Abstract
Leukocyte telomere length (LTL) is a proposed marker of biological age. Here we report the measurement and initial characterization of LTL in 474,074 participants in UK Biobank. We confirm that older age and male sex associate with shorter LTL, with women on average ~7 years younger in ‘biological age’ than men. Compared to white Europeans, LTL is markedly longer in African and Chinese ancestries. Older paternal age at birth is associated with longer individual LTL. Higher white cell count is associated with shorter LTL, but proportions of white cell subtypes show weaker associations. Age, ethnicity, sex and white cell count explain ~5.5% of LTL variance. Using paired samples from 1,351 participants taken ~5 years apart, we estimate the within-individual variability in LTL and provide a correction factor for this. This resource provides opportunities to investigate determinants and biomedical consequences of variation in LTL.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Access to samples was made available through the UKB Resource under application no. 6077. As per the standard terms of UKB, all data for the telomere measurements were returned to UKB to be made available to other researchers. All source data used in this study, including all data related to the telomere measurements are accessible via application to UKB. Further information on registration to access the data can be found at http://www.ukbiobank.ac.uk/register-apply/. Information on telomere measurements can be viewed in the data showcase (https://biobank.ndph.ox.ac.uk/showcase/) under the following fields: 22190 (unadjusted), 22191 (adjusted), 22192 (adjusted and z-transformed) and 22194 (both time point measurements for the regression dilution bias experiment).
Code availability
LTL measurement data were added to a custom-built database application. The source code for this is available at https://github.com/LCBRU/telomere. No other custom code was used in this study.
References
Berry, J. D. et al. Lifetime risks of cardiovascular diseases. New Engl. J. Med. 366, 321–329 (2012).
Samani, N. J. & van der Harst, P. Biological ageing and cardiovascular disease. Heart 94, 537–539 (2008).
Blasco, M. A. Telomeres and human disease: ageing, cancer and beyond. Nat. Rev. Genet. 6, 611–622 (2005).
Harley, C. B. et al. Telomeres shorten during ageing of human fibroblasts. Nature 345, 458–460 (1990).
Allsopp, R. C. et al. Telomere length predicts replicative capacity of human fibroblasts. PNAS 89, 10114–10118 (1992).
Demanelis, K. et al. Determinants of telomere length across human tissues. Science 369, eaaz6876 (2020).
Broer, L. et al. Meta-analysis of telomere length in 19,713 subjects reveals high heritability, stronger maternal inheritance and a paternal age effect. Eur. J. Hum. Genet. 21, 1163–10 (2013).
Li, C. et al. Genome-wide association analysis in humans links nucleotide metabolism to leukocyte telomere length. Am. J. Hum. Genet. 106, 389–404 (2020).
Dorajoo, R. et al. Loci for human leukocyte telomere length in the Singaporean Chinese population and trans-ethnic genetic studies. Nat. Commun. 10, 2491 (2019).
Kimura, M. et al. Offspring’s leukocyte telomere length, paternal age, and telomere elongation in sperm. PLoS Genet. 4, e37 (2008).
De Meyer, T. et al. Paternal age at birth is an important determinant of offspring telomere length. Hum. Mol. Genet. 16, 3097–3102 (2007).
Hansen, M. E. B. et al. Shorter telomere length in Europeans than in Africans due to polygenetic adaptation. Hum. Mol. Genet. 25, 2324–2330 (2016).
Lynch, S. M. et al. Race, ethnicity, psychosocial factors, and telomere length in a multicenter setting. PLoS ONE 11, e0146723 (2016).
Needham, B. L. et al. Socioeconomic status, health behavior, and leukocyte telomere length in the National Health and Nutrition Examination Survey, 1999-2002. Soc. Sci. Med. 85, 1–8 (2013).
Richter, T. & von Zglinicki, T. A. Continuous correlation between oxidative stress and telomere shortening in fibroblasts. Exp. Gerontol. 42, 1039–1042 (2007).
Valdes, A. M. et al. Obesity, cigarette smoking, and telomere length in women. Lancet 366, 662–664 (2005).
Ornish, D. et al. Effect of comprehensive lifestyle changes on telomerase activity and telomere length in men with biopsy-proven low-risk prostate cancer: 5-year follow-up of a descriptive pilot study. Lancet Oncol. 14, 1112–1120 (2013).
Farzaneh-Far, R. et al. Association of marine omega-3 fatty acid levels with telomeric aging in patients with coronary heart disease. JAMA 303, 250–257 (2010).
Weischer, M., Bojesen, S. E. & Nordestgaard, B. G. Telomere shortening unrelated to smoking, body weight, physical activity, and alcohol intake: 4,576 general population individuals with repeat measurements 10 years apart. PLoS Genet. 10, e1004191 (2014).
Benetos, A. et al. Tracking and fixed ranking of leukocyte telomere length across the adult life course. Aging Cell 12, 615–621 (2013).
Armanios, M. & Blackburn, E. H. The telomere syndromes. Nat. Rev. Genet. 13, 693–704 (2012).
Zhu, X. et al. The association between telomere length and cancer risk in population studies. Sci. Rep. 6, 22243 (2016).
Brouilette, S. W. et al. Telomere length, risk of coronary heart disease, and statin treatment in the West of Scotland Primary Prevention Study: a nested case-control study. Lancet 369, 107–114 (2007).
Forero, D. A. et al. Meta-analysis of telomere length in Alzheimer’s disease. J. Gerontol. A Biol. Sci. Med. Sci. 71, 1069–1073 (2016).
Kuszel, L., Trzeciak, T., Richter, M. & Czarny-Ratajczak, M. Osteoarthritis and telomere shortening. J. Appl. Genet. 56, 169–176 (2015).
Rode, L., Bojesen, S. E., Weischer, M., Vestbo, J. & Nordestgaard, B. G. Short telomere length, lung function and chronic obstructive pulmonary disease in 46,396 individuals. Thorax 68, 429–435 (2013).
Rosner, B., Willett, W. & Spiegelman, D. Correction of logistic regression relative risk estimates and confidence intervals for systematic within‐person measurement error. Stat. Med. 8, 1051–1069 (1989).
Hutcheon, J. A., Chiolero, A. & Hanley, J. A. Random measurement error and regression dilution bias. Brit. Med. J. 340, c2289 (2010).
Sudlow, C. et al. UK Biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 12, e1001779 (2015).
Bycroft, C. et al. The UK Biobank resource with deep phenotyping and genomic data. Nature 562, 203–209 (2018).
Rode, L., Nordestgaard, B. G., Weischer, M. & Bojesen, S. E. Increased body mass index, elevated C-reactive protein, and short telomere length. J. Clin. Endocrinol. Metab. 99, E1671–E1675 (2014).
Wang, J. et al. Association between telomere length and diabetes mellitus: a meta-analysis. J. Int. Med. Res. 44, 1156–1173 (2016).
Valente, C. et al. Effect of physical activity and exercise on telomere length: systematic review with meta-analysis. J. Am. Geriatr. Soc. https://doi.org/10.1111/jgs.17334 (2021).
Strandberg, T. E. et al. Association between alcohol consumption in healthy midlife and telomere length in older men. The Helsinki Businessmen Study. Eur. J. Epidemiol. 27, 815–822 (2012).
Sharma, S., Malarcher, A. M., Giles, W. H. & Myers, G. Racial, ethnic and socioeconomic disparities in the clustering of cardiovascular disease risk factors. Ethn. Dis. 14, 43–48 (2004).
Codd, V. et al. Identification of seven loci affecting mean telomere length and their association with disease. Nat. Genet. 45, 422–427 (2013).
Bekaert, S. et al. Telomere length and cardiovascular risk factors in a middle‐aged population free of overt cardiovascular disease. Aging Cell 6, 639–647 (2007).
Dalgård, C. et al. Leukocyte telomere length dynamics in women and men: menopause vs age effects. Int. J. Epidemiol. 44, 1688–1695 (2015).
Ghimire, S., Hill, C. V., Sy, F. S. & Rodriguez, R. Decline in telomere length by age and effect modification by gender, allostatic load and comorbidities in National Health and Nutrition Examination Survey (1999–2002). PLoS ONE 14, e0221690 (2019).
Rehkopf, D. H. et al. Leukocyte telomere length in relation to 17 biomarkers of cardiovascular disease risk: a cross-sectional study of US adults. PLoS Med. 13, e1002188 (2016).
Neuner, B. et al. Telomere length is not related to established cardiovascular risk factors but does correlate with red and white blood cell counts in a German blood donor population. PLoS ONE 10, e0139308 (2015).
Mazidi, M., Penson, P. & Banach, M. Association between telomere length and complete blood count in US adults. Arch. Med. Sci. 13, 601–605 (2017).
Lin, Y. et al. Age-associated telomere attrition of lymphocytes in vivo is co-ordinated with changes in telomerase activity, composition of lymphocyte subsets and health conditions. Clin. Sci. 128, 367–377 (2015).
Fry, A. et al. Comparison of sociodemographic and health-related characteristics of UK Biobank participants with those of the general population. Am. J. Epidemiol. 186, 1026–1034 (2017).
Batty, D. G., Gale, C. R., Kivimäki, M., Deary, I. J. & Bell, S. Comparison of risk factor associations in UK Biobank against representative, general population based studies with conventional response rates: prospective cohort study and individual participant meta-analysis. Brit. Med. J. 368, m131 (2020).
Welsh, S., Peakman, T., Sheard, S. & Almond, R. Comparison of DNA quantification methodology used in the DNA extraction protocol for the UK Biobank cohort. BMC Genomics. 18, 26 (2017).
Cawthon, R. M. Telomere length measurement by a novel monochrome multiplex quantitative PCR method. Nucleic Acids Res. 37, e21(2009).
Acknowledgements
This research has been conducted using the UKB Resource under application no. 6077 and was funded by the UK Medical Research Council (MRC), Biotechnology and Biological Sciences Research Council and British Heart Foundation (BHF) through MRC grant MR/M012816/1 (V.C., C.P.N., J.R.T., J.N.D. and N.J.S.). The authors are also supported by grants from the BHF, SP/16/4/32697 (C.P.N.), RG/13/13/30194, RG/18/13/33946, CH/12/2/29428 (E.A., S.K., T.J., E.D.A., A.M.W., A.S.B. and J.N.D.); MRC, MR/L003120/1 (E.A., S.K., T.J., E.D.A., A.M.W., A.S.B. and J.N.D.); the National Institute for Health Research (NIHR) Leicester Cardiovascular Biomedical Research Centre (BRC-1215–20010, V.C., C.A.B., C.M., V.B., Q.W., S.E.H., C.P.N. and N.J.S.), NIHR Cambridge Biomedical Research Centre (BRC-1215-20014, E.A., S.K., T.J., E.D.A., A.M.W., A.S.B. and J.N.D.), NIHR Blood and Transplant Research Unit in Donor Health and Genomics (NIHR BTRU-2014-10024, E.A., S.K., T.J., E.D.A., A.M.W., A.S.B. and J.N.D.), Health Data Research UK (E.A., S.K., T.J., E.D.A., A.M.W., A.S.B. and J.N.D.) and EU/EFPIA Innovative Medicines Initiative Joint Undertaking BigData@Heart (11607, A.M.W. and E.A.). J.N.D. holds a BHF Personal Professorship. V.C., Q.W. and C.P.N. acknowledge support from the van Geest Heart and Cardiovascular Diseases Research Fund, University of Leicester. P. Akbari, T. Bolton and M. Arnold made computational and biostatistical contributions to this work. We thank L. Courtney, S. Welsh and D. Fry for assistance with UKB samples.
Author information
Authors and Affiliations
Contributions
M.D., C.S., M.P., S. Sheth, D.E.N. and V.C. generated the data. S.C.W., C.A.B., R.B., J.R.T., V.C. and C.P.N. curated the data. C.M., V.B., Q.W., A.S.B., J.R.T., V.C. and C.P.N. performed statistical analyses. V.C., C.P.N., C.M., Q.W., C.A.B., E.A., S.K., S. Stoma, V.B., T.J., E.D.A., A.M.W., A.S.B., J.R.T., J.N.D. and N.J.S. drafted the manuscript and all authors revised it. V.C., C.P.N., J.R.T., J.N.D. and N.J.S. (Principal Investigator) secured funding and oversaw the project.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Aging thanks Timothy Hohman, Immaculata De Vivo, Sara Hagg and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Significant technical parameters affecting LTL measurements based on the stage 1 adjustment.
Summary box plots are shown for the 474, 074 LTL measurements for each associated parameter: Enzyme batch (A), PCR machine (B), primer batch (C), operator (D). Individual data points show minimum and maximum measures, the box represents the lower quartile (bottom), upper quartile (top) and median (internal line). The upper and lower whiskers extend to a value no further than 1.5 * IQR from the respective quartile. Linear relationships were seen between LTL and temperature (E) and humidity (F). For both (E) and (F) a fitted regression line is shown with 95% confidence intervals (gray shading).
Extended Data Fig. 2 Significant interactions based on the stage 2 adjustment.
(A) LTL by Primer and Operator. (B) LTL by primer and PCR machine. PCR machines 5 and 6 were not used at the start of the pilot study (primer batch 1) and machines 7 and 8 were used from the end of the pilot stage (primer batch 3 onwards).
Extended Data Fig. 3 Effect of A260/280 on LTL.
The distribution of DNA sample A260/280 ratios is illustrated in (A). We observed an increase in LTL with very low and very high A260/280 ratios (B). Data shown is mean LTL (blue0 with 95% confidence interval (gray).
Extended Data Fig. 4 Distribution of the coefficients of variation for the repeat samples.
Distribution of CVs after technical adjustment for both the blinded repeats (A) (n=528) and deliberate repeats (B) (n=22,615) are shown. The gray dotted line represents the median coefficient of variation with the shaded region representing the interquartile range.
Extended Data Fig. 5 Data on the first and second DNA sample used to estimate regression dilution ratio.
(A) Histogram showing that the gap between the two sample collections has a mean interval of 5.5 years (range: 2–10 years, N=1,312). (B) Correlation between the first and second loge-LTL measure by time, estimated by the difference in years between the two sample collections and shown with 95% confidence intervals. The blue circle reflects the correlation estimate (center) with size reflecting the number of participants measured each year (exact N shown in brackets). The black line shows the overall pooled correlation for all samples and the red dotted lines indicate the 95% confidence interval for this estimate.
Extended Data Fig. 6 Age and sex relationships for participants used to estimate regression dilution bias.
The decline of LTL with age is shown for men (blue) and women (plum) for both the first (A) and second (B) LTL measurements. The estimated effect sizes are shown for age (β_Age) and sex (β_Sex) within the figures.
Extended Data Fi. 7 Decline of LTL with age.
The decline of z-standardized loge-LTL with age is shown for men (blue) and women (plum) in adjusted data. The y-axis is truncated at -5SD to +5 SD with 166 data points (80 women, 86 men) not shown. A small number of participants recruited by UK Biobank fall outside of the stated 40–69 age range.
Extended Data Fig. 8 Decline in LTL with age by sex.
Using stratified regression for men (blue) and women (plum) for all participants (N=474,074) we considered the non-linear effect of age within each sex. Here we show the predicted shape in a solid line and the observed data in a dashed line with 95% confidence intervals. There is significant non-linearity observed for women, where the rate of LTL decline increases as the population ages.
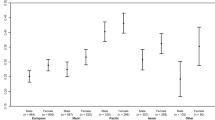
Extended Data Fig. 9 Telomere lengths within individual ethnic groups.
Data adjusted for both age and sex are shown in purple for individual observations to indicate the range and quantity of data alongside a box-plot to show the median (line) and interquartile range (box) with whiskers extending to a value no further than 1.5 * IQR from the respective quartile. Box plots of data with additional adjustment for BMI, CRP, HbA1c, smoking status, alcohol consumption and measures of physical activity, socioeconomic status and diet are shown in blue. Ethnicity is self-reported and presented as defined by UK Biobank Data-Field 21000. Note that we shorten “Asian or Asian British” to Asian and “Black or Black British” to Black.
Extended Data Fig. 10 LTL by age in different ethnic groups.
LTL measurements were adjusted for sex, BMI, CRP, HbA1c, smoking status, alcohol consumption and measures of physical activity, socioeconomic status and diet.
Supplementary information
Rights and permissions
About this article
Cite this article
Codd, V., Denniff, M., Swinfield, C. et al. Measurement and initial characterization of leukocyte telomere length in 474,074 participants in UK Biobank. Nat Aging 2, 170–179 (2022). https://doi.org/10.1038/s43587-021-00166-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s43587-021-00166-9
This article is cited by
-
Insight into telomere regulation: road to discovery and intervention in plasma drug-protein targets
BMC Genomics (2024)
-
Association between modifiable lifestyle factors and telomere length: a univariable and multivariable Mendelian randomization study
Journal of Translational Medicine (2024)
-
Causal association of obesity with epigenetic aging and telomere length: a bidirectional mendelian randomization study
Lipids in Health and Disease (2024)
-
Smoking and diabetes cause telomere shortening among alcohol use disorder patients
Scientific Reports (2024)
-
Causal relationship between telomere length and sepsis: a bidirectional Mendelian randomization study
Scientific Reports (2024)