294, H1036–H1047 (2008).
Mermet, J., Yeung, J. & Naef, F. Oscillating and stable genome topologies underlie hepatic physiological rhythms during the circadian cycle. PLoS Genet. 17, e1009350 (2021).
Motomura, Y. et al. The transcription factor E4BP4 regulates the production of IL-10 and IL-13 in CD4+ T cells. Nat. Immunol. 12, 450–459 (2011).
Bugge, A. et al. Rev-erbα and Rev-erbβ coordinately protect the circadian clock and normal metabolic function. Genes Dev. 26, 657–667 (2012).
Luongo, T. S. et al. SLC25A51 is a mammalian mitochondrial NAD+ transporter. Nature 588, 174–179 (2020).
Kim, D., Langmead, B. & Salzberg, S. L. HISAT: a fast spliced aligner with low memory requirements. Nat. Methods 12, 357–360 (2015).
Pertea, M. et al. StringTie enables improved reconstruction of a transcriptome from RNA-seq reads. Nat. Biotechnol. 33, 290–295 (2015).
Liao, Y., Smyth, G. K. & Shi, W. featureCounts: an efficient general purpose program for assigning sequence reads to genomic features. Bioinformatics 30, 923–930 (2014).
Love, M. I., Huber, W. & Anders, S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 15, 550 (2014).
Skene, P. J., Henikoff, J. G. & Henikoff, S. Targeted in situ genome-wide profiling with high efficiency for low cell numbers. Nat. Protoc. 13, 1006–1019 (2018).
Zhang, Y. et al. Model-based analysis of ChIP–seq (MACS). Genome Biol. 9, R137 (2008).
Xingwang, L. et al. Long-read ChIA-PET for base-pair-resolution mapping of haplotype-specific chromatin interactions. Nat. Protoc. 12, 899–915 (2017).
Martin, M. Cutadapt removes adapter sequences from high-throughput sequencing reads. EMBnet j. 17, 10–12 (2011).
Li, H. Aligning sequence reads, clone sequences and assembly contigs with BWA-MEM. Preprint at https://arxiv.org/abs/1303.3997 (2013).
Li, H. et al. The Sequence Alignment/Map format and SAMtools. Bioinformatics 25, 2078–2079 (2009).
Yu, G., Wang, L.-G. & He, Q.-Y. ChIPseeker: an R/Bioconductor package for ChIP peak annotation, comparison and visualization. Bioinformatics 31, 2382–2383 (2015).
Heinz, S. et al. Simple combinations of lineage-determining transcription factors prime cis-regulatory elements required for macrophage and B cell identities. Mol. Cell 38, 576–589 (2010).
Sakamoto, T. et al. A critical role for estrogen-related receptor signaling in cardiac maturation. Circ. Res. 120, 1685–1702 (2020).
Liberzon, A. et al. The molecular signatures database (MSigDB) hallmark gene set collection. Cell Syst. 1, 417–425 (2015).
Ryan, M. et al. GIGGLE: a search engine for large-scale integrated genome analysis. Nat. Methods 15, 123–126 (2018).
Durand, N. C. et al. Juicebox provides a visualization system for Hi-C contact maps with unlimited zoom. Cell Syst. 3, 99–101 (2016).
Acknowledgements
We thank L. Cheng for help with histology. We thank the Functional Genomics Core of the Penn Diabetes Research Center (DK19525), the Mouse Cardiovascular Phenotyping Core (S. Shewale) at the Penn Cardiovascular Institute and the Electron Microscopy Resource Laboratory Core. This work was supported by NIH R01DK45586, the JPB Foundation and the Cox Institute for Medical Research (M.A.L.); RO1 DK111495 and the Department of Defense (W81XWH20-1-0042 and W81XWH20-1-0089) (L.P.); NIH R01HL058493, R01HL128349 and R01HL151345 (D.P.K.); NIH R01 DK098656 (J.A.B.); and R01HL149159 (M.E.Y.). P.D. was supported by a Netherlands Heart Institute postdoctoral fellowship and an American Heart Association postdoctoral fellowship (20POST35210738); M.W.V. was supported by an EMBO long-term fellowship (ALTF 540-2018) and an American Heart Association postdoctoral fellowship (836074); Y.X. was supported by an American Heart Association postdoctoral fellowship (827529); T.S.L. was supported by F32HL145923; and A.K.H. was supported by F32DK122684-01A1.
Author information
Authors and Affiliations
Contributions
P.D. and M.A.L. conceived and designed the overall study. P.D., K.Z., Y.X., C.J., M.W.V., under the supervision of G.A.B., J.Z., under the supervision of L.P., and H.C.B.N. contributed to next-generation sequencing experiments and bioinformatic analyses. T.S.L. performed NAD+ measurements under the supervision of J.A.B. P.D., B.J.C., A.K.H. and B.K. helped with circadian sampling. P.D. and B.J.C. performed gene expression measurements, western blotting, cell culture experiments, animal caretaking, reporter assays and metabolic experiments. T.Y., under the supervision of D.P.K., and I.M.-P. assisted with echocardiography experiments. S.M. and M.L. (under the supervision of M.E.Y.) performed RT–qPCR and western blots on CM-specific Bmal1-KO, E4bp4-KO and Bmal1;E4bp4-DKO hearts. A.D. assisted with the generation of CM-specific E4bp4-KO mice. P.D. and M.A.L. wrote the manuscript with input from all authors.
Corresponding authors
Ethics declarations
Competing interests
M.A.L. receives research support from Pfizer for unrelated work; serves as an advisory board member for Pfizer and Flare Therapeutics; has consulted for Novartis, Madrigal, Calico and Third Rock; and holds equity in KDAC Therapeutics and Flare Therapeutics. D.P.K. serves as an advisory board member for Pfizer and Amgen. J.A.B. is an inventor on a patent for using NAD+ precursors in liver injury, is a consultant for Pfizer and Cytokinetics and has received research funding and materials from Elysium Health and Metro International Biotech, both of which have an interest in NAD+ precursors. No funds or materials from Elysium Health and Metro International Biotech were used to generate any data for this study. The remaining authors declare no competing interests.
Additional information
Peer review information Nature Cardiovascular Research thanks Junichi Sadoshima and Li Wang for their contribution to the peer review of this work.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
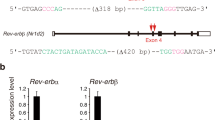
Extended Data Fig. 1 Additional validation of CM-RevDKO.
a, Immunoblot for BMAL1 with quantification from control (αMHC-Cre-) vs CM-RevDKO (αMHC-Cre + ) hearts from 2-month-old male mice (n = 2/timepoint/genotype). b, Relative mRNA expression in control vs CM-RevDKO hearts from 2-month-old male mice (n = 3 hearts/genotype/timepoint except for n = 2 for ZT2 and n = 4 for ZT22 in CM-RevDKO) and c, young and old WT mice (n = 3/genotype). n represents biologically independent replicates. Data are presented as mean ± SEM, except for a. ns, non significant; * P < 0.05; ** P < 0.01; *** P < 0.001; ****P < 0.0001 by 2-way ANOVA (exact P values are provided in the Source Data).
Extended Data Fig. 2 Age-dependent impairment of cardiac structure and function in CM-RevDKO mice.
a, Birth rates for CM-RevDKO and littermate control animals. b, Locomotor activity and c, food consumption of 2-month-old male control (n = 3) and CM-RevDKO (n = 5) mice housed under 12:12 light:dark conditions. d, Body weight (in grams) of male control and CM-RevDKO mice at 2 (n = 17 for control and n = 34 for CM-RevDKO)-4 (n = 8 for control and n = 14 for CM-RevDKO)-6 (n = 8 for control and n = 11 for CM-RevDKO) months of age. e, Blood glucose concentrations of 6-months old male control (n = 6) and CM-RevDKO (n = 11) mice that underwent glucose tolerance test (GTT) and f, insulin tolerance test (ITT) (n = 6 for control and n = 10 for CM-RevDKO). g, Biventricular to body weight (BVW/BW) ratios of from control (n = 5) and CM-RevDKO (n = 6) hearts. h, Cardiomyocyte size assesment of 6-month old control and CM-RevDKO hearts. Representative images (cardiac sarcolemma stained by WGA in red, nuclei by DAPI = blue) of 11 control and 9 CM-RevDKO hearts are shown. Scale bars, 50μM. i, Cardiac structure (LVIDd/s: Left ventricular internal diameter during diastole/systole) and function (EF: Ejection fraction and FS: Fractional shortening) data from 2-month-old control and CM-RevDKO mice obtained through echocardiagraphy (n = 4/genotype). j, Echocardiographic parameters from control vs CM-RevDKO mice age 2 months (n = 4/genotype) versus 6 months (n = 11 for control and n = 8 for CM-RevDKO). (HR) Heart rate; (LVPWs/d) Left ventricular posterior wall during systole/diastole; (IVSs/d) Interventricular septum thickness during systole/diastole; (RWT) Relative wall thickness. k, Masson’s trichrome and l, TUNEL staining (green) on hearts of 6-month-old control and CM-RevDKO mice. Nuclei are stained with DAPI (blue). Representative images of n = 11 hearts for control and n = 9 hearts for CM-RevDKO are shown. Scale bars, (k) 50μM and (l), 100μM. n represents biologically independent replicates unless otherwise indicated. Data are presented as mean ± SEM. ns, non significant; *P < 0.05; ***P < 0.001 by 2-sided Student’s t test (exact P values are provided in the Source Data).
Extended Data Fig. 3 CM-RevDKO causes tissue-specific deregulated expression of circadian genes.
a, Circadian Rev-erbα/β and Bmal1 mRNA expression in 2-month-old male control hearts (n = 5 timepoint, except for ZT7, n = 4 and ZT10, n = 6). b, Left: Venn diagram showing overlap between DEGs in CM-RevDKO hearts and hepatocyte-specific Rev-erb DKO (HepDKO) livers22 (at ZT10). Right: relative mRNA expression of commonly (in both CM-RevDKO and Hep-RevDKO) deregulated clock genes in CM-RevDKO vs control hearts (n = 3 hearts/genotype, harvested at ZT10). c, qRT-PCR validation of genes derepressed upon CM-RevDKO in the heart of 2-month-old male mice (n = 5 for control and n = 6 for CM-RevDKO). d, Left: Venn diagram showing overlap between cardiac oscillators published in24 and all DEGs in CM-RevDKO that were assessed in24. Right: phase plots of rhythmic, differentially expressed genes identified on the left. n represents biologically independent replicates. Data are presented as mean ± SEM. Adj. P values in b were calculated by DESeq2. ***P < 0.001; ****P < 0.0001 by 2-sided Student’s t-test (exact P values are provided in the Source Data).
Extended Data Fig. 4 Mitochondrial size is affected in CM-RevDKO cardiomyocytes.
a, Relative Ppp1r1b mRNA expression in CM-RevDKO (n = 6) vs control (n = 5) hearts from 2-month-old male mice. b, Immunoblot for DARPP-32 in CM-RevDKO vs control hearts. c, Scatter plot and histogram of mitochondria area for ventricular CMs in control and CM-RevDKO hearts from 6-month-old male mice based on electron microscopy images (n = 86 mitochondria for control, measured from 5 images, n = 90 mitochondria for CM-RevDKO, measured from 7 images). d, Left: scatter plot of mitochondria area for ventricular CMs in control and CM-RevDKO hearts from 2-month-old mice. Right: Electron micrographs of ventricular tissue from control and CM-RevDKO hearts at 2 months (n = 108 mitochondria for control, measured from 7 images, n = 100 mitochondria for CM-RevDKO, measured from 9 images). Scale bars, 1μM. e, Relative levels of mitochondrial DNA quantified by RT-qPCR. mtCo1/2 and mtNd1 levels were normalized to nuclear genomic βActin (n = 3/genotype). n represents biologically independent replicates unless otherwise indicated. Data are presented as mean ± s.e.m. ns:, non significant; *P < 0.05; ***P < 0.001; ****P < 0.0001 by 2-sided Student’s t-test (exact P values are provided in the Source Data).
Extended Data Fig. 5 Characterization of the 3xHA-REV-ERBα cistrome in the heart.
a, Venn diagram showing the overlap between the downregulated differentially expressed genes (DEGs) in CM-RevDKO hearts and up/downregulated genes in cardiomyocyte-specific glucocorticoid receptor (GR) KO hearts32. b, Pearson correlation plots comparing 3xHA ChIP-seq replicate samples. c, Pie chart of annotated cardiac 3xHA-REV-ERBα ChIP-seq peaks. d, Results of motif search at 3xHA-REV-ERBα ChIP-seq peaks and enhancers that displayed increased H3K27ac Cut&Run signal (FC > 2) in CM-RevDKO vs control cardiomyocytes as reported by HOMER. e, Venn diagram showing overlap between DEGs in CM-RevDKO vs control hearts and annotated peaks from the cardiac 3xHA-REV-ERBα cistrome (at ZT10). f, ChIP-seq, Cut&Run and RNA-seq read distribution for REV-ERBα and H3K27ac near derepressed REV-ERBα canonical target genes Bmal1 and g, Cry1 and h, output genes p21 and Fbn2. i, Immunoblot and quantification for FLAG and REV-ERBα from DsRed (control) vs FLAG-Rev-erbα overexpressing plasmid transfected C2C12 cells (n = 2 independently transfected wells/condition). Significance of overlap in e is calculated via a hypergeometric test without multiple testing correction.
Extended Data Fig. 6 E4BP4-based repression is a unifying mechanism to explain transcriptional changes and cardiomyopathy common to the cardiac-specific loss of BMAL1 or REV-ERBs.
a, Results of motif search at cardiac E4BP4 ChIP-seq peaks (Control at ZT22) as reported by HOMER. b, Pie chart of annotated cardiac E4BP4 ChIP-seq peaks (control ZT22). c, Venn diagram showing overlap between annotated peaks from the cardiac control (at ZT22) and CM-RevDKO (at ZT10 and ZT22) E4BP4 cistromes. d, ChIP-seq, Cut&Run and RNA-seq read distribution for E4BP4 and H3K27ac near identified E4BP4 target genes in control and CM-RevDKO hearts. e, Overlap between upregulated and g, downregulated genes in CM-RevDKO hearts and cardiomyocyte-specific Bmal1 KO (CBK) hearts. Proposed models for normal (Norm) and experimental (Exp.) conditions are depicted on the right. f, Overlap between commonly upregulated and h, downregulated genes in CBK/CM-RevDKO hearts (identified in e and g respectively) and cardiac REV-ERBα/E4BP4 cistromes. CBK data in (e,f,g,h) was obtained from35.
Extended Data Fig. 7 Deletion of Rev-erb genes in cardiomyocytes derepresses key metabolic regulators leading to mitochondrial abnormalities and loss of normal heart function.
a, Relative Pgc-1α/β, Naprt1 and Nampt mRNA levels in CM-RevDKO and control hearts (n = 3/genotype) from 2-month-old male mice. b, Relative Bmal1, Rev-erbα/β, and E4bp4 mRNA levels in CBK (n = 7 for control and n = 8 for KO), CM-RevDKO (n = 5 for control and n n = 6 for KO), E4bp4 (n = 8 for control and n = 10 for KO) and CBK/E4bp4 (double) KO (n = 6 for control and n = 9 for DKO) and control hearts from 2-month-old male mice for CM-RevDKO and control at ZT10 and from 3-month-old male mice for the rest at ZT12. c, Representative immunoblots and relative protein quantification for NAMPT in hearts from 3-month-old male mice with the following genetic background: CBK (n = 6/genotype), E4bp4 (n = 7/genotype), and CBK/E4bp4 (double) KO (n = 6/genotype), harvested at ZT12. n represents biologically independent replicates. All data are presented as mean ± SEM. Adj. P values in a were calculated by DESeq2, while ns, non significant; *P < 0.05; **P < 0.01; ***P < 0.001; ****P < 0.0001 by 2-sided Student’s t-test in b and one-way ANOVA followed by a Tukey’s multiple comparisons test in c (exact P values are provided in the Source Data).
Supplementary information
Supplementary Information
Supplementary Fig. 1
Supplementary Table 1
DEGs in CM-RevDKO versus control hearts. Isolated cardiac mRNA from 2-month-old male CM-RevDKO versus control mice (n = 3 per genotype) was subjected to RNA-seq. For differential gene expression analysis, FC, P and adjusted P (FDR) values were calculated with DESeq254. Supplementary Table 2. Output list of IMAGE analysis integrating H3K27ac and RNA-seq changes in CM-RevDKO samples.
Source data
Source Data Fig. 1
Statistical source data.
Source Data Fig. 2
Statistical source data.
Source Data Fig. 3
Statistical source data.
Source Data Fig. 4
Statistical source data.
Source Data Fig. 5
Statistical source data.
Source Data Extended Data Fig. 1
Statistical source data.
Source Data Extended Data Fig. 2
Statistical source data.
Source Data Extended Data Fig. 3
Statistical source data.
Source Data Extended Data Fig. 4
Statistical source data.
Source Data Extended Data Fig. 5
Statistical source data.
Source Data Extended Data Fig. 6
Statistical source data.
Source Data Extended Data Fig. 7
Statistical source data.
Rights and permissions
About this article
Cite this article
Dierickx, P., Zhu, K., Carpenter, B.J. et al. Circadian REV-ERBs repress E4bp4 to activate NAMPT-dependent NAD+ biosynthesis and sustain cardiac function. Nat Cardiovasc Res 1, 45–58 (2022). https://doi.org/10.1038/s44161-021-00001-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s44161-021-00001-9
This article is cited by
-
KDM8 epigenetically controls cardiac metabolism to prevent initiation of dilated cardiomyopathy
Nature Cardiovascular Research (2023)
-
Cardiomyocyte-specific disruption of the circadian BMAL1–REV-ERBα/β regulatory network impacts distinct miRNA species in the murine heart
Communications Biology (2023)
-
A new border for circadian rhythm gene NFIL3 in diverse fields of cancer
Clinical and Translational Oncology (2023)