Abstract
The coronavirus disease 2019 (COVID-19) pandemic presents an unprecedented challenge to public health, with over 233 million confirmed cases and over 4.6 million deaths globally as of September 20211. Although many studies have reported worse mental health outcomes during the early weeks of the pandemic, some sources suggest a gradual decrease in anxiety and depressive symptoms during the lockdown2. It remains to be explained whether mental health continued to deteriorate during the initial lockdown or whether there were signs of stabilization or improvement in the mental health of community-dwelling middle-aged and older adults. Our results showed that adults had twice the odds of depressive symptoms during the pandemic compared with the prepandemic period, with subgroups characterized by lower socioeconomic status and poor health-related factors experiencing a greater impact. Over 43% of adults showed a pattern of moderate or clinically high levels of depressive symptoms at baseline that increased over time. Loneliness and COVID-19 stressors were predictors of worsening depressive symptom trajectories. The disparities and patterns in the depressive symptom trajectories suggest that the negative mental health impacts of the pandemic persist and may worsen over time. Interventions that address the pandemic stressors and alleviate their impact on the mental health of adults are needed.
Similar content being viewed by others
Main
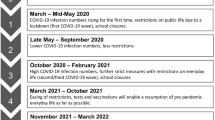
The rapid spread of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus across the globe resulted in many national and local governments implementing drastic health measures, including isolation, quarantine, lockdowns, physical distancing, closure of nonessential services and travel restrictions, to contain the spread of the virus3. The first complete lockdown began in most Canadian provinces in mid-March 2020 and continued until June 2020, with large numbers of people across the country urged to stay at home for substantial periods of time. The direct risks of the virus, uncertainty about disease status and the socioeconomic consequences of the enacted public health measures can have a substantial, long-lasting impact on individuals’ mental health and well-being, especially for older adults who are disproportionately affected by COVID-19, and the pandemic mitigation measures4.
Studies comparing mental health outcomes before the pandemic with results obtained during the early weeks of the pandemic have shown an increase in clinically significant levels of psychological distress5,6. Evidence from previous outbreaks, including the severe acute respiratory syndrome (SARS) and Ebola outbreaks, and the current COVID-19 pandemic indicates that many individuals have experienced a wide range of adversities, including challenges with meeting basic needs, increased caregiving responsibilities, difficulties with accessing non-COVID-19-related healthcare, employment and financial loss, and disruption of social networks, which may increase the risk of mental illness during and after the outbreaks7,8,9. Further, the impact of the COVID-19 pandemic on the older population has occurred against the backdrop of existing physical and mental health morbidities, social isolation, loneliness and reliance of aging individuals on both family and formal caregivers—factors that are themselves associated with increased risk, severity and progression of mental illness10. These findings highlight the importance of identifying subgroups of individuals who are most at risk of poor mental health and examining how their mental health is changing as the pandemic continues.
Most studies examining the mental health impact of the COVID-19 pandemic have been conducted in younger samples, have included specific target populations and have been cross-sectional in design. Some longitudinal studies have focused on average change in depressive symptoms for the entire sample or lacked depression measures before the pandemic, which makes it challenging to examine changes in mental health and can obscure different patterns of change in mental health over time. Although many studies have reported worse mental health outcomes during the early weeks of the pandemic, some sources suggest a gradual decrease in anxiety and depressive symptoms during lockdown2. Some evidence also suggests that older individuals did not experience poorer psychological well-being than comparatively younger individuals11. However, social participation and loneliness were identified as important risk factors for psychological well-being, and it is these factors that have been impacted during the pandemic, especially for older adults. Therefore, it remains to be explained whether mental health continued to deteriorate during the initial lockdown (March–December 2020) or whether there were signs of stabilization or improvement in the mental health of community-dwelling middle-aged and older adults. Further, it remains to be clarified whether the risk factors had a differential effect on the psychological well-being of older adults compared with middle-aged adults or whether the impact was consistent across the adult lifespan. The purpose of this study was to examine the relationship of social determinants and health-related factors with changes in the prevalence of depressive symptoms during the initial lockdown and after reopening following the first wave in Canada and to evaluate the impact of loneliness and pandemic-related stressors on the severity and trajectory of depressive symptoms in middle-aged and older adults.
Results
Descriptive statistics
Cross-sectional descriptive characteristics of participants in the Canadian Longitudinal Study on Aging (CLSA) baseline (n = 51,338), first follow-up (n = 44,817), and COVID-19 baseline (n = 28,559) and exit (n = 24,114) surveys are provided in Supplementary Table 1. Of the total participants recruited at CLSA baseline, 50.95% were female, 41.87% were aged 65 years and older, and 68.52% had an annual household income of CDN $50,000 or more. Of the 28,559 participants recruited into the COVID-19 baseline survey, 0.34% were confirmed cases, 0.23% were probable cases and 9.34% were suspected cases of COVID-19. At the COVID-19 baseline survey, 21.15% of participants reported health-related concerns, 51.58% had difficulties in accessing resources, 7.17% experienced verbal or physical conflict, 20.91% reported caregiving challenges and 71.40% reported separation from family. The prevalence of depressive symptoms increased from 16.38% at CLSA baseline to 21.14% during the initial lockdown of the pandemic and was 21.96% at the time of administering the COVID-19 exit survey when there was a gradual lifting of the public health restrictions. The distributions of the prevalence of depressive symptoms by social determinants and health-related factors before and during the pandemic are presented in Table 1.
Sociodemographic factors and change in depressive symptoms
Results from weighted generalized estimating equation (WGEE) models examining the change in prevalence of depressive symptoms over time after adjusting for covariates are presented in Table 2. Overall, participants had approximately two times higher odds of depressive symptoms during the initial wave of the COVID-19 pandemic compared with the pre-COVID-19 period. There was also evidence of differential effects by social determinants and health-related factors when examining effect modification with time period, demonstrating that some subgroups were more vulnerable to poor mental health. Our results showed an inverse association between annual income and depressive symptoms over time, where the lower the income, the greater the increase in the odds of depressive symptoms during the pandemic when compared with the highest income group before the pandemic. The odds of depressive symptoms during the initial lockdown increased by 3.35 times (95% confidence interval (CI): 2.81, 3.99) for individuals who had an annual household income of less than CDN $20,000 and by 3.03 times (95% CI: 2.71, 3.38) for those with income of CDN $20,000 or greater and less than CDN $50,000, relative to those with an income of CDN $150,000 or more in the pre-COVID-19 period.
Health-related risk factors including loneliness, pre-existing chronic conditions and low social participation were significant determinants of increase in the prevalence of depressive symptoms during the pandemic. The odds of depressive symptoms during the initial lockdown increased 6.75 times (95% CI: 6.34, 7.18) for individuals who reported feelings of loneliness compared with those who did not report loneliness before the pandemic and 2.36 times (95% CI: 2.18, 2.56) for individuals with lower social participation before the pandemic compared with those with higher social participation before the pandemic. Further, the odds of depressive symptoms during the initial lockdown increased for individuals living with a greater number of chronic conditions (three or more chronic conditions: odds ratio (OR): 3.92, 95% CI: 3.58, 4.30; two chronic conditions: OR: 3.18, 95% CI: 2.89, 3.51; one chronic condition: OR: 2.56, 95% CI: 2.34, 2.81) compared with those with no chronic conditions before the pandemic. Overall, the odds of depressive symptoms remained elevated for all subgroups at the COVID-19 exit survey when compared with reference groups before the pandemic. Our results also showed evidence of differential effects by sex, living arrangements and health behaviors when interactions were examined with time period (Supplementary Table 2). We explored interactions of age with risk factors, including number of chronic conditions and loneliness, and found the results to be consistent with the trends reported for the main effects and time period by risk factor interactions (Supplementary Table 3). As part of a sensitivity analysis, we also examined the association stratified by age groups and found the results to be in agreement with those reported for the entire sample (Supplementary Table 4).
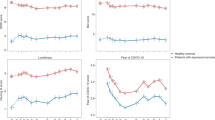
COVID-19 stressors and depressive symptom trajectories
The group-based trajectory model identified three distinct trajectory groups: one with a linear term and the other two with a quadratic term. The three depressive symptom trajectories were labeled as ‘high-increasing’, ‘moderate-increasing’ and ‘low-consistent’. As depicted in Fig. 1, 8.0% of participants showed high-increasing, 35.5% showed moderate-increasing and 56.6% showed low-consistent patterns of depressive symptoms over time. The linear change estimate was statistically significant for the low-consistent trajectory, while both linear and quadratic changes were statistically significant for the high-increasing and moderate-increasing trajectories.
Results from multivariable analysis evaluating the impact of loneliness and COVID-19 stressors on the severity and trajectory of depressive symptoms are presented in Table 3. The odds of a high-increasing trajectory were greater than for a low-consistent trajectory for adults who had experienced verbal or physical conflict (OR: 8.34; 95% CI: 6.65, 10.45), reported loss of income or were unable to access resources (OR: 2.81; 95% CI: 2.43, 3.25), had health-related concerns (OR: 2.47; 95% CI: 2.12, 2.88), were unable to provide care or spent more time in caregiving responsibilities (OR: 1.86; 95% CI: 1.58, 2.18) and were separated from family (OR: 1.49; 95% CI: 1.28, 1.73) during the pandemic. Further, loneliness was associated with membership in the high-increasing and moderate-increasing trajectory groups. Participants who reported being lonely were 15.50 times (95% CI: 13.17, 18.25) more likely to be in the high-increasing trajectory group and 5.41 times (95% CI: 4.94, 5.93) more likely to be in the moderate-increasing trajectory group compared with the low-consistent group. Social determinants and health-related factors were also significantly associated with the severity of depressive symptom trajectories (Table 3). Using latent class growth modeling (LCGM), we also explored the impact of the COVID-19 pandemic stressors and loneliness on depression subcomponents, including depressed affect, somatic symptoms and positive affect, and found the results to be largely consistent with those observed for the overall depressive symptom score (Supplementary Table 5 and Supplementary Figs. 1–3).
Discussion
Using longitudinal data from a large, nationally generalizable sample of community-dwelling middle-aged and older adults, this study examined the association of social determinants and health-related factors with changes in the prevalence of depressive symptoms during the initial lockdown and after reopening following the first wave of COVID-19 in Canada and evaluated the impact of loneliness and pandemic-related stressors on the severity and trajectory of depressive symptoms. Our results showed that adults had twice the odds of depressive symptoms during the pandemic compared with the prepandemic period, with subgroups characterized by lower socioeconomic status and poorer health-related factors experiencing a greater impact across the age groups. More than four in ten adults showed a pattern of moderate or high levels of depressive symptoms at baseline that increased over time. Loneliness and COVID-19 stressors were significant predictors of worsening depressive symptom trajectories.
Social determinants were found to be the key drivers of mental health effects during the pandemic. In comparison with the low-consistent depressive symptom trajectory group, subgroups of adults with higher and increasing depressive symptoms were more likely to have lower income or report loss of income and difficulties in accessing resources including supplies or food, usual healthcare, prescription medications and treatments during the pandemic. These findings are consistent with previous research reporting unemployment, job insecurity, financial instability and food insecurity to be associated with stress, anxiety and depression12,13,14,15. Further, many individuals have been unable to access a range of healthcare services during the pandemic, including regular medical services and diagnostic procedures, elective surgical procedures and counseling services16,17. The inability to access healthcare services, especially for those living with pre-existing mental health conditions, frailty or multimorbidity, may lead to new or worsening depressive symptoms over time. In fact, our results showed that participants who reported health-related concerns during the pandemic and participants who had a greater number of pre-existing health conditions were more likely to have membership in the moderate or high and increasing depressive symptom trajectory groups compared with the low-consistent trajectory group.
Caregiving responsibilities, separation from family and loneliness were associated with a greater likelihood of membership in the moderate or high and increasing trajectory groups compared with the low-consistent group. Evidence indicates that caregivers have worse mental health and are more likely to report fatigue, sleep disturbance and anxiety than noncaregivers18,19. Caregiving responsibilities increased or intensified as informal caregivers may feel obligated to help care recipients with activities of daily living and manage health complications resulting from exposure to COVID-19 or due to disruptions in regular care access during the pandemic18. The pandemic made it physically, emotionally and economically more difficult for caregivers to provide care, thereby making them particularly more vulnerable to poor mental health19. Separation from family members due to the restrictions around social gatherings is also an important risk factor for poor mental health as it may limit access to informal caregivers and weaken social networks, resulting in increased social isolation and feelings of loneliness. There is evidence that loneliness and separation from family during the pandemic were associated with a higher risk of mood disorders and exacerbated pre-existing mental illness20,21. A greater proportion of females reported separation from family, increased time caregiving and inability to care for people who required assistance due to a health condition or limitation, which may partly explain the higher odds of depressive symptoms during the pandemic in females compared with males.
Adults who experienced verbal or physical conflict during the pandemic were more likely to show patterns of moderate or clinically high and increasing depressive symptoms. Studies have broadly demonstrated an increase in family conflict and interpersonal violence in the aftermath of natural disasters22,23. In the context of the COVID-19 pandemic, individual or simultaneous presence of risk factors such as unemployment, economic loss, lack of access to basic needs, lockdowns and social isolation, reduced healthcare service availability and the inability of individuals to temporarily escape abusive family members may increase the risk of, or exacerbate, emotional and physical family or partner conflict and may, in turn, increase the risk of worsening existing mental health problems24,25.
Together, our results suggest several targets for prevention and intervention. Responding to COVID-19 pandemic-related stressors and challenges requires a multifaceted approach that includes strategies that avoid disruption to healthcare access while following physical distancing guidelines (for example, telemedicine), enhance unemployment insurance, promote supportive workplace environments and policies, ensure adequate access to basic needs and resources, enable access to online and telephone support services and increase opportunities for safe social participation. Because disparities in mental health outcomes have persisted, interventions to mitigate the negative impact of the COVID-19 pandemic and lockdown on mental health should be targeted at those who are most at risk, including individuals with low socioeconomic status, those who are lonely and those living with multimorbidity. Our findings also indicate the need to identify and address concerns early to avoid worsening of depressive symptom trajectories.
The present study has several strengths, including the timing of data collection relative to the lockdown restrictions implemented in Canada and use of a large population-based sample to longitudinally examine social determinants, health-related factors and COVID-19 pandemic stressors associated with changes in the prevalence of depressive symptoms in middle-aged and older adults. However, it is important to note that our study sample did not include individuals residing in long-term care institutions, which may have led to underestimates of the prevalence of depressive symptoms and limits the generalizability of our findings to community-dwelling populations only. Further, a greater proportion of the participants who did not take part in the COVID-19 study were older, had lower annual income and had depressive symptoms (Supplementary Table 6), which may have impacted the validity of our findings. Differences in the method of administration of the ten-item Center for Epidemiologic Studies Short Depression Scale (CES-D10) questionnaire may also have impacted the results, as some participants completed the questionnaire in person whereas other participants completed the questionnaire over the telephone or online. However, the CES-D10 scale has been shown to perform well and had high internal consistency (range, 0.86–0.88) in a sample of adults who completed the survey in person, over the telephone and online26. Measurement invariance of the CES-D10 has also been examined in the CLSA, and the results support the use of this scale in a heterogenous CLSA sample27. Also, information on social connectivity and network size during the pandemic was not available and therefore not examined in the analysis. We examined age as a time-varying covariate; however, other variables such as physical activity, social participation and alcohol consumption were not included as time-varying covariates in the analysis. Finally, the prevalence of depressive symptoms may have differed based on when, and during what phase, data collection was conducted during the pandemic.
Overall, the results of this study indicate that the COVID-19 pandemic has had a substantial negative impact on the mental health of middle-aged and older adults. Social determinants, loneliness and COVID-19 stressors were important predictors of increase in depressive symptoms during the pandemic. The disparities and patterns in the depressive symptom trajectories observed during the initial stages of the pandemic indicate that the negative mental health impacts of the pandemic persist and may worsen over the long term in the absence of effective interventions. Therefore, identifying and implementing intervention strategies, support and related public health measures for adults at higher risk of poor mental health trajectories may help alleviate the impact of the pandemic.
Methods
Data source and study participants
The study was approved by the Hamilton Integrated Research Ethics Board and by the research ethics boards of all the participating institutions across Canada. Written informed consent was obtained from the participants. Participants had the study and data collection procedures explained to them and had the opportunity to seek clarification before consenting. Participants provided separate consent for questionnaire and physical data collection, for biological sample collection and for linking their provincial health information to information collected by the CLSA. There was no direct compensation for the participants. The CLSA is a large, national, longitudinal cohort study that recruited 51,338 Canadian residents (25,183 males and 26,155 females) aged 45–85 years at baseline (2012–2015) to be followed every 3 years, for at least 20 years or until death or loss to follow-up, to collect information on the changing biological, medical, psychological, social, lifestyle and economic aspects of people’s lives. Participants were recruited from across the ten provinces through Statistics Canada’s Canadian Community Health Survey, provincial healthcare registration databases and random digit dialing. Individuals residing in Canada’s three territories, on First Nations reserves, in long-term care facilities, members of the armed forces, those who were unable to communicate in English or French and those with severe cognitive deficits were not eligible to participate in the study. At each study visit, all participants provided data by questionnaires, but a subset of 30,097 participants living within 25–50 km of 1 of 11 Data Collection Sites (DCS) across seven Canadian provinces were also interviewed in their home and visited a DCS to provide a range of physical assessments and biological samples. The first follow-up was completed on 48,893 participants (95% retention) in mid-2018, and the second follow-up is nearing completion (2018–2021). The CLSA design and methods have been described in detail elsewhere28.
The CLSA participants were invited to participate in the CLSA COVID-19 Questionnaire Study, which was launched on 15 April 2020 with the aim of understanding the epidemiology of COVID-19, including its impact on the mental health outcomes of middle-aged and older adults. Of the 51,388 CLSA participants, 8,638 were excluded because of death (n = 2,500), loss to follow-up (n = 3,406), requiring a proxy to participate (n = 318) or for other reasons such as unavailability of their contact information (n = 2,414). The remaining 42,700 participants were invited to participate by email to complete the web-based questionnaire (n = 34,498) or by telephone to complete the telephone interview with a trained CLSA interviewer (n = 8,202). During the recruitment process, another 189 participants were identified as deceased or requiring a proxy and therefore excluded. Of the 42,511 participants who were eligible to take part in the COVID-19 study, 28,559 (67.2%) agreed to participate. Over the 9-month period, participants completed a 30-min questionnaire at baseline (15 April–30 May 2020), 10-min questionnaires weekly (four times by web) or biweekly (two times by phone), three monthly questionnaires and a final 30-min exit questionnaire (29 September–30 December 2020).
Measurement of study variables
Depressive symptoms
Screening for depressive symptoms in the CLSA was done using the CES-D10, which assesses depressive symptoms in the past week29. It includes three items on depressed affect, five items on somatic symptoms and two items on positive affect. Each item is scored from zero to three: rarely or never (<1 day), some of the time (1–2 days), occasionally (3–4 days) and all of the time (5–7 days). Scores for each participant were summed after reversing the positive affect items and can range between 0 and 30 with higher scores indicating a greater number of depressive symptoms. A positive screen for depressive symptoms was based on a score of ten or higher29. The CES-D10 has been shown to be reliable and valid in assessing depressive symptoms in adults, with internal consistency of 0.86, test–retest reliability of 0.85, convergent validity of 0.91 and divergence of 0.89 (refs. 30,31).
COVID-19 experiences
The COVID-19 pandemic experiences and stressors were measured using a self-reported questionnaire administered at the COVID-19 baseline survey. Health-related stressors were identified by asking participants to indicate whether they were ill or if someone close to them was ill or had died due to COVID-19 or non-COVID-19-related reasons. Difficulties with accessing resources was identified by asking participants to indicate whether they had experienced loss of income, and difficulties in accessing necessary supplies, food and usual healthcare including prescription medications and treatments. Conflict was identified by asking participants to report whether they had experienced increased verbal or physical conflict. Separation from family was identified by asking participants to report whether they were separated from family during the pandemic. Caregiving experience assessed whether participants had spent increased time in caregiving or whether they were unable to care for people who required assistance due to a health condition or limitation. The pandemic experiences were grouped as ‘yes’ if the participant indicated at least one experience in the specific category or ‘no’ if the participant did not indicate any of the experiences in the specific category.
Covariates
The data from the CLSA baseline and first follow-up surveys were considered as being in the ‘pre-COVID-19’ period, and the time period variable for both these time points was coded as a zero and considered as the reference group in WGEE models. The time period was categorized as ‘pre-COVID-19’, ‘COVID-19 baseline’ and ‘COVID-19 exit’. The WGEE model was adjusted for age (<55, 55–64, 65–74 and ≥75 years), sex, ethnicity (white or nonwhite), total annual household income (CDN <$20,000, $20,000 to <$50,000, $50,000 to <$100,000, $100,000 to <$150,000 and ≥$150,000), dwelling type (house; apartment/condominium; or other type of dwelling including senior’s housing, mobile home and hotel), living area (urban, rural), household composition (living alone, not living alone), loneliness (see definition below), alcohol consumption (never, occasional, binge or regular drinker), smoking status (never, former or current smoker), physical activity (see definition below), social participation (see definition below) and number of chronic conditions (see definition below). Loneliness was assessed using the Revised UCLA Loneliness Scale (R-UCLA)32. Participants were asked to indicate how often they felt left out, felt isolated from others and lacked companionship. Response options included ‘hardly ever’, ‘some of the time’ and ‘often’. The total score may range from three to nine, and participants with a score of greater than three were classified as lonely32. Physical activity was assessed using the Physical Activity Scale for the Elderly (PASE) and dichotomized as meeting the World Health Organization’s age-specific guidelines for physical activity of at least 150 min of moderate-intensity or at least 75 min of vigorous-intensity physical activity per week33,34. Social participation was assessed by summing the frequency of involvement in eight categories to represent the number of community activities undertaken in a month. The social activities included family or friendship activities outside the household; church or religious activities; sports/physical activities with other people; educational or cultural activities involving other people; service club or fraternal organization activities; neighborhood, community or professional association activities; volunteer or charity work and other recreational activities involving other people35. The total score for social participation was categorized based on age- and sex-specific quintile into ‘low’ and ‘high’ social participation. The number of chronic conditions from ten disease categories including musculoskeletal, respiratory, cardiovascular, endocrine-metabolic, neurological, gastrointestinal, genitourinary, ophthalmologic, renal and cancer was summed up and categorized into ‘none’, ‘one’, ‘two’ and ‘three or more’ chronic conditions.
Statistical analysis
Descriptive statistics were reported at each time point. CLSA first follow-up data were used to impute a whole variable that was not assessed in the COVID-19 baseline and exit surveys, and COVID-19 baseline data were used to impute a variable that was not assessed in the COVID-19 exit survey. The WGEE was used to examine the change in prevalence of depressive symptoms over time. The WGEE can model longitudinal or clustered data and binary outcomes and can handle monotonic missing data appropriately when the data are missing at random36. We performed WGEE on 37,111 individuals, which includes those with a monotonic pattern of missing data for the depressive symptom variable. Interaction terms between time period and sociodemographic and health factors were assessed to determine how the change in depressive symptom prevalence over time depended on these factors. For each risk factor by time period interaction, ORs were reported for at-risk groups during the COVID-19 baseline and exit time points in comparison with the group that was least at risk before the pandemic. The WGEE models were adjusted for all the covariates listed above. Age was included as a time-varying covariate, loneliness was assessed at CLSA first follow-up and all other covariates were assessed at CLSA baseline.
LCGM, a semiparametric, group-based modeling strategy, was used to identify distinct classes of individuals who follow a similar pattern of depressive symptoms over the four time points and to examine the impact of loneliness and COVID-19 experiences on the depressive symptoms trajectories37. The censored normal distribution was specified as the depressive symptoms score was modeled as a continuous variable to more accurately model data where floor and ceiling effects may be possible. Model selection involved testing different numbers and shapes of trajectory groups using statistical considerations and model parsimony. The best fitting model was identified by comparing the Akaike’s information criterion (AIC) and Bayesian information criterion (BIC) values, with smaller values indicating a good fitting model. Quadratic and cubic terms that were not statistically significant were excluded from the model. Trajectories were modeled using the PROC TRAJ procedures in SAS37. Missing longitudinal data were handled in the PROC TRAJ procedure under the missing-at-random assumption, which permits patterns with missing data to borrow parameter information from patterns with more or complete data points through the latent variable38. In addition to the covariates listed above, the LCGM was adjusted for self-reported COVID-19 status based on the criteria adapted from the Public Health Agency of Canada and Centers for Disease Control and Prevention that were available during the initial wave of the pandemic39,40. Confirmed cases of COVID-19 included participants who reported testing positive for SARS-CoV-2 by nucleic acid amplification test. Probable cases of COVID-19 included (1) participants who had a laboratory test with fever (over 38 °C) or new onset or exacerbation of cough or who met the COVID-19 exposure criteria and were tested for COVID-19, but the results were inconclusive; or (2) participants who did not have a laboratory test but reported fever (over 38 °C) or a new onset or exacerbation of cough and had close contact with a confirmed COVID-19 case or lived or worked in a closed facility known to be experiencing an outbreak of COVID-19; (3) participants who were told by a healthcare provider that they had COVID-19 but did not have a confirmatory test. Suspected cases of COVID-19 included participants who reported two or more symptoms including fever, cough (dry or wet), runny nose, sore/scratchy throat, headache, chills or shivering, muscle and/or joint aches/pains, loss of smell or difficulty breathing and met the exposure criteria or had a close contact with a probable case of COVID-19. OR and 95% CI values were reported, statistical significance was set at 0.05 for a two-tailed test and statistical analysis was conducted using SAS software v.9.4. CLSA has developed a core suite of software based on open-source code to collect data. The specific software used to collect data include ONYX (v.1.12.0), Limesurvey (v.3.7.1 with customizations) and PINE (v.2.7).
Reporting Summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
Data are available from the Canadian Longitudinal Study on Aging (www.clsa-elcv.ca) for researchers who meet the criteria for access to de-identified CLSA data.
Code availability
Custom code that supports the results of this study can be made available upon request from the corresponding author.
References
World Health Organization. WHO coronavirus (COVID-19) dashboard. https://covid19.who.int (2021).
Fancourt, D., Steptoe, A. & Bu, F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiatry 8, 141–149 (2021).
Government of Canada. Individual and community-based measures to mitigate the spread of COVID-19 in Canada. https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/health-professionals/public-health-measures-mitigate-covid-19.html (2021).
Mueller, A. L., McNamara, M. S. & Sinclair, D. A. Why does COVID-19 disproportionately affect older people? Aging 12, 9959–9981 (2020).
Pierce, M. et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry 7, 883–892 (2020).
Shanahan, L. et al. Emotional distress in young adults during the COVID-19 pandemic: evidence of risk and resilience from a longitudinal cohort study. Psychol. Med. 2020, 1–10 (2020).
Brooks, S. K. et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 395, 912–920 (2020).
Jalloh, M. F. et al. Impact of Ebola experiences and risk perceptions on mental health in Sierra Leone, July 2015. BMJ Glob. Health 3, e000471 (2018).
Hawryluck, L. et al. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg. Infect. Dis. 10, 1206–1212 (2004).
Coyle, C. E. & Dugan, E. Social isolation, loneliness and health among older adults. J. Aging Health 24, 1346–1363 (2012).
López, J. et al. Psychological well-being among older adults during the COVID-19 outbreak: a comparative study of the young-old and the old-old adults. Int. Psychogeriatr. 32, 1365–1370 (2020).
Wolfson, J. A., Garcia, T. & Leung, C. W. Food insecurity is associated with depression, anxiety, and stress: evidence from the early days of the COVID-19 pandemic in the United States. Health Equity 5, 64–71 (2021).
Xiong, J. et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J. Affect. Disord. 277, 55–64 (2020).
Schmitz, N., Holley, P., Meng, X., Fish, L. & Jedwab, J. COVID-19 and depressive symptoms: a community-based study in Quebec, Canada. Can. J. Psychiatry 65, 733–735 (2020).
Wilson, J. M. et al. Job insecurity and financial concern during the COVID-19 pandemic are associated with worse mental health. J. Occup. Environ. Med. 62, 686–691 (2020).
Yang, F., Dorrance, K. & Aitken, N. The changes in health and well-being of Canadians with long-term conditions or disabilities since the start of the COVID-19 pandemic. https://www150.statcan.gc.ca/n1/pub/45-28-0001/2020001/article/00082-eng.htm (2020).
De Biase, S., Cook, L., Skelton, D. A., Witham, M. & Ten Hove, R. The COVID-19 rehabilitation pandemic. Age Ageing 49, 696–700 (2020).
Park, S. S. Caregivers’ mental health and somatic symptoms during COVID-19. Gerontol. B Psychol. Sci. Soc. Sci. 76, e235–e240 (2021).
Beach, S. R., Schulz, R., Donovan, H. & Rosland, A. M. Family caregiving during the COVID-19 pandemic. Gerontologist 61, 650–660 (2021).
Holmes, E. A. et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry 7, 547–560 (2020).
Groarke, J. M. et al. Loneliness in the UK during the COVID-19 pandemic: cross-sectional results from the COVID-19 Psychological Wellbeing Study. PLoS ONE 15, e0239698 (2020).
Gearhart, S. et al. The impact of natural disasters on domestic violence: an analysis of reports of simple assault in Florida (1999–2007). Violence Gend. 5, 87–92 (2018).
Rezaeian, M. The association between natural disasters and violence: a systematic review of the literature and a call for more epidemiological studies. J. Res. Med. Sci. 18, 1103–1107 (2013).
Zhang, H. The influence of the ongoing COVID-19 pandemic on family violence in China. J. Fam. Violence https://doi.org/10.1007/s10896-020-00196-8 (2020).
Gadermann, A. C. et al. Examining the impacts of the COVID-19 pandemic on family mental health in Canada: findings from a national cross-sectional study. BMJ Open 11, e042871 (2021).
Andresen, E. M., Byers, K., Friary, J., Kosloski, K. & Montgomery, R. Performance of the 10-item Center for Epidemiologic Studies Depression Scale for caregiving research. SAGE Open Med. 1, 2050312113514576 (2013).
O’Connell, M. E. et al. P1-603: measurement invariance of the Centre for Epidemiological Studies Depression Scale 10-item short form (CES-D-10) in the Canadian Longitudinal Study on Aging. Alzheimers Dement. 14, P570 (2018).
Raina, P. et al. Cohort profile: the Canadian Longitudinal Study on Aging (CLSA). Int. J. Epidemiol. 48, 1752–1753 (2019).
Andresen, E. M., Malmgren, J. A., Carter, W. B. & Patrick, D. L. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am. J. Prev. Med. 10, 77–84 (1994).
Björgvinsson, T., Kertz, S. J., Bigda-Peyton, J. S., McCoy, K. L. & Aderka, I. M. Psychometric properties of the CES-D-10 in a psychiatric sample. Assessment 20, 429–436 (2013).
Miller, W. C., Anton, H. A. & Townson, A. F. Measurement properties of the CESD scale among individuals with spinal cord injury. Spinal Cord 46, 287–292 (2008).
Hughes, M. E., Waite, L. J., Hawkley, L. C. & Cacioppo, J. T. A short scale for measuring loneliness in large surveys: results from two population-based studies. Res. Aging 26, 655–672 (2004).
Washburn, R. A., McAuley, E., Katula, J., Mihalko, S. L. & Boileau, R. A. The Physical Activity Scale for the Elderly (PASE): evidence for validity. J. Clin. Epidemiol. 52, 643–651 (1999).
World Health Organization. Global recommendations on physical activity for health. https://www.who.int/publications/i/item/9789241599979 (2010).
Levasseur, M. et al. Associations between perceived proximity to neighborhood resources, disability, and social participation among community-dwelling older adults: results from the VoisiNuAge study. Arch. Phys. Med. Rehabil. 92, 1979–1986 (2011).
Salazar, A., Ojeda, B., Dueñas, M., Fernández, F. & Failde, I. Simple generalized estimating equations (GEEs) and weighted generalized estimating equations (WGEEs) in longitudinal studies with dropouts: guidelines and implementation in R. Stat. Med. 35, 3424–3448 (2016).
Jones, B. L. & Nagin, D. S. Advances in group-based trajectory modeling and an SAS procedure for estimating them. Sociol. Methods Res. 35, 542–571 (2007).
Dodge, H. H., Shen, C. & Ganguli, M. Application of the pattern-mixture latent trajectory model in an epidemiological study with non-ignorable missingness. J. Data Sci. 6, 247–259 (2008).
Public Health Agency of Canada. Interim national case definition: coronavirus disease (COVID-19). https://open.canada.ca/data/en/dataset/722481c4-c44d-4bb6-9ceb-002022d52f80 (Government of Canada, 2020).
Centers for Disease Control and Prevention. Coronavirus disease 2019 (COVID-19) 2020 interim case definition. https://wwwn.cdc.gov/nndss/conditions/coronavirus-disease-2019-covid-19/case-definition/2020/08/05/ (2020).
Acknowledgements
Funding for support of the CLSA COVID-19 questionnaire-based study is provided by the Juravinski Research Institute, Faculty of Health Sciences, McMaster University, the Provost Fund from McMaster University, the McMaster Institute for Research on Aging, the Public Health Agency of Canada and the government of Nova Scotia. Funding for CLSA is provided by the government of Canada through the Canadian Institutes of Health Research (CIHR), under grant reference LSA 94473, and the Canada Foundation for Innovation and provincial governments (Newfoundland, Nova Scotia, Quebec, Ontario, Manitoba, Alberta and British Columbia). P.R. holds the Raymond and Margaret Labarge Chair in Optimal Aging and Knowledge Application for Optimal Aging, is the director of the McMaster Institute for Research on Aging and the Labarge Centre for Mobility in Aging and holds a Tier 1 Canada Research Chair in Geroscience. L.G. is supported by the McLaughlin Foundation Professorship in Population and Public Health. This research has been conducted using the CLSA Baseline Tracking Dataset version 3.7, Baseline Comprehensive Dataset version 5.1, Follow-up 1 Tracking Dataset version 2.2, Follow-up 1 Comprehensive Dataset version 3.0, CLSA Sample Weights version 1.2 and COVID-19 questionnaire data under application ID 21CON001.
Author information
Authors and Affiliations
Consortia
Contributions
P.R., C.W., L.G., S.K., J.M. and N.B. designed the CLSA COVID-19 study and contributed to the revision of the manuscript. U.E.O., N.S., D.J., G. Maimon and M.T. conducted the data analysis. P.R. and D.J. wrote the manuscript with input from all authors. The members of the CLSA team have contributed to the collection of the data across Canada.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information Nature Aging thanks the anonymous reviewers for their contribution to the peer review of this work.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Raina, P., Wolfson, C., Griffith, L. et al. A longitudinal analysis of the impact of the COVID-19 pandemic on the mental health of middle-aged and older adults from the Canadian Longitudinal Study on Aging. Nat Aging 1, 1137–1147 (2021). https://doi.org/10.1038/s43587-021-00128-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s43587-021-00128-1
This article is cited by
-
The impact of COVID-19 on the mental health of older sexual minority Canadians in the CLSA
BMC Geriatrics (2023)
-
Lived Experiences of the COVID-19 Pandemic Among the Vietnamese Population in the Region of Peel
Journal of Racial and Ethnic Health Disparities (2023)
-
The Buffering Role of Self-compassion in the Association Between Loneliness with Depressive Symptoms: A Cross-Sectional Survey Study Among Older Adults Living in Residential Care Homes During COVID-19
International Journal of Mental Health and Addiction (2023)
-
Increased prevalence of loneliness and associated risk factors during the COVID-19 pandemic: findings from the Canadian Longitudinal Study on Aging (CLSA)
BMC Public Health (2023)
-
Obesity and adverse childhood experiences in relation to stress during the COVID-19 pandemic: an analysis of the Canadian Longitudinal Study on Aging
International Journal of Obesity (2023)