Abstract
Loss of fertility is a major concern for female reproductive-age cancer survivors, since a common side-effect of conventional cytotoxic cancer therapies is permanent damage to the ovary. While immunotherapies are increasingly becoming a standard of care for many cancers—including in the curative setting—their impacts on ovarian function and fertility are unknown. We evaluated the effect of immune checkpoint inhibitors blocking programmed cell death protein ligand 1 and cytotoxic T lymphocyte-associated antigen 4 on the ovary using tumor-bearing and tumor-free mouse models. We find that immune checkpoint inhibition increases immune cell infiltration and tumor necrosis factor-α expression within the ovary, diminishes the ovarian follicular reserve and impairs the ability of oocytes to mature and ovulate. These data demonstrate that immune checkpoint inhibitors have the potential to impair both immediate and future fertility, and studies in women should be prioritized. Additionally, fertility preservation should be strongly considered for women receiving these immunotherapies, and preventative strategies should be investigated in future studies.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
Previously published microarray data that were re-analyzed here are available under accession code GSE38666. Source data are provided with this paper. All other data supporting the findings of this study are available from the corresponding author on reasonable request.
References
Barr, R. D. Adolescents, young adults, and cancer—the international challenge. Cancer 117, 2245–2249 (2011).
Lambertini, M. et al. Fertility preservation and post-treatment pregnancies in post-pubertal cancer patients: ESMO Clinical Practice Guidelines. Ann. Oncol. 31, 1664–1678 (2020).
ESHRE Guideline Group on Female Fertility Preservation et al. ESHRE guideline: female fertility preservation. Hum. Reprod. Open 2020, hoaa052 (2020).
Zhang, H. & Chen, J. Current status and future directions of cancer immunotherapy. J Cancer 9, 1773–1781 (2018).
Alesi, L. R., Winship, A. L. & Hutt, K. J. Evaluating the impacts of emerging cancer therapies on ovarian function. Curr. Opin. Endo. Metab. Res. 18, 15–28 (2021).
Johnson, D. B., Chandra, S. & Sosman, J. A. Immune checkpoint inhibitor toxicity in 2018. JAMA 320, 1702–1703 (2018).
Postow, M. A., Sidlow, R. & Hellmann, M. D. Immune-related adverse events associated with immune checkpoint blockade. N. Engl. J. Med. 378, 158–168 (2018).
Vaddepally, R. K., Kharel, P., Pandey, R., Garje, R. & Chandra, A. B. Review of indications of FDA-approved immune checkpoint inhibitors per NCCN guidelines with the level of evidence. Cancers (Basel) 12, 738 (2020).
Franasiak, J. M. & Scott, R. T. in Cancer & Fertility (ed. Sabanegh, J.E.S.) Ch. 2 (Springer International Publishing, 2016).
Cui, W. et al. Assessment of ovarian function in phase 3 (neo)adjuvant breast cancer clinical trials: a systematic evaluation. J. Natl Cancer Inst. 113, 1770–1778 (2021).
Kerr, J. B., Myers, M. & Anderson, R. A. The dynamics of the primordial follicle reserve. Reproduction 146, R205–R215 (2013).
Kerr, J. B. et al. The primordial follicle reserve is not renewed after chemical or γ-irradiation mediated depletion. Reproduction 143, 469–476 (2012).
Dunlop, C. E. & Anderson, R. A. The regulation and assessment of follicular growth. Scand. J. Clin. Lab. Invest. 74, 13–17 (2014).
Gilchrist, R. B., Ritter, L. J. & Armstrong, D. T. Mouse oocyte mitogenic activity is developmentally coordinated throughout folliculogenesis and meiotic maturation. Dev. Biol. 240, 289–298 (2001).
Chaffin, C. L. & Van de Voort, C. A. Follicle growth, ovulation, and luteal formation in primates and rodents: a comparative perspective. Exp. Biol. Med. 238, 539–548 (2013).
Gougeon, A. Dynamics of follicular growth in the human: a model from preliminary results. Hum. Reprod. 1, 81–87 (1986).
Bertolin, K. & Murphy, B. D. in The Guide to Investigation of Mouse Pregnancy (eds Croy, B. A. et al.) Ch. 7 (Academic Press, 2014).
Coxworth, J. E. & Hawkes, K. Ovarian follicle loss in humans and mice: lessons from statistical model comparison. Hum. Reprod. 25, 1796–1805 (2010).
Wu, R., Van der Hoek, K. H., Ryan, N. K., Norman, R. J. & Robker, R. L. Macrophage contributions to ovarian function. Hum. Reprod. Update 10, 119–133 (2004).
Bukulmez, O. & Arici, A. Leukocytes in ovarian function. Hum. Reprod. Update 6, 1–15 (2000).
Best, C. L., Pudney, J., Welch, W. R., Burger, N. & Hill, J. A. Localization and characterization of white blood cell populations within the human ovary throughout the menstrual cycle and menopause. Hum. Reprod. 11, 790–797 (1996).
Komatsu, K., Manabe, N., Kiso, M., Shimabe, M. & Miyamoto, H. Changes in localization of immune cells and cytokines in corpora lutea during luteolysis in murine ovaries. J. Exp. Zool. A Comp. Exp. Biol. 296A, 152–159 (2003).
Takaya, R. et al. Macrophages in normal cycling human ovaries; immunohistochemical localization and characterization. Hum. Reprod. 12, 1508–1512 (1997).
Cui, L. L., Yang, G., Pan, J. & Zhang, C. Tumor necrosis factor α knockout increases fertility of mice. Theriogenology 75, 867–876 (2011).
Lliberos, C., Liew, S. H., Mansell, A. & Hutt, K. J. The inflammasome contributes to depletion of the ovarian reserve during aging in mice. Front. Cell Dev. Biol. 8, 628473 (2020).
Lliberos, C. et al. Evaluation of inflammation and follicle depletion during ovarian ageing in mice. Sci. Rep. 11, 278 (2021).
Yamakami, L. Y. et al. Ovarian reserve in women with primary antiphospholipid syndrome. Lupus 23, 862–867 (2014).
Mont’Alverne, A. R. et al. Reduced ovarian reserve in patients with Takayasu arteritis. J. Rheumatol. 41, 2055–2059 (2014).
Mont’Alverne, A. R. et al. Diminished ovarian reserve in Behcet’s disease patients. Clin. Rheumatol. 34, 179–183 (2015).
Lawrenz, B. et al. Impact of systemic lupus erythematosus on ovarian reserve in premenopausal women: evaluation by using anti-Müllerian hormone. Lupus 20, 1193–1197 (2011).
Cui, L. et al. Chronic pelvic inflammation diminished ovarian reserve as indicated by serum anti Müllerian hormone. PLoS ONE 11, e0156130 (2016).
Winship, A. L., Stringer, J. M., Liew, S. H. & Hutt, K. J. The importance of DNA repair for maintaining oocyte quality in response to anti-cancer treatments, environmental toxins and maternal ageing. Hum. Reprod. Update 24, 119–134 (2018).
Stringer, J. M., Winship, A., Liew, S. H. & Hutt, K. The capacity of oocytes for DNA repair. Cell. Mol. Life Sci. 75, 2777–2792 (2018).
Steinert, E. M. et al. Quantifying memory CD8 T cells reveals regionalization of immunosurveillance. Cell 161, 737–749 (2015).
Kumar, B. V. et al. Human tissue-resident memory T cells are defined by core transcriptional and functional signatures in lymphoid and mucosal sites. Cell Rep. 20, 2921–2934 (2017).
Johnson, J. et al. Expression and T cell regulatory action of the PD-1 immune checkpoint in the ovary and fallopian tube. Preprint at bioRxiv https://doi.org/10.1101/2020.06.06.138123 (2020).
Hailemichael, Y. et al. Cancer vaccine formulation dictates synergy with CTLA-4 and PD-L1 checkpoint blockade therapy. J. Clin. Invest. 128, 1338–1354 (2018).
Jost, P. J. et al. XIAP discriminates between type I and type II FAS-induced apoptosis. Nature 460, 1035–1039 (2009).
Scaffidi, C. et al. Two CD95 (APO-1/Fas) signaling pathways. EMBO J. 17, 1675–1687 (1998).
Schug, Z. T., Gonzalvez, F., Houtkooper, R. H., Vaz, F. M. & Gottlieb, E. BID is cleaved by caspase-8 within a native complex on the mitochondrial membrane. Cell Death Differ. 18, 538–548 (2011).
Strasser, A., Jost, P. J. & Nagata, S. The many roles of FAS receptor signaling in the immune system. Immunity 30, 180–192 (2009).
Dhodapkar, K. M. Role of tissue-resident memory in intra-tumor heterogeneity and response to immune checkpoint blockade. Front. Immunol. 9, 1655 (2018).
Park, S. L. & Mackay, L. K. Decoding tissue-residency: programming and potential of frontline memory T cells. Cold Spring Harb. Perspect. Biol. 13, a037960 (2021).
Mackay, L. K. et al. Long-lived epithelial immunity by tissue-resident memory T (TRM) cells in the absence of persisting local antigen presentation. Proc. Natl Acad. Sci. USA 109, 7037–7042 (2012).
Sasson, S. C. et al. Interferon-gamma–producing CD8+ tissue resident memory T cells are a targetable hallmark of immune checkpoint inhibitor–colitis. Gastroenterology 161, 1229–1244.e1229 (2021).
Ebrahimi, M. & Akbari Asbagh, F. The role of autoimmunity in premature ovarian failure. Iran. J. Reprod. Med. 13, 461–472 (2015).
Matsuda-Minehata, F., Inoue, N., Goto, Y. & Manabe, N. The regulation of ovarian granulosa cell death by pro- and anti-apoptotic molecules. J. Reprod. Dev. 52, 695–705 (2006).
Yamamoto, Y. et al. Tumor necrosis factor alpha inhibits ovulation and induces granulosa cell death in rat ovaries. Reprod. Med. Biol. 14, 107–115 (2015).
Sasson, R., Winder, N., Kees, S. & Amsterdam, A. Induction of apoptosis in granulosa cells by TNFα and its attenuation by glucocorticoids involve modulation of Bcl-2. Biochem. Biophys. Res. Commun. 294, 51–59 (2002).
Quirk, S. M., Porter, D. A., Huber, S. C. & Cowan, R. G. Potentiation of Fas-mediated apoptosis of murine granulosa cells by interferon-γ, tumor necrosis factor-α, and cycloheximide. Endocrinology 139, 4860–4869 (1998).
Lee, H. J. et al. Induction of Fas-mediated apoptosis by interferon-γ is dependent on granulosa cell differentiation and follicular maturation in the rat ovary. Dev. Reprod. 20, 315–329 (2016).
Morrison, L. J. & Marcinkiewicz, J. L. Tumor necrosis factor α enhances oocyte/follicle apoptosis in the neonatal rat ovary. Biol. Reprod. 66, 450–457 (2002).
Michot, J. M. et al. Immune-related adverse events with immune checkpoint blockade: a comprehensive review. Eur. J. Cancer 54, 139–148 (2016).
Letourneau, J. M. et al. Pretreatment fertility counseling and fertility preservation improve quality of life in reproductive age women with cancer. Cancer 118, 1710–1717 (2012).
Ruddy, K. J. & Partridge, A. H. The unique reproductive concerns of young women with breast cancer. Adv. Exp. Med. Biol. 732, 77–87 (2012).
Faubion, S. S., Kuhle, C. L., Shuster, L. T. & Rocca, W. A. Long-term health consequences of premature or early menopause and considerations for management. Climacteric 18, 483–491 (2015).
Mittendorf, E. A. et al. Neoadjuvant atezolizumab in combination with sequential nab-paclitaxel and anthracycline-based chemotherapy versus placebo and chemotherapy in patients with early-stage triple-negative breast cancer (IMpassion031): a randomised, double-blind, phase 3 trial. Lancet 396, 1090–1100 (2020).
Schmid, P. et al. Pembrolizumab for early triple-negative breast cancer. N. Engl. J. Med. 382, 810–821 (2020).
Stewart, T. J. & Abrams, S. I. Altered immune function during long-term host-tumor interactions can be modulated to retard autochthonous neoplastic growth. J. Immunol. 179, 2851–2859 (2007).
Kaufmann, T. et al. The BH3-only protein bid is dispensable for DNA damage- and replicative stress-induced apoptosis or cell-cycle arrest. Cell 129, 423–433 (2007).
Byers, S. L., Wiles, M. V., Dunn, S. L. & Taft, R. A. Mouse estrous cycle identification tool and images. PLoS ONE 7, e35538 (2012).
Cora, M. C., Kooistra, L. & Travlos, G. Vaginal cytology of the laboratory rat and mouse: review and criteria for the staging of the estrous cycle using stained vaginal smears. Toxicol. Pathol. 43, 776–793 (2015).
Jin, S. Y., Lei, L., Shikanov, A., Shea, L. D. & Woodruff, T. K. A novel two-step strategy for in vitro culture of early-stage ovarian follicles in the mouse. Fertil. Steril. 93, 2633–2639 (2010).
Winship, A. L., Sarma, U. C., Alesi, L. R. & Hutt, K. J. Accurate follicle enumeration in adult mouse ovaries. J. Vis. Exp. https://doi.org/10.3791/61782 (2020).
Sarma, U. C., Winship, A. L. & Hutt, K. J. Comparison of methods for quantifying primordial follicles in the mouse ovary. J. Ovarian Res. 13, 121 (2020).
Molania, R., Gagnon-Bartsch, J. A., Dobrovic, A. & Speed, T. P. A new normalization for Nanostring nCounter gene expression data. Nucleic Acids Res. 47, 6073–6083 (2019).
Acknowledgements
The authors acknowledge the technical support of the Monash Animal Research Platform, Monash Histology Platform, Monash FlowCore Platform, Monash Micro Imaging Facility, Peter MacCallum Cancer Centre Animal Research Platform and Peter MacCallum Cancer Centres Flow Facility. We thank P. Bouillet and WEHI Bioservices for the provision of large numbers of BID-deficient mice. We also thank H. Thorne, E. Niedermayr, all the kConFab research nurses and staff, the heads and staff of the Family Cancer Clinics, the National Breast Cancer Foundation of Australia (NBCF), Cancer Australia and the National Institutes of Health (USA) for their contributions to this resource, and the many families who contribute to kConFab. Fig. 6h and the Supplementary Fig. 1 were created using BioRender.com. This work was made possible through Victorian State Government Operational Infrastructure Support and the Australian Government National Health and Medical Research Council (NHMRC) IRIISS. This work was supported by NBCF funding grant no. IIRS-22-092. A.L.W. is supported by DECRA funding grant no. DE21010037 from the Australian Research Council (ARC). L.R.A. is supported by an Australian Government Research Training Program Scholarship and a Monash Graduate Excellence Scholarship. K.-A.P. is an NHMRC Leadership Fellow. S.L. is supported by the NBCF. A.S. is supported by an NHMRC Program Grant no. 1113133, NHMRC Fellowship no. 1116937 and NHMRC Investigator Grant no. 2007887. K.J.H. is supported by an ARC Future Fellowship grant no. FT190100265.
Author information
Authors and Affiliations
Contributions
A.L.W. and K.J.H. conceived and designed the study. A.L.W., L.R.A., S.S., A.C., J.M.S., C.L.R., S.H.L., P.Z., E.B., S.B.F., U.S., M.J.G., T.H. and N.Z. performed experiments. L.R.A., A.L.W., A.C., P.Z., K.J.H., S.S., S.L., K.-A.P. and F.C. analyzed and interpreted the data. S.S., P.Z., S.L., N.L.G. and A.S. contributed materials and reagents. A.L.W., L.R.A. and K.J.H. wrote the manuscript. All authors edited the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Cancer thanks Michael Dougan, Matteo Lambertini, and Kunle Odunsi for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Flow cytometry gating strategy for tumor-bearing mice.
Gating strategy used to identify ovarian immune cell populations of tumor-bearing mice 4 d after the following final immunotherapy treatment.
Extended Data Fig. 2 Immune checkpoint molecules are expressed in both mouse and human ovary.
CD69 and PD-1 expression in the ovary of healthy WT non-tumor bearing mice was assessed by flow cytometry. (A) The proportions of ovarian CD69+CD4+ and CD69+CD8+ of total effector memory T cells and (B) PD-1+CD4+ and PD-1+CD8+ T cells were quantified in healthy, tumor-free WT mice (n = 3 animals/group). Data are presented as mean ± s.e.m. (C) Log2 expression of PDCD1, CD8A, CD3D, CD274 and CTLA4 in normal human ovary epithelia from n = 12 women and ovarian cancer epithelia from n = 18 women. Data are presented as mean (centre) ± s.e.m. (bounds) of box plots and minima and maxima of whiskers; two-tailed unpaired t-test. (D) Representative immunohistochemical localisation of (i) CD4+ T cells, (ii) CD8+ T cells, (iii) PD-1 and (iv) PD-L1 in human ovarian cortex from n = 4 healthy pre-menopausal women. Arrows indicate ovarian follicles, bars=50 μm.
Extended Data Fig. 3 Ovarian and splenic immune cell numbers in tumor-free mice, 21 days post-final treatment, and flow cytometry gating strategy.
Numbers of ovarian (A) CD4+ T cells, (B) CD8+ T cells and (C) macrophages; and splenic immune cells, including (D) CD4+ T cells, (E) CD8+ T cells and (F) macrophages were analysed by flow cytometry in mice 21 d after the final indicated treatment. Data are presented as mean ± s.e.m.; n = 5 animals/group. (G) Gating strategy used to identify mouse ovarian and splenic immune cell populations 24 h or 21 d following immunotherapy treatment.
Extended Data Fig. 4 Estrous cycling is disrupted in immune checkpoint inhibitor-treated tumor-free mice.
Estrous cycling was monitored by vaginal cytology for a 14-day period following the final indicated treatment in the 21 d cohort of animals administered with 10 mg/kg anti-PD-L1, anti-CTLA-4 or control antibody (IgG). Plots depict the estrous cycles of each individual animal. Vertical axes represent the phase of estrous cycle (P, proestrus; E, estrus; M, metestrus; D, diestrus). Red highlights disrupted phases of the cycle in some anti-PD-L1 or anti-CTLA4 animals; n = 5 animals/group.
Extended Data Fig. 5 Ovarian follicles and ovulation are disrupted even with lower-dose immune checkpoint inhibitor treatment.
Adult female C57BL6/J mice received 5 mg/kg anti-PD-L1, anti-CTLA-4 or control antibody (IgG) on d 1, 4 and 7. Ovaries were collected either 24 h or 14 d later (n = 6/group). At both time points, total numbers of (A) primordial, transitional and primary follicles; Kruskal-Wallis test: *p = 0.0453; one-way ANOVA: ***p = 0.0008, (B) secondary and antral follicles, **p = 0.001, ****p < 0.0001, **p = 0.0017, *p = 0.0204, *p = 0.0429 and (C) corpora lutea were quantified; one-way ANOVA: *p = 0.0454; Kruskal-Wallis test: *p = 0.0353. All data are presented as mean ± s.e.m.
Extended Data Fig. 6 Primordial follicles remain significantly depleted 100 days post-treatment, even after local ovarian cytokine production has returned to control levels.
Adult female C57BL6/J mice received 10 mg/kg anti-PD-L1, anti-CTLA-4 or control antibody (IgG) on d 1, 4 and 7. Ovaries were collected 100 d later (n = 6 animals/group). Total numbers of (A) primordial follicles were quantified. (B) Cytokine mRNA levels in the ovary 100 d after the final indicated treatment were analysed by RT-qPCR (IgG n = 5, anti-PD-L1 n = 4, anti-CTLA-4 n = 6 animals). Data are presented as mean ± s.e.m.; one-way ANOVA; **p = 0.0039, ***p = 0.0003.
Extended Data Fig. 7 Ovarian and splenic immune cell numbers in tumor-free mice, 24 hours post-final treatment.
Numbers of ovarian (A) CD4+ T cells, (B) CD8+ T cells and (C) macrophages; and splenic immune cells, including (D) CD4+ T cells, (E) CD8+ T cells and (F) macrophages were analysed by flow cytometry in mice 24 h after the final indicated treatment. Data are presented as mean ± s.e.m.; one-way ANOVA; *p < 0.05; n = 5 animals/group.
Extended Data Fig. 8 Estrous cycling is not disrupted following immune checkpoint blockade in Bid-/- mice.
(A) Estrous cycling was monitored by vaginal cytology for a 15-day period following the final indicated treatment in the 21-day cohort of Bid-/- animals that had been administered with 10 mg/kg anti-PD-L1 (n = 4) or control antibody (n = 5). Plots depict the estrous cycles of each individual animal. Vertical axes represent the phase of estrous cycle (P, proestrus; E, estrus; M, metestrus; D, diestrus). (B) Compilation of primordial follicle numbers from wild-type and genetic knockout mouse models.
Supplementary information
Supplementary Figure 1
Graphical Abstract
Supplementary Tables
Supplementary Tables 1–3.
Source data
Source Data Fig. 1
Numerical data.
Source Data Fig. 2
Numerical data.
Source Data Fig. 3
Numerical data.
Source Data Fig. 4
Numerical data.
Source Data Fig. 5
Numerical data.
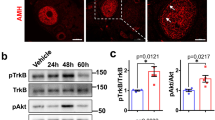
Source Data Fig. 5
Unprocessed western blots.
Source Data Fig. 6
Numerical data.
Source Data Extended Data Fig. 2
Numerical data.
Source Data Extended Data Fig. 3
Numerical data.
Source Data Extended Data Fig. 4
Numerical data.
Source Data Extended Data Fig. 5
Numerical data.
Source Data Extended Data Fig. 6
Numerical data.
Source Data Extended Data Fig. 7
Numerical data.
Source Data Extended Data Fig. 8
Numerical data.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Winship, A.L., Alesi, L.R., Sant, S. et al. Checkpoint inhibitor immunotherapy diminishes oocyte number and quality in mice. Nat Cancer 3, 1–13 (2022). https://doi.org/10.1038/s43018-022-00413-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s43018-022-00413-x
This article is cited by
-
A life-course approach to tackling noncommunicable diseases in women
Nature Medicine (2024)
-
Clinical and translational attributes of immune-related adverse events
Nature Cancer (2024)
-
Effects of Cetrorelix on Ovary and Endometrium Prior to Anti-PD-L1 Antibody in Murine Model
Tissue Engineering and Regenerative Medicine (2024)
-
Immunotherapy in Early-Stage Triple-Negative Breast Cancer: Where Are We Now and Where Are We Headed?
Current Treatment Options in Oncology (2023)
-
Fertilität, Kontrazeption und Teratogenität bei Immuncheckpointblockade
Die Dermatologie (2023)