Abstract
Alzheimer’s disease (AD) is a form of dementia characterized by amyloid-β plaques and tau neurofibrillary tangles that progressively disrupt neural circuits in the brain. The signaling networks underlying AD pathological changes are poorly characterized at the phosphoproteome level. Using mass spectrometry, we analyzed the proteome and tyrosine, serine and threonine phosphoproteomes of temporal cortex tissue from patients with AD and aged-matched controls. We identified cocorrelated peptide clusters that were linked to varying levels of phospho-tau, oligodendrocyte, astrocyte, microglia and neuron pathologies. We found that neuronal synaptic protein abundances were strongly anti-correlated with markers of microglial reactivity. We also observed that phosphorylation sites on kinases targeting tau and other new signaling factors were correlated with these peptide modules. Finally, we used data-driven statistical modeling to identify individual peptides and peptide clusters that were predictive of AD histopathologies. Together, these results build a map of pathology-associated phosphorylation signaling events occurring in AD.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
Data supporting findings from this study are available from the lead contact, F.M.W., upon request. The MS raw and searched proteomics data files have been deposited to the ProteomeXchange Consortium via the PRIDE114 partner repository with the dataset accession no. PXD020087 and 10.6019/PXD020087. Patient clinical histopathology data and MS-run information are available in Supplementary Data 1. Processed peptide data are available in Supplementary Data 2. All calculated peptide feature correlations and group fold-changes are available in Supplementary Data 4 and 5. Cell type-specific sequencing data were downloaded from BrainRNASeq (https://web.stanford.edu/group/barres_lab/brainseq2/TableS4-HumanMouseMasterFPKMList.xlsx). Kinase–substrate and homology mapping data were downloaded from PhosphoSite Plus (https://www.phosphosite.org/downloads/Kinase_Substrate_Dataset.gz, https://phosphosite.org/downloads/Phosphorylation_site_dataset.gz). BRSK1 and BRSK2 substrates were derived from MaxQuant processed ‘_phosphoSites_filtered_imputed.txt’ file, shared directly by Tamir et al.112. For GO analysis, ‘gene2go’ (ftp://ftp.ncbi.nlm.nih.gov/gene/DATA/gene2go.gz) and ‘go-basic.obo’ (http://geneontology.org/ontology/go-basic.obo) were downloaded using goatools. Mouse phosphoproteome data for analysis was sourced from Morshed et al.22: dataset EV1. Mouse source MS data are available on PRIDE via accession no. PXD018757.
Code availability
The proteomics data integration software is available on GitHub (https://github.com/white-lab/pyproteome). This repository also includes detailed software for concatenating peptide fractions on a Gibson FC 204 Fraction Collection (https://github.com/white-lab/fc-cycle) and an updated tool for validating PSMs (https://github.com/white-lab/CAMV). Sources for other code used in the present study are indicated in Supplementary Information.
References
2020 Alzheimer’s disease facts and figures. Alzheimers Dement. 16, 391–460 (2020).
Musiek, E. S. & Holtzman, D. M. Three dimensions of the amyloid hypothesis: time, space and ‘wingmen’. Nat. Neurosci. 18, 800–806 (2015).
De Strooper, B. & Karran, E. The cellular phase of Alzheimer’s disease. Cell 164, 603–615 (2016).
Long, J. M. & Holtzman, D. M. Alzheimer disease: an update on pathobiology and treatment strategies. Cell 179, 312–339 (2019).
Ittner, L. M. & Götz, J. Amyloid-β and tau—a toxic pas de deux in Alzheimer’s disease. Nat. Rev. Neurosci. 12, 65–72 (2011).
Cavallini, A. et al. An unbiased approach to identifying tau kinases that phosphorylate tau at sites associated with Alzheimer disease. J. Biol. Chem. 288, 23331–23347 (2013).
Jicha, G. A. et al. cAMP-dependent protein kinase phosphorylations on Tau in Alzheimer’s disease. J. Neurosci. 19, 7486–7494 (1999).
Alfonso, S. I. et al. Gain-of-function mutations in protein kinase Cα (PKCα) may promote synaptic defects in Alzheimer’s disease. Sci. Signal. 9, ra47 (2016).
Callender, J. A. et al. Protein kinase Cα gain-of-function variant in Alzheimer’s disease displays enhanced catalysis by a mechanism that evades down-regulation. Proc. Natl Acad. Sci. USA 115, E5497–E5505 (2018).
Reichenbach, N. et al. Inhibition of Stat3‐mediated astrogliosis ameliorates pathology in an Alzheimer’s disease model. EMBO Mol. Med. 11, e9665 (2019).
Haim, L. Ben et al. The JAK/STAT3 pathway is a common inducer of astrocyte reactivity in Alzheimer’s and Huntington’s diseases. J. Neurosci. 35, 2817–2829 (2015).
Styr, B. & Slutsky, I. Imbalance between firing homeostasis and synaptic plasticity drives early-phase Alzheimer’s disease. Nat. Neurosci. 21, 463–473 (2018).
Seo, J. et al. Inhibition of p25/Cdk5 attenuates tauopathy in mouse and iPSC models of frontotemporal dementia. J. Neurosci. 37, 9917–9924 (2017).
Seo, J. et al. Activity-dependent p25 generation regulates synaptic plasticity and aβ-induced cognitive impairment. Cell 157, 486–498 (2014).
Rigbolt, K. T. G. & Blagoev, B. Quantitative phosphoproteomics to characterize signaling networks. Semin. Cell Dev. Biol. https://doi.org/10.1016/j.semcdb.2012.05.006 (2012).
Riley, N. M. & Coon, J. J. Phosphoproteomics in the age of rapid and deep proteome profiling. Anal. Chem. https://doi.org/10.1021/acs.analchem.5b04123 (2016).
Lemeer, S. & Heck, A. J. The phosphoproteomics data explosion. Curr. Opin. Chem. Biol. https://doi.org/10.1016/j.cbpa.2009.06.022 (2009).
Ficarro, S. B. et al. Phosphoproteome analysis by mass spectrometry and its application to Saccharomyces cerevisiae. Nat. Biotechnol. 20, 301–305 (2002).
Zhang, Y. et al. Time-resolved mass spectrometry of tyrosine phosphorylation sites in the epidermal growth factor receptor signaling network reveals dynamic modules. Mol. Cell Proteomics 4, 1240–1250 (2005).
White, F. M. & Wolf-Yadlin, A. Methods for the analysis of protein phosphorylation-mediated cellular signaling networks. Annu. Rev. Anal. Chem. https://doi.org/10.1146/annurev-anchem-071015-041542 (2016).
Bai, B. et al. Deep multilayer brain proteomics identifies molecular networks in Alzheimer’s disease progression. Neuron 105, 975–991.e7 (2020).
Morshed, N. et al. Phosphoproteomics identifies microglial Siglec‐F inflammatory response during neurodegeneration. Mol. Syst. Biol. 16, e9819 (2020).
Tagawa, K. et al. Comprehensive phosphoproteome analysis unravels the core signaling network that initiates the earliest synapse pathology in preclinical Alzheimer’s disease brain. Hum. Mol. Genet. 24, 540–558 (2015).
Dammer, E. B. et al. Quantitative phosphoproteomics of Alzheimer’s disease reveals cross-talk between kinases and small heat shock proteins. Proteomics 15, 508–519 (2015).
Marttinen, M. et al. A multiomic approach to characterize the temporal sequence in Alzheimer’s disease-related pathology. Neurobiol. Dis. 124, 454–468 (2019).
Johnson, E. C. B. et al. Large-scale proteomic analysis of Alzheimer’s disease brain and cerebrospinal fluid reveals early changes in energy metabolism associated with microglia and astrocyte activation. Nat. Med. 26, 769–780 (2020).
Ping, L. et al. Global quantitative analysis of the human brain proteome in Alzheimer’s and Parkinson’s disease. Sci. Data 5, 180036 (2018).
Wingo, A. P. et al. Large-scale proteomic analysis of human brain identifies proteins associated with cognitive trajectory in advanced age. Nat. Commun. 10, 1619 (2019).
Di Domenico, F. et al. Quantitative proteomics analysis of phosphorylated proteins in the hippocampus of Alzheimer’s disease subjects. J. Proteomics 74, 1091–1103 (2011).
Triplett, J. C., Swomley, A. M., Cai, J., Klein, J. B. & Butterfield, D. A. Quantitative phosphoproteomic analyses of the inferior parietal lobule from three different pathological stages of Alzheimer’s disease. J. Alzheimers Dis. 49, 45–62 (2016).
Mathys, H. et al. Single-cell transcriptomic analysis of Alzheimer’s disease. Nature 570, 332–337 (2019).
Kunkle, B. W. et al. Genetic meta-analysis of diagnosed Alzheimer’s disease identifies new risk loci and implicates Aβ, tau, immunity and lipid processing. Nat. Genet. 51, 414–430 (2019).
Mattsson, N. et al. Association of plasma neurofilament light with neurodegeneration in patients with Alzheimer disease. JAMA Neurol. https://doi.org/10.1001/jamaneurol.2016.6117 (2017).
Mattsson, N., Cullen, N. C., Andreasson, U., Zetterberg, H. & Blennow, K. Association between longitudinal plasma neurofilament light and neurodegeneration in patients with Alzheimer disease. JAMA Neurol. https://doi.org/10.1001/jamaneurol.2019.0765 (2019).
Preische, O. et al. Serum neurofilament dynamics predicts neurodegeneration and clinical progression in presymptomatic Alzheimer’s disease. Nat. Med. https://doi.org/10.1038/s41591-018-0304-3 (2019).
Davidsson, P., Jahn, R., Bergquist, J., Ekman, R. & Blennow, K. Synaptotagmin, a synaptic vesicle protein, is present in human cerebrospinal fluid—a new biochemical marker for synaptic pathology in Alzheimer disease? Mol. Chem. Neuropathol. https://doi.org/10.1007/BF02815094 (1996).
Galasko, D. et al. Synaptic biomarkers in CSF aid in diagnosis, correlate with cognition and predict progression in MCI and Alzheimer’s disease. Alzheimer’s Dement. Transl. Res. Clin. Interv. https://doi.org/10.1016/j.trci.2019.11.002 (2019).
Wingo, A. P. et al. Shared proteomic effects of cerebral atherosclerosis and Alzheimer’s disease on the human brain. Nat. Neurosci. https://doi.org/10.1038/s41593-020-0635-5 (2020).
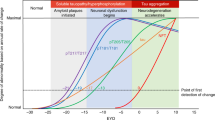
Jack, C. R. et al. Tracking pathophysiological processes in Alzheimer’s disease: an updated hypothetical model of dynamic biomarkers. Lancet Neurol. 12, 207–216 (2013).
Janelidze, S. et al. Cerebrospinal fluid p-tau217 performs better than p-tau181 as a biomarker of Alzheimer’s disease. Nat. Commun. 11 (2020).
Dujardin, S. et al. Tau molecular diversity contributes to clinical heterogeneity in Alzheimer’s disease. Nat. Med. https://doi.org/10.1038/s41591-020-0938-9 (2020).
Wesseling, H. et al. Tau PTM profiles identify patient heterogeneity and stages of Alzheimer’s disease. Cell https://doi.org/10.1016/j.cell.2020.10.029 (2020).
Harauz, G. & Boggs, J. M. Myelin management by the 18.5-kDa and 21.5-kDa classic myelin basic protein isoforms. J. Neurochem. 125, 334–361 (2013).
Lin, H., Lin, T. Y. & Juang, J. L. Abl deregulates Cdk5 kinase activity and subcellular localization in Drosophila neurodegeneration. Cell Death Differ. 14, 607–615 (2007).
Zukerberg, L. R. et al. Cables links Cdk5 and c-Abl and facilitates Cdk5 tyrosine phosphorylation, kinase upregulation, and neurite outgrowth Cdks are involved in events unrelated to cell division. A function of Cdk5 has been demonstrated only in the development of the nervous system. Neuron 26, 633–646 (2000).
Muñoz, I. M. et al. Phosphoproteomic screening identifies physiological substrates of the CDKL5 kinase. EMBO J. 37, e99559 (2018).
Mikolcevic, P. et al. Cyclin-dependent kinase 16/PCTAIRE kinase 1 is sctivated by cyclin Y and is essential for spermatogenesis. Mol. Cell. Biol. 32, 868–879 (2012).
Chaput, D., Kirouac, L., Stevens, S. M., Padmanabhan, J. & Padmanabhan, J. Potential role of PCTAIRE-2, PCTAIRE-3 and P-Histone H4 in amyloid precursor protein-dependent Alzheimer pathology. Oncotarget 7, 8481–8497 (2016).
Patrick, G. N. et al. Conversion of p35 to p25 deregulates Cdk5 activity and promotes neurodegeneration. Nature 402, 615–622 (1999).
Herskovits, A. Z. & Davies, P. The regulation of tau phosphorylation by PCTAIRE 3: Implications for the pathogenesis of Alzheimer’s disease. Neurobiol. Dis. 23, 398–408 (2006).
Hensley, K. et al. p38 kinase is activated in the Alzheimer’s disease brain. J. Neurochem. 72, 2053–2058 (1999).
Ghosh, A. & Giese, K. P. Calcium/calmodulin-dependent kinase II and Alzheimer’s disease. Mol. Brain 8, 78 (2015).
Yarza, R., Vela, S., Solas, M. & Ramirez, M. J. c-Jun N-terminal kinase (JNK) signaling as a therapeutic target for Alzheimer’s disease. Front. Pharmacol. 6, 321 (2015).
Lisnock, J. et al. Activation of JNK3 alpha 1 requires both MKK4 and MKK7: kinetic characterization of in vitro phosphorylated JNK3 alpha 1. Biochemistry 39, 3141–3148 (2000).
Brichkina, A. et al. P38MAPK builds a hyaluronan cancer niche to drive lung tumorigenesis. Genes Dev. 30, 2623–2636 (2016).
Seidler, J., Adal, M., Kübler, D., Bossemeyer, D. & Lehmann, W. D. Analysis of autophosphorylation sites in the recombinant catalytic subunit alpha of cAMP-dependent kinase by nano-UPLC-ESI-MS/MS. Anal. Bioanal. Chem. 395, 1713–1720 (2009).
Geng, J. et al. Kinases Mst1 and Mst2 positively regulate phagocytic induction of reactive oxygen species and bactericidal activity. Nat. Immunol. 16, 1142–1152 (2015).
Robison, A. J., Winder, D. G., Colbran, R. J. & Bartlett, R. K. Oxidation of calmodulin alters activation and regulation of CaMKII. Biochem. Biophys. Res. Commun. https://doi.org/10.1016/j.bbrc.2007.02.087 (2007).
Giese, K. P., Fedorov, N. B., Filipkowski, R. K. & Silva, A. J. Autophosphorylation at Thr286 of the α calcium-calmodulin kinase II in LTP and learning. Science 279, 870–873 (1998).
Boggon, T. J. & Eck, M. J. Structure and regulation of Src family kinases. Oncogene 23, 7918–7927 (2004).
Pan, Q. et al. Cdk5 targets active Src for ubiquitin-dependent degradation by phosphorylating Src(S75). Cell Mol. Life Sci. 68, 3425–3436 (2011).
Weir, M. E. et al. Novel autophosphorylation sites of Src family kinases regulate kinase activity and SH2 domain-binding capacity. FEBS Lett. 590, 1042–1052 (2016).
Manser, C., Vagnoni, A., Guillot, F., Davies, J. & Miller, C. C. J. Cdk5/p35 phosphorylates lemur tyrosine kinase-2 to regulate protein phosphatase-1C phosphorylation and activity. J. Neurochem. 121, 343–348 (2012).
Brunton, V. G. et al. Identification of Src-specific phosphorylation site on focal adhesion kinase: dissection of the role of Src SH2 and catalytic functions and their consequences for tumor cell behavior. Cancer Res. 65, 1335–1342 (2005).
Fu, H. L. et al. Glycosylation at Asn211 regulates the activation state of the discoidin domain receptor 1 (DDR1). J. Biol. Chem. 289, 9275–9287 (2014).
Hebron, M. et al. Discoidin domain receptor inhibition reduces neuropathology and attenuates inflammation in neurodegeneration models. J. Neuroimmunol. 311, 1–9 (2017).
Fowler, A. J. et al. Multikinase Abl/DDR/Src inhibition produces optimal effects for tyrosine kinase inhibition in neurodegeneration. Drugs R. D. 19, 149–166 (2019).
Fowler, A. J. et al. Discoidin domain receptor 1 is a therapeutic target for neurodegenerative diseases. Hum. Mol. Genet. https://doi.org/10.1093/hmg/ddaa177 (2020).
Reddy, R. J. et al. Early signaling dynamics of the epidermal growth factor receptor. Proc. Natl Acad. Sci. USA 113, 3114–3119 (2016).
Hornbeck, P. V. et al. PhosphoSitePlus, 2014: mutations, PTMs and recalibrations. Nucleic Acids Res. 43, D512–D520 (2015).
Okuno, S., Kitani, T. & Fujisawa, H. Regulation of Ca2+/calmodulin-dependent protein kinase kinase alpha by cAMP-dependent protein kinase: I. Biochemical analysis. J. Biochem. 130, 503–513 (2001).
Bürklen, T. S. et al. The creatine kinase/creatine connection to Alzheimer’s disease: CK-inactivation, APP–CK complexes and focal creatine deposits. J. Biomed. Biotechnol. 2006, 35936 (2006).
Aksenov, M., Aksenova, M., Butterfield, D. A. & Markesbery, W. R. Oxidative modification of creatine kinase BB in Alzheimer’s disease brain. J. Neurochem. 74, 2520–2527 (2000).
Gonzales, E. B., Smith, R. N. & Agharkar, A. S. A review of creatine supplementation in age-related diseases: more than a supplement for athletes. F1000Research https://doi.org/10.12688/f1000research.5218.1 (2014).
Matthews, R. T. et al. Neuroprotective effects of creatine and cyclocreatine in animal models of Huntington’s disease. J. Neurosci. 18, 156–163 (1998).
Ulland, T. K. et al. TREM2 maintains microglial metabolic fitness in Alzheimer’s disease. Cell 170, 649–663 (2017).
Carbajosa, G. et al. Loss of Trem2 in microglia leads to widespread disruption of cell coexpression networks in mouse brain. Neurobiol. Aging 69, 151–166 (2018).
Kirouac, L., Rajic, A. J., Cribbs, D. H. & Padmanabhan, J. Activation of Ras-ERK signaling and GSK-3 by amyloid precursor protein and amyloid beta facilitates neurodegeneration in Alzheimer’s disease. eNeuro https://doi.org/10.1523/ENEURO.0149-16.2017 (2017).
Arstikaitis, P. et al. Paralemmin-1, a modulator of filopodia induction is required for spine maturation. Mol. Biol. Cell 19, 2026–2038 (2008).
Zorzetto, M. et al. Complement C4A and C4B gene copy number study in Alzheimer’s disease patients. Curr. Alzheimer Res. https://doi.org/10.2174/1567205013666161013091934 (2016).
Sellgren, C. M. et al. Increased synapse elimination by microglia in schizophrenia patient-derived models of synaptic pruning. Nat. Neurosci. https://doi.org/10.1038/s41593-018-0334-7 (2019).
Hong, S. et al. Complement and microglia mediate early synapse loss in Alzheimer mouse models. Science 8373, 712–716 (2016).
Beckmann, N. D. et al. Multiscale causal networks identify VGF as a key regulator of Alzheimer’s disease. Nat. Commun. 11, 3942 (2020).
Zhang, Y. et al. Purification and characterization of progenitor and mature human astrocytes reveals transcriptional and functional differences with mouse. Neuron 89, 37–53 (2016).
Zhang, Y. et al. An RNA-sequencing transcriptome and splicing database of glia, neurons, and vascular cells of the cerebral cortex. J. Neurosci. 34, 11929–11947 (2014).
Cullen, N. C. et al. Individualized prognosis of cognitive decline and dementia in mild cognitive impairment based on plasma biomarker combinations. Nat. Aging https://doi.org/10.1038/s43587-020-00003-5 (2020).
Hong, S., Dissing-Olesen, L. & Stevens, B. New insights on the role of microglia in synaptic pruning in health and disease. Curr. Opin. Neurobiol. 36, 128–134 (2016).
Yilmaz, M. et al. Overexpression of schizophrenia susceptibility factor human complement C4A promotes excessive synaptic loss and behavioral changes in mice. Nat. Neurosci. https://doi.org/10.1038/s41593-020-00763-8 (2020).
Sekar, A. et al. Schizophrenia risk from complex variation of complement component 4. Nature 530, 177–183 (2016).
Ferreira, S. et al. Oligodendrogenesis increases in hippocampal grey and white matter prior to locomotor or memory impairment in an adult mouse model of tauopathy. Eur. J. Neurosci. https://doi.org/10.1111/ejn.14726 (2020).
Birdsill, A. C., Walker, D. G., Lue, L. F., Sue, L. I. & Beach, T. G. Postmortem interval effect on RNA and gene expression in human brain tissue. Cell Tissue Bank. 12, 311–318 (2011).
Walker, D. G. et al. Characterization of RNA isolated from eighteen different human tissues: results from a rapid human autopsy program. Cell Tissue Bank. 17, 361–375 (2016).
Emdal, K. B. et al. Characterization of in vivo resistance to osimertinib and JNJ-61186372, an EGFR/Met bi-specific antibody, reveals unique and consensus mechanisms of resistance. Mol. Cancer Ther. https://doi.org/10.1158/1535-7163.MCT-17-0413 (2017).
Huang, P. H. et al. Phosphotyrosine signaling analysis of site-specific mutations on EGFRvIII identifies determinants governing glioblastoma cell growth. Mol. Biosyst. 6, 1227–1237 (2010).
Miraldi, E. R. et al. Molecular network analysis of phosphotyrosine and lipid metabolism in hepatic PTP1b deletion mice. Integr. Biol. (United Kingdom) 5, 940–963 (2013).
Zecha, J. et al. TMT labeling for the masses: a robust and cost-efficient, in-solution labeling approach. Mol. Cell. Proteomics 18, 1468–1478 (2019).
Wolf-Yadlin, A. et al. Effects of HER2 overexpression on cell signaling networks governing proliferation and migration. Mol. Syst. Biol. 2, 54 (2006).
Johnson, H. & White, F. M. Toward quantitative phosphotyrosine profiling in vivo. Semin. Cell Dev. Biol. 23, 854–862 (2012).
Johnson, H. et al. Molecular characterization of EGFR and EGFRvIII signaling networks in human glioblastoma tumor xenografts. Mol. Cell. Proteomics 11, 1724–1740 (2012).
Gajadhar, A. S. et al. Phosphotyrosine signaling analysis in human tumors is confounded by systemic ischemia-driven artifacts and intra-specimen heterogeneity. Cancer Res. 75, 1495–1503 (2015).
Taus, T. et al. Universal and confident phosphorylation site localization using phosphoRS. J. Proteome Res. https://doi.org/10.1021/pr200611n (2011).
Maes, E. et al. CONSTANd: a normalization method for isobaric labeled spectra by constrained optimization. Mol. Cell. Proteomics 15, 2779–2790 (2016).
Pedregosa, F. et al. Scikit-learn: machine learning in python. J. Mach. Learn. Res. 12, 2825–2830 (2012).
Virtanen, P. et al. SciPy 1.0: fundamental algorithms for scientific computing in Python. Nat. Methods https://doi.org/10.1038/s41592-019-0686-2 (2020).
Van Der Walt, S., Colbert, S. C. & Varoquaux, G. The NumPy array: a structure for efficient numerical computation. Comput. Sci. Eng. 13, 22–30 (2011).
McKinney, W. Data structures for statistical computing in Python. In Proceedings of the 9th Python in Science Conference (eds van der Walt, S. & Millman, K. J.) 51–56 (SciPy, 2010).
Waskom, M. mwaskom/seaborn: v0.9.0. Zenodo https://doi.org/10.5281/zenodo.1313201 (2018).
Hunter, J. D. Matplotlib: a 2D graphics environment. Comput. Sci. Eng. 9, 99–104 (2007).
Gaudet, S. et al. A compendium of signals and responses triggered by prodeath and prosurvival cytokines. Mol. Cell. Proteomics 4, 1569–1590 (2005).
Metz, K. S. et al. Coral: clear and customizable visualization of human kinome data. Cell Syst. 7, 347–350 (2018).
Krug, K. et al. A curated resource for phosphosite-specific signature analysis. Mol. Cell. Proteomics 18, 576–593 (2018).
Tamir, T. Y. et al. Gain-of-function genetic screen of the kinome reveals BRSK2 as an inhibitor of the NRF2 transcription factor. J. Cell Sci. https://doi.org/10.1242/jcs.241356 (2020).
Klopfenstein, D. V. et al. GOATOOLS: a python library for gene ontology analyses. Sci. Rep. https://doi.org/10.1038/s41598-018-28948-z (2018).
Perez-Riverol, Y. et al. The PRIDE database and related tools and resources in 2019: improving support for quantification data. Nucleic Acids Res. https://doi.org/10.1093/nar/gky1106 (2019).
Acknowledgements
We thank members of the laboratories of F.M.W., L.-H. Tsai and D.A.L. for numerous discussions and feedback. N.M. was partially supported by the NIH Biotechnology Training grant (no. T32GM008334). M.J.L. was partially supported through the US Army Research Office Cooperative Agreement (no. W911NF-19-2-0026) for the Institute for Collaborative Biotechnologies and the National Science Foundation Graduate Research Fellowship Program (award no. 1745302). We thank the BSHRI Brain and Body Donation Program of Sun City, AZ for the provision of human brain tissue. The Brain and Body Donation Program has been supported by the National Institute of Neurological Disorders and Stroke (U24 NS072026 National Brain and Tissue Resource for Parkinson’s Disease and Related Disorders), the National Institute on Aging (P30 AG19610 Arizona Alzheimer’s Disease Core Center), the Arizona Department of Health Services (contract no. 211002, Arizona Alzheimer’s Research Center), the Arizona Biomedical Research Commission (contract nos. 4001, 0011, 05-901 and 1001 to the Arizona Parkinson’s Disease Consortium) and the Michael J. Fox Foundation for Parkinson’s Research.
Author information
Authors and Affiliations
Contributions
N.M. and F.M.W. designed the study. D.M. collected human brain tissue samples. N.M. and F.H.R. collected proteomics datasets. N.M. wrote proteomics data integration and enrichment software. N.M. and M.J.L. performed statistical analyses with methodology and analysis oversight from D.A.L. N.M., M.J.L. and F.M.W. wrote the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information Nature Aging thanks the anonymous reviewers for their contribution to the peer review of this work.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Proteome and phosphoproteome dataset statistics and quantification reproducibility.
a–c, Venn diagram showing peptide overlap between (a) pTyr sites, (b) pSer/pThr sites, and (c) proteins identified in each 10-plex analysis. d, Cumulative number of peptides identified compared to the number of patients with peptide quantification. e-f, Reproducibility analysis of peptide quantification after data integration and normalization. Shown are the log2 quantification ratios between two separate brain samples from patients (e) 06-49 and (f) 06-03. Peptides are separated on the x-axis by log10 total TMT intensity from all PSMs in both 10-plex analyses. The standard deviation of abundance ratios and Pearson’s correlation coefficient between all peptide replicates are listed in the panels. g,h, Reproducibility of peptide quantification between technical replicates of peptide aliquots for each TMT10-plex analysis. Shown are (g) the standard deviation of abundance ratios and (h) the Pearson’s correlation coefficient calculated over all peptides. Box plot indicates quartiles, and whiskers indicate the last datum within 1.5 interquartile range. Individual data points are shown for each technical replicate.
Extended Data Fig. 2 Accessory clustering and dataset comparison analyses.
a-b, Properties of clusters generated by clustering with increasing number of clusters. Shown are the (a) mean Pearson correlation coefficient for cluster peptides with their respective cluster centroid, averaged over all clusters, and (b) minimum absolute Pearson correlation coefficient for cluster peptides with their respective cluster centroid, summed and normalized over all clusters. Dotted line indicates the final cluster count used for downstream analysis. c, Co-correlation heatmap between all cluster centroids, group by cluster. Selected named clusters are shown on the y-axis. d, Phosphopeptide composition of all peptides associated with cluster centroids. Peptides are labeled as ‘pY’ if they contain at least one pTyr site, ‘pST’ if they contain at least one pSer or pThr site, or ‘no phospho’ if they are not phosphorylated. Statistics calculations are same as Fig. 2g. e, Binomial enrichment for proteome module marker proteins identified in Johnson et al. (2020). Heatmap shows log-odds enrichment (LOE) values for the overlap of marker transcripts with pTyr, pSer/pThr, and proteome datasets that are correlated with cluster centroids. f, Binomial enrichment for single-nuclei populations markers identified in Mathys et al. (2019). Legend is same as (e). g, Venn diagram overlap between proteins correlated with Oligo in our dataset, M2 Oligo proteome module from (e) and Oli0 marker transcripts from (f). Numbers indicate the total number of proteins in each overlapping set and selected protein names are shown. h, Transcript log2 Fold Change values Oli0 population from Mathys et al. (2019) for markers of the Oligo cluster.
Extended Data Fig. 3 Peptide cluster principle component and stratification analyses.
a, Principal component analysis (PCA) of peptides quantified in all samples. Patients are colored by (a) AD or ND status, (b) Tau, (c) Oligo, (d) Astro, (e) Micro, (f) pNeuro, and (g) Neuro cluster centroid values. h–j, PCA of samples colored by patient stratifications using (h) Tau and Oligo, (i) Astro and Micro, and (j) pNeuro and Neuro cluster centroids. k,l, Patients numbers for (k) Astro;Micro or (l) pNeuro;Neuro patient stratifications. m,n, Overlap between Tau;Oligo and (m) Astro;Micro or (n) pNeuro;Neuro patient stratifications.
Extended Data Fig. 4 Peptide correlation analyses.
a,b, Distribution of Spearman’s correlation coefficient for peptides identified in ≥15 patients with (a) scrambled cluster centroids or (b) true cluster centroids. c,d, Distribution of Spearman’s correlation p-values for peptides identified in ≥15 patients with (c) scrambled cluster centroids or (d) true cluster centroids. (e–g) Venn diagram showing the number of correlated peptides with (e) Tau and Oligo, (f) Astro and Micro, and (g) pNeuro and Neuro cluster centroids. Plots include the total number of associated peptides for each cluster, as well as the number of overlapping peptides between similar clusters. h, Heatmap showing phosphopeptide fold changes for peptides that are significantly correlated with Tau cluster centroid. Samples are ordered by centroid values. Left color bars indicate proteins that were predicted to be cell type-specific. Green = Astrocyte, Purple = Oligodendrocyte, Yellow = Neuron, Blue = Microglia. Missing values are indicated as white boxes. i, Heatmap showing fold changes cell type-specific proteins that are significantly correlated with Oligo cluster centroid. Samples are ordered by centroid value. Left color bar legend is same as (h).
Extended Data Fig. 5 Analyses of peptide partial cluster correlation.
a-d, Fold changes for (a) MAPT pS579 (pS262), (b) MAPT pT534 (pS217), (c) MBP protein, and (d) PLP1 protein. Protein levels were estimated from the median abundance of all unmodified peptides that map uniquely to that protein. Values are normalized to the median of Tau− Oligo− patients. Box plot indicates quartiles, and whiskers indicate the last datum within 1.5 interquartile range. Individual data points are shown for each sample. Stars indicate two-sided t-test values for each group compared with Tau− Oligo− and Tau− Oligo+ patients (n = 8-14 patients in each group). ns, not significant (p > 0.05); * p < 5e-2, **p < 1e-2; ***p < 1e-3; ****p < 1e-4. e, All peptides mapping to the peripheral nervous system (PNS) isoform of MAPT. Colored bars indicate directional correlation for non-phosphorylated peptides. Red = correlated, blue = anti-correlated, grey = uncorrelated, light-grey = only phosphopeptides were seen in that region. Colored circles indicate phosphorylation sites that were quantified. Red circle = correlated, blue circle = anti-correlated, black circle = uncorrelated. Green dividers indicate the borders between the N-terminal projection, proline-rich domain, microtubule-binding repeats, and C-terminal flanking region. f, All peptides mapping to the full-length isoform of MBP. Legend is same as (e). g–r, Fold changes across Astro+ and Micro+ groups for (g) GFAP protein, (h) VIM protein, (i) GNA13 protein, (j) AIF1 protein, (k) ITGB2 protein, (l) SPP1 pS270, (m) C1QA protein, (n) C1QB protein, (o) C1QC protein, (p) C3 protein, (q) C4A protein, and (r) C4B protein. Legend is same as (a-d). Stars indicate two-sided t-test values for each group compared with Astro− Micro− and Astro+ Micro− patients (n = 12-14 patients in each group). ns, not significant (p > 0.05); * p < 5e-2, **p < 1e-2; ***p < 1e-3; ****p < 1e-4.
Extended Data Fig. 6 Tau kinase and CDK phosphosite abundances.
a-d, Fold changes for (a) TNIK pS680, (b) BRSK1 pS443, (c) BRSK2 pS423, and (d) TTBK1 pS483 across Tau and Oligo groups. Values are normalized to the median of Tau− Oligo− patients. Box plot indicates quartiles, and whiskers indicate the last datum within 1.5 interquartile range. Individual data points are shown for each sample. Stars indicate two-sided t-test values for each group compared with Tau− Oligo− and Tau− Oligo+ patients (n = 8-14 patients in each group). ns, not significant (p > 0.05); * p < 5e-2, **p < 1e-2; ***p < 1e-3; ****p < 1e-4. e–h, Fold changes for all non-phospho peptides and significantly changing phosphosites on (e) TNIK, (f) BRSK1, (g) BRSK2, (h) TTBK1. Each dot indicates one unique peptide. Phosphosite ranges are estimated from peptides with missed cleavages. Box plot indicates quartiles, and whiskers indicate the last datum within 1.5 interquartile range. Phosphosites labeled with ‘*’ are on peptides that map ambiguously to more than one protein. i–m, Fold changes for (i) CDK5 pY15, (j) CDKL5 pY171, (k) CDK16 pS153, (l) CDK17 pS180, and (m) CDK18 pS132 across Tau and Oligo groups. Legend is same as (a-d). n–r, Fold changes for all non-phospho peptides and significantly changing phosphosites on (n) CDK5, (o) CDKL5, (p) CDK16, (q) CDK17, and (r) CDK18. Legend is same as (e-h).
Extended Data Fig. 7 Accessory kinome analyses.
a, Maximum phosphosite fold changes and median protein abundances for all kinases shown in Fig. 4d. Changes are calculated for each Tau;Oligo group compared to Tau−;Oligo−. Stars indicate two-sided t-test values for each group compared with Tau− Oligo− patients (n = 8-14 patients in each group). *p < 5e-2; **p < 1e-3; ***p < 1e-4. b–m, Fold changes for all non-phospho peptides and significantly changing phosphosites on (b) MAPK8 (c) MAPK10, (d) MAPK11, (e) MAPK14, (f) PRKACA, (g) PRKCA, (h) all CaMKII subunits, (i) SRC, (j) LMTK2, (k) PTK2, (l) DDR1, and (m) EGFR. Legend is same as Extended Data Figure 6e.
Extended Data Fig. 8 Kinase-substrate and AD mouse model analyses.
a–d, Volcano plots showing Spearman’s correlation coefficient and p-values between PKA Cα substrates and (a) Tau, (b) Astro, (d) Oligo, and (d) pNeuro cluster centroids. Labels are colored using the same scheme as Extended Data Figure 4h. e, Number of phosphosites from AD mouse models identified in three mouse models of neurodegeneration that could be translated to human and were significantly correlated with each cluster centroid and shared directional changes. f, Phosphoproteins that were identified to have at least one shared phosphosite with three mouse models of neurodegeneration. Proteins are shown as a Venn diagram between downregulated phosphosites and pNeuro or Neuro cluster centroids.
Extended Data Fig. 9 PLSR accessory analyses
a–c, Latent variable plots for multivariate PLSR analysis for X scores. Points are colored by patient (a) NIA-R score, (b) CERAD-NP score, and (c) TangleT score. d, K-fold validation of the multivariate PLSR model for all included histopathology variables. R2 and Q2 values are shown for training and test data predictions respectively. e, Scatter plot showing PLSR patient scores generated from cluster centroids compared with subsets of the matrix of peptides quantified in all patients. f, Fold changes for all non-phospho peptides and significantly changing phosphosites on CKB. Legend is same as Extended Data Fig. 6e. g–j, Fold changes for (g) SYN1, (h) SYT1, (i) CAMKK1 pS52, and (j) CASKIN pS935 across pNeuro and Neuro groups. Box plot indicates quartiles, and whiskers indicate the last datum within 1.5 interquartile range. Individual data points are shown for each sample. Stars indicate two-sided t-test values for each group compared with pNeuro− Neuro− patients (n = 5-16 patients in each group). ns, not significant (p > 0.05); * p < 5e-2, **p < 1e-2; ***p < 1e-3; ****p < 1e-4. k–m, Fold changes for (k) EMILIN3, (l) C4A, and (m) VGF across Tau and Oligo groups. Legend is same as (g-j). Stars indicate two-sided t-test values for each group compared with Tau− Oligo− and Tau− Oligo+ patients (n = 8-14 patients in each group). ns, not significant (p > 0.05); * p < 5e-2, **p < 1e-2; ***p < 1e-3; ****p < 1e-4.
Extended Data Fig. 10 Additional ROC and PMI analyses.
a,b, ROC curves predicting AD status from (a) protein and (b) phosphosites highlighted in Fig. 5f–h.
Supplementary information
Supplementary Information
Supplementary Note 1, Table 1 and Fig. 1.
Supplementary Data 1
Demographic information and clinical histopathology measurements for individual patients.
Supplementary Data 2
Full peptidome dataset with individual quantification values.
Supplementary Data 3
Peptide cluster composition: cluster identities and centroid values for peptides quantified in all samples.
Supplementary Data 4
Proteome and phosphoproteome cluster correlations: the table includes the Spearman’s correlation and associated P values between each peptide and each cluster centroid.
Supplementary Data 5
Proteome and phosphoproteome cluster fold-changes: the table includes fold-changes and P values for each peptide and cluster group against their respective negative cases.
Supplementary Data 6
AD mouse phosphoproteome overlap: AD mouse model phosphosites from Morshed et al.22 that had homologous phosphosites detected in the human AD phosphoproteome.
Supplementary Data 7
Peptide scores and VIP values for peptide-centric PLSR models: the table includes tabs for PLSR models built from pTyr, pSer/pThr, protein and all data.
Rights and permissions
About this article
Cite this article
Morshed, N., Lee, M.J., Rodriguez, F.H. et al. Quantitative phosphoproteomics uncovers dysregulated kinase networks in Alzheimer’s disease. Nat Aging 1, 550–565 (2021). https://doi.org/10.1038/s43587-021-00071-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s43587-021-00071-1
This article is cited by
-
Death-associated protein kinase 1 as a therapeutic target for Alzheimer's disease
Translational Neurodegeneration (2024)
-
A nonhuman primate model with Alzheimer’s disease-like pathology induced by hippocampal overexpression of human tau
Alzheimer's Research & Therapy (2024)
-
Plasma extracellular vesicles reveal early molecular differences in amyloid positive patients with early-onset mild cognitive impairment
Journal of Nanobiotechnology (2023)
-
Enhanced activity of Alzheimer disease-associated variant of protein kinase Cα drives cognitive decline in a mouse model
Nature Communications (2022)
-
Transcriptome-based analysis of blood samples reveals elevation of DNA damage response, neutrophil degranulation, cancer and neurodegenerative pathways in Plasmodium falciparum patients
Malaria Journal (2021)