Abstract
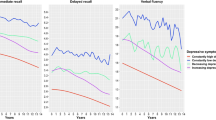
With the progressive aging of the world’s population, prolongation of a healthy lifespan in old age has become a medical research priority. The presence of depressive symptoms in later life is associated with poor health prognosis and increased mortality1,2. Here we explore distinct trajectories of depressive symptoms in later life and their association with several health-related outcomes in 19,110 older individuals followed for a median of 4.7 years. Using a latent class, mixed-modeling approach we identified four distinct trajectories of depressive symptoms with scoring patterns of consistently low, moderate, emerging and persistently high. Compared to those with minimal depressive symptoms, membership of any other class was associated with specific patterns of baseline sociodemographic and medical factors. Membership of any group with depressive symptoms was associated with a higher likelihood of health events, including physical disability, cancer and major bleeding episodes. Membership of the persistently depressed class was associated with increased mortality, while a diagnosis of dementia was generally limited to the class with initially low and progressively rising symptoms. The course of depressive symptoms in older individuals can vary widely and depend on several factors. The presence of depressive symptoms, including those that do not meet criteria for major depression, can flag a poor prognosis and risk for specific health conditions. Systematic assessment of depressive symptoms may facilitate early identification of at-risk populations.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The individual participant data that underlie the results reported in this article will be made available after deidentification. Requests for data access will be via the ASPREE Principal Investigators, with details for applications provided through the website, www.ASPREE.org, and in accordance with the NIH policy on data sharing: details available at https://grants.nih.gov/grants/policy/data_sharing/. Data availability will commence on publication of this article. The supporting Protocol and Statistical Analysis Plan is already available as an independently published article53. These data will be available upon request to investigators whose proposed use of the data, registered as a project through the ASPREE Access Management Site: https://ams.aspree.org/public/, has been approved by a review committee. These data will be available through a web-based data portal safe haven, based at Monash University, Australia.
Code availability
Codes are stored in the ASPREE web-based data portal safe haven, based at Monash University. They are available upon request following the procedures described above and on www.ASPREE.org.
References
Moussavi, S. et al. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet 370, 851–858 (2007).
Wei, J. et al. The association of late-life depression with all-cause and cardiovascular mortality among community-dwelling older adults: systematic review and meta-analysis. Br. J. Psychiatry 215, 449–455 (2019).
Alexopoulos, G. S. Mechanisms and treatment of late-life depression. Transl. Psychiatry 9, 188 (2019).
Gold, S. M., et al. Comorbid depression in medical diseases. Nat. Rev. Dis. Primers 6, 69 (2020).
Menear, M. et al. The influence of comorbid chronic physical conditions on depression recognition in primary care: a systematic review. J. Psychosom. Res. 78, 304–313 (2015).
Unützer, J. et al. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. J. Am. Med. Assoc. 288, 2836–2845 (2002).
Kuchibhatla, M. N., Fillenbaum, G. G., Hybels, C. F. & Blazer, D. G. Trajectory classes of depressive symptoms in a community sample of older adults. Acta Psychiatr. Scand. 125, 492–501 (2012).
Mirza, S. S. et al. 10-Year trajectories of depressive symptoms and risk of dementia: a population-based study. Lancet Psychiatry 3, 628–635 (2016).
Saeed Mirza, S. et al. 12 Year trajectories of depressive symptoms in community-dwelling older adults and the subsequent risk of death over 13 years. J. Gerontol. A Biol. Sci. Med. Sci. 73, 820–827 (2018).
Formánek, T. et al. Trajectories of depressive symptoms and associated patterns of cognitive decline. Sci. Rep. 10, 20888 (2020).
Sutin, A. R. et al. The trajectory of depressive symptoms across the adult life span. JAMA Psychiatry 70, 803–811 (2013).
Da Silva, S. A., Scazufca, M. & Menezes, P. R. Population impact of depression on functional disability in elderly: results from “São Paulo Ageing & Health Study” (SPAH). Eur. Arch. Psychiatry Clin. Neurosci. 263, 153–158 (2013).
Ly, M. et al. Late-life depression and increased risk of dementia: a longitudinal cohort study. Transl. Psychiatry 11, 147 (2021).
Wang, Y. H. et al. Depression and anxiety in relation to cancer incidence and mortality: a systematic review and meta-analysis of cohort studies. Mol. Psychiatry 25, 1487–1499 (2020).
Machado, M. O. et al. The association of depression and all-cause and cause-specific mortality: an umbrella review of systematic reviews and meta-analyses. BMC Med. 16, 112 (2018).
Ferrucci, L. & Fabbri, E. Inflammageing: chronic inflammation in ageing, cardiovascular disease, and frailty. Nat. Rev. Cardiol. 15, 505–522 (2018).
Mclaughlin, A. P. et al. The influence of comorbid depression and overweight status on peripheral inflammation and cortisol levels. Psychol. Med. 18, 1–8 (2021).
Furman, D. et al. Chronic inflammation in the etiology of disease across the life span. Nat. Med. 25, 1822–1832 (2019).
Diniz, B. S., Iii, C. F. R., Sibille, E., Bot, M. & Penninx, B. W. J. H. Major depression and enhanced molecular senescence abnormalities in young and middle-aged adults. Transl. Psychiatry 9, 198 (2019).
Martínez-Cengotitabengoa, M. et al. Peripheral inflammatory parameters in late-life depression: a systematic review. Int. J. Mol. Sci. 17, 2022 (2016).
Diniz, B. S. et al. Oxidative stress markers imbalance in late-life depression. J. Psychiatr. Res. 102, 29–33 (2018).
Mohebbi, M. et al. Prevalence of depressive symptoms and its associated factors among healthy community-dwelling older adults living in Australia and the United States. Int. J. Geriatr. Psychiatry 34, 1208–1216 (2019).
Ploubidis, G. B., Batty, G. D., Patalay, P., Bann, D. & Goodman, A. Association of early-life mental health with biomarkers in midlife and premature mortality: evidence from the 1958 British birth cohort. JAMA Psychiatry 78, 38–46 (2021).
Leone, M. et al. Association of youth depression with subsequent somatic diseases and premature death. JAMA Psychiatry 78, 302–310 (2021).
Demnitz, N. et al. Association of trajectories of depressive symptoms with vascular risk, cognitive function and adverse brain outcomes: the Whitehall II MRI sub-study. J. Psychiatr. Res. 131, 85–93 (2020).
Kaup, A. R. et al. Trajectories of depressive symptoms in older adults and risk of dementia. JAMA Psychiatry 73, 525–531 (2016).
Almeida, O. P., Hankey, G. J., Yeap, B. B., Golledge, J. & Flicker, L. Depression as a modifiable factor to decrease the risk of dementia. Transl. Psychiatry 7, e1117 (2017).
Quigley, E. M. M. Microbiota-brain-gut axis and neurodegenerative diseases. Curr. Neurol. Neurosci. Rep. 17, 94 (2017).
Berk, M. et al. Effects of aspirin on the long-term management of depression in older people: a double-blind randomised placebo-controlled trial. Mol. Psychiatry 26, 5161–5170 (2021).
Mulugeta, A., Zhou, A., King, C. & Hyppönen, E. Association between major depressive disorder and multiple disease outcomes: a phenome-wide Mendelian randomisation study in the UK Biobank. Mol. Psychiatry 25, 1469–1476 (2020).
Ohlsson, L. et al. Leaky gut biomarkers in depression and suicidal behavior. Acta Psychiatr. Scand. 139, 185–193 (2019).
Liśkiewicz, P. et al. Analysis of gut microbiota and intestinal integrity markers of inpatients with major depressive disorder. Prog. Neuropsychopharmacol. Biol. Psychiatry 106, 11076 (2021).
Snelson, M. et al. Processed foods drive intestinal barrier permeability and microvascular diseases. Sci. Adv. 7, eabe4841 (2021).
Burgueño, J. F. & Abreu, M. T. Epithelial Toll-like receptors and their role in gut homeostasis and disease. Nat. Rev. Gastroenterol. Hepatol. 17, 263–278 (2020).
McNeil, J. J. et al. Effect of aspirin on all-cause mortality in the healthy elderly. New Engl. J. Med. 379, 1519–1528 (2018).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J. R. Stat. Soc. Series B Methodol. 57, 289–300 (1995).
Group, A. I. Study design of ASPirin in Reducing Events in the Elderly (ASPREE): a randomized, controlled trial. Contemp. Clin. Trials 36, 555–564 (2013).
McNeil, J. J. et al. Baseline characteristics of participants in the ASPREE (ASPirin in Reducing Events in the Elderly) study. J. Gerontol. A Biol. Sci. Med. Sci. 72, 1586–1593 (2017).
Stocks, N. P. et al. Quality of life for 19,114 participants in the ASPREE (ASPirin in Reducing Events in the Elderly) study and their association with sociodemographic and modifiable lifestyle risk factors. Qual. Life Res. 28, 935–946 (2019).
Berk, M. et al. ASPREE-D: aspirin for the prevention of depression in the elderly. Int. Psychogeriatr. 28, 1741–1748 (2016).
Agustini, B. et al. Patterns of association between depressive symptoms and chronic medical morbidities in older adults. J. Am. Geriatr. Soc. 68, 1834–1841 (2020).
Gandek, B. et al. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. J. Clin. Epidemiol. 51, 1171–1178 (1998).
Chang, K.-F. & Weng, L.-J. Screening for depressive symptoms among older adults in Taiwan: cutoff of a short form of the Center for Epidemiologic Studies Depression Scale. Health (Irvine) 5, 588–594 (2013).
Mohebbi, M. et al. Psychometric properties of a short form of the Center for Epidemiologic Studies Depression (CES-D-10) scale for screening depressive symptoms in healthy community dwelling older adults. Gen. Hosp. Psychiatry 51, 118–125 (2018).
Irwin, M., Artin, K. H. & Oxman, M. N. Screening for depression in the older adult. Arch. Intern Med. 159, 1701–1704 (1999).
McNeil, J. J. et al. Effect of aspirin on cardiovascular events and bleeding in the healthy elderly. New Engl. J. Med. 379, 1509–1518 (2018).
McNeil, J. J. et al. Effect of aspirin on disability-free survival in the healthy elderly. New Engl. J. Med. 379, 1499–1508 (2018).
van Buuren, S. & Groothuis-Oudshoorn, K. mice: Multivariate imputation by chained equations in R. J. Stat. Softw. 45, 1–67 (2011).
Proust-Lima, C., Philipps, V. & Liquet, B. Estimation of extended mixed models using latent classes and latent processes: the R package lcmm. J. Stat. Softw. 78, 1–56 (2017).
Berlin, K. S., Williams, N. A. & Parra, G. R. An introduction to latent variable mixture modeling (Part 1): overview and cross-sectional latent class and latent profile analyses. J. Pediatr. Psychol. 39, 174–187 (2014).
Myung, I. J. Tutorial on maximum likelihood estimation. J. Math. Psychol. 47, 90–100 (2003).
Hubbard, A. E. et al. To GEE or not to GEE: comparing population average and mixed models for estimating the associations between neighborhood risk factors and health. Epidemiology 21, 467–474 (2010).
Wolfe, R. et al. The aspirin in reducing events in the elderly trial: statistical analysis plan. Int. J. Stroke 13, 335–338 (2018).
Acknowledgements
The ASPREE trial was supported by grants from the National Institute on Aging and the National Cancer Institute at the US National Institutes of Health (NIH, nos. U01AG029824 and U19AG062682); the National Health and Medical Research Council of Australia (NHMRC) (nos. 334047, 1081901 and 1127060); Monash University (Australia); and the Victorian Cancer Agency (Australia). M.B. is supported by a NHMRC Senior Principal Research Fellowship (no. 1156072), C.M.R. by a NHMRC Principal Research Fellowship (no. 1136372) and L.J.W. by a NHMRC Emerging Leadership Fellowship (no. 1174060). M.L. is funded by the Alfred Deakin Postdoctoral Research Fellowship. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript. We thank the ASPREE participants who volunteered for this study, the general practitioners and staff of the medical clinics who support the study participants and the trial staff and management team of the ASPREE study in Australia and the United States (www.aspree.org).
Author information
Authors and Affiliations
Contributions
Study design and grant application were performed by M.B., M.M., J.J.M., R.L.W., R.C.S., A.M.M., C.M.R., M.R.N., A.T., B.A. and M.L. Data were collected by M.B., R.L.W., M.R.N., R.C.S., C.M.R., A.M.M. and J.J.M. Statistical analysis was carried out by M.L., M.M. and B.A. Manuscript preparation and editing were the responsibility of B.A., M.L., M.B., C.M.R., R.L.W., M.R.N., R.C.S., A.M.M., J.J.M., M.L., M.M., J.R., L.J.W. and M.P.F.
Corresponding author
Ethics declarations
Competing interests
The authors declare the following potential competing interests. M.B. has received grant/research support from the NIH, Cooperative Research Centre, Simons Autism Foundation, Cancer Council of Victoria, Stanley Medical Research Foundation, Medical Benefits Fund, NHMRC, Medical Research Futures Fund, Beyond Blue, Rotary Health, A2 milk company, Meat and Livestock Board, Woolworths, Avant and the Harry Windsor Foundation; has been a speaker for AstraZeneca, Lundbeck, Merck and Pfizer; and served as a consultant to Allergan, AstraZeneca, Bioadvantex, Bionomics, Collaborative Medicinal Development, Lundbeck Merck, Pfizer and Servier—all unrelated to this work. M.R.N. is member of the Novartis lipids advisory board and received travel and advisory board support from Bayer AG, who provided product for the ASPREE study. A.T. has received honoraria for Safety Monitoring Committee or Advisory Board participation, or lectures from Amgen, Boehringer-Ingelheim, The Medicines Group, Novartis, Pfizer and Merck; and research support from Bayer for materials in ASPREE—all unrelated to this work. These funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Peer review
Peer review information
Nature Aging thanks Gindo Tampubolon, Mark Ward and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Tables
Supplementary Tables 1–5.
Rights and permissions
About this article
Cite this article
Agustini, B., Lotfaliany, M., Mohebbi, M. et al. Trajectories of depressive symptoms in older adults and associated health outcomes. Nat Aging 2, 295–302 (2022). https://doi.org/10.1038/s43587-022-00203-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s43587-022-00203-1
This article is cited by
-
Longitudinal Associations Between Multiple Types of Adverse Childhood Experiences and Depression Trajectories in Middle-Aged and Older Chinese Adults: a Growth Mixture Model
International Journal of Mental Health and Addiction (2023)