Abstract
Small cell lung cancer (SCLC) is notorious for its early and frequent metastases, which contribute to it as a recalcitrant malignancy. To understand the molecular mechanisms underlying SCLC metastasis, we generated SCLC mouse models with orthotopically transplanted genome-edited lung organoids and performed multiomics analyses. We found that a deficiency of KMT2C, a histone H3 lysine 4 methyltransferase frequently mutated in extensive-stage SCLC, promoted multiple-organ metastases in mice. Metastatic and KMT2C-deficient SCLC displayed both histone and DNA hypomethylation. Mechanistically, KMT2C directly regulated the expression of DNMT3A, a de novo DNA methyltransferase, through histone methylation. Forced DNMT3A expression restrained metastasis of KMT2C-deficient SCLC through repressing metastasis-promoting MEIS/HOX genes. Further, S-(5′-adenosyl)-l-methionine, the common cofactor of histone and DNA methyltransferases, inhibited SCLC metastasis. Thus, our study revealed a concerted epigenetic reprogramming of KMT2C- and DNMT3A-mediated histone and DNA hypomethylation underlying SCLC metastasis, which suggested a potential epigenetic therapeutic vulnerability.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
Data availability
The RNA-seq, ATAC-seq, CUT&Tag, WGBS and scRNA-seq data in this study are deposited in the NCBI Gene Expression Omnibus under accession number GSE161570. The processed files for omics analysis were submitted to the Figshare database (https://figshare.com/articles/dataset/A_Coherent_Histone_and_DNA_Hypomethylation_Reprogramming_Drives_Small_Cell_Lung_Cancer_Metastasis/13206338). The SCLC genomics data were downloaded from cBioPortal (https://www.cbioportal.org/). The omics data of 39 SCLC cell lines were accessed from the CCLE database of the depmap portal (https://depmap.org/portal), including the mutation, CpG methylation, RNA-seq and annotation information. The RNA-seq data and clinical data of 81 individuals with SCLC were downloaded from ref. 21. The RNA-seq data of 86 individuals with SCLC were downloaded from ref. 47. The RNA-seq data of 120 SCLC CDX samples were downloaded from ref. 48 (https://doi.org/10.5281/zenodo.3574846). The scRNA-seq data of individuals with SCLC were downloaded from ref. 20. Source data are provided with this paper. All other data supporting the findings of this study are available from the corresponding author on reasonable request.
Code availability
The analysis code can be found at GitHub (https://github.com/pangxueyu233/KMT2C-in-SCLC-Metastasis).
References
Valastyan, S. & Weinberg, R. A. Tumor metastasis: molecular insights and evolving paradigms. Cell 147, 275–292 (2011).
Hu, Z., Li, Z., Ma, Z. & Curtis, C. Multi-cancer analysis of clonality and the timing of systemic spread in paired primary tumors and metastases. Nat. Genet. 52, 701–708 (2020).
Reiter, J. G. et al. Minimal functional driver gene heterogeneity among untreated metastases. Science 361, 1033–1037 (2018).
Makohon-Moore, A. P. et al. Limited heterogeneity of known driver gene mutations among the metastases of individual patients with pancreatic cancer. Nat. Genet. 49, 358–366 (2017).
Ramaswamy, S., Ross, K. N., Lander, E. S. & Golub, T. R. A molecular signature of metastasis in primary solid tumors. Nat. Genet. 33, 49–54 (2003).
van ‘t Veer, L. J. et al. Gene expression profiling predicts clinical outcome of breast cancer. Nature 415, 530–536 (2002).
McDonald, O. G. et al. Epigenomic reprogramming during pancreatic cancer progression links anabolic glucose metabolism to distant metastasis. Nat. Genet. 49, 367–376 (2017).
Gazdar, A. F., Bunn, P. A. & Minna, J. D. Small-cell lung cancer: what we know, what we need to know and the path forward. Nat. Rev. Cancer 17, 725–737 (2017).
Matthews, M. J., Kanhouwa, S., Pickren, J. & Robinette, D. Frequency of residual and metastatic tumor in patients undergoing curative surgical resection for lung cancer. Cancer Chemother. Rep. 3 4, 63–67 (1973).
H.R.733—Recalcitrant Cancer Research Act of 2012 (US Congress, 2012); https://www.congress.gov/bill/112th-congress/house-bill/733
Augustyn, A. et al. ASCL1 is a lineage oncogene providing therapeutic targets for high-grade neuroendocrine lung cancers. Proc. Natl Acad. Sci. USA 111, 14788–14793 (2014).
Osborne, J. K. et al. NeuroD1 regulates survival and migration of neuroendocrine lung carcinomas via signaling molecules TrkB and NCAM. Proc. Natl Acad. Sci. USA 110, 6524–6529 (2013).
Semenova, E. A. et al. Transcription factor NFIB is a driver of small cell lung cancer progression in mice and marks metastatic disease in patients. Cell Rep. 16, 631–643 (2016).
Denny, S. K. et al. NFIB promotes metastasis through a widespread increase in chromatin accessibility. Cell 166, 328–342 (2016).
Yang, D. et al. Intertumoral heterogeneity in SCLC is influenced by the cell type of origin. Cancer Discov. 8, 1316–1331 (2018).
Meuwissen, R. et al. Induction of small cell lung cancer by somatic inactivation of both Trp53 and Rb1 in a conditional mouse model. Cancer Cell 4, 181–189 (2003).
Schaffer, B. E. et al. Loss of p130 accelerates tumor development in a mouse model for human small-cell lung carcinoma. Cancer Res. 70, 3877–3883 (2010).
Rudin, C. M. et al. Molecular subtypes of small cell lung cancer: a synthesis of human and mouse model data. Nat. Rev. Cancer 19, 289–297 (2019).
Ghandi, M. et al. Next-generation characterization of the Cancer Cell Line Encyclopedia. Nature 569, 503–508 (2019).
Stewart, C. A. et al. Single-cell analyses reveal increased intratumoral heterogeneity after the onset of therapy resistance in small-cell lung cancer. Nat. Cancer 1, 423–436 (2020).
George, J. et al. Comprehensive genomic profiles of small cell lung cancer. Nature 524, 47–53 (2015).
Chen, C. et al. MLL3 is a haploinsufficient 7q tumor suppressor in acute myeloid leukemia. Cancer Cell 25, 652–665 (2014).
Hodgkinson, C. L. et al. Tumorigenicity and genetic profiling of circulating tumor cells in small-cell lung cancer. Nat. Med. 20, 897–903 (2014).
Yang, D. et al. Axon-like protrusions promote small cell lung cancer migration and metastasis. eLife 8, e50616 (2019).
Zhang, Z. M. et al. Structural basis for DNMT3A-mediated de novo DNA methylation. Nature 554, 387–391 (2018).
Jia, D., Jurkowska, R. Z., Zhang, X., Jeltsch, A. & Cheng, X. Structure of Dnmt3a bound to Dnmt3L suggests a model for de novo DNA methylation. Nature 449, 248–251 (2007).
Gao, Q. et al. Deletion of the de novo DNA methyltransferase Dnmt3a promotes lung tumor progression. Proc. Natl Acad. Sci. USA 108, 18061–18066 (2011).
Mayle, A. et al. Dnmt3a loss predisposes murine hematopoietic stem cells to malignant transformation. Blood 125, 629–638 (2015).
Kandoth, C. et al. Mutational landscape and significance across 12 major cancer types. Nature 502, 333–339 (2013).
Alam, H. et al. KMT2D deficiency impairs super-enhancers to confer a glycolytic vulnerability in lung cancer. Cancer Cell 37, 599–617 (2020).
Shilatifard, A. The COMPASS family of histone H3K4 methylases: mechanisms of regulation in development and disease pathogenesis. Annu. Rev. Biochem. 81, 65–95 (2012).
Paco, A., Aparecida de Bessa Garcia, S., Leitao Castro, J., Costa-Pinto, A. R. & Freitas, R. Roles of the HOX proteins in cancer invasion and metastasis. Cancers 13, 10 (2020).
Tiberio, C. et al. HOX gene expression in human small-cell lung cancers xenografted into nude mice. Int. J. Cancer 58, 608–615 (1994).
Roe, J. S. et al. Enhancer reprogramming promotes pancreatic cancer metastasis. Cell 170, 875–888 (2017).
Hanahan, D. Hallmarks of cancer: new dimensions. Cancer Discov. 12, 31–46 (2022).
Rudin, C. M., Brambilla, E., Faivre-Finn, C. & Sage, J. Small-cell lung cancer. Nat. Rev. Dis. Primers 7, 3 (2021).
Drapkin, B. J. & Rudin, C. M. Advances in small-cell lung cancer (SCLC) translational research. Cold Spring Harb. Perspect. Med. 11, a038240 (2020).
Chatterjee, A., Rodger, E. J. & Eccles, M. R. Epigenetic drivers of tumourigenesis and cancer metastasis. Semin. Cancer Biol. 51, 149–159 (2018).
Fares, J., Fares, M. Y., Khachfe, H. H., Salhab, H. A. & Fares, Y. Molecular principles of metastasis: a hallmark of cancer revisited. Signal Transduct. Target. Ther. 5, 28 (2020).
Gardner, E. E. et al. Chemosensitive relapse in small cell lung cancer proceeds through an EZH2–SLFN11 axis. Cancer Cell 31, 286–299 (2017).
Mohammad, H. P. et al. A DNA hypomethylation signature predicts antitumor activity of LSD1 inhibitors in SCLC. Cancer Cell 28, 57–69 (2015).
Wu, B. et al. Epigenetic drug library screening identified an LSD1 inhibitor to target UTX-deficient cells for differentiation therapy. Signal Transduct. Target. Ther. 4, 11 (2019).
Drost, J. et al. Organoid culture systems for prostate epithelial and cancer tissue. Nat. Protoc. 11, 347–358 (2016).
Chen, C. et al. Cancer-associated IDH2 mutants drive an acute myeloid leukemia that is susceptible to Brd4 inhibition. Genes Dev. 27, 1974–1985 (2013).
Buenrostro, J. D., Giresi, P. G., Zaba, L. C., Chang, H. Y. & Greenleaf, W. J. Transposition of native chromatin for fast and sensitive epigenomic profiling of open chromatin, DNA-binding proteins and nucleosome position. Nat. Methods 10, 1213–1218 (2013).
Chen, M. et al. An epigenetic mechanism underlying chromosome 17p deletion-driven tumorigenesis. Cancer Discov. 11, 194–207 (2021).
Jiang, L. et al. Genomic landscape survey identifies SRSF1 as a key oncodriver in small cell lung cancer. PLoS Genet. 12, e1005895 (2016).
Simpson, K. L. et al. A biobank of small cell lung cancer CDX models elucidates inter- and intratumoral phenotypic heterogeneity. Nat. Cancer 1, 437–451 (2020).
Acknowledgements
We thank Ruizhan Tong and the members of the C.C.–L.Y. laboratory for their technical support and suggestions and the Core Facilities of West China Hospital. This work was supported by the National Key R&D Program of China (2017YFA0505600, C.C.), the National Natural Science Foundation of China (81522003, 82170171, 81770157 and 81570150, C.C.; 81570150, F.N.; 8210102196, J.C.), the Sichuan Science and Technology Program (2020YFQ0059, 2020ZYD002, 2018JZ0077 and 2017TJPT0005, C.C.) and the 1.3.5. Project for Disciplines of Excellence, West China Hospital, Sichuan University (C.C.).
Author information
Authors and Affiliations
Contributions
F.N., X.P., J.C. and X.C. designed and performed experiments, analyzed data and wrote the manuscript. M.W., P.C., L.Y., L. Zhang, A.Z., L. Zhao, S.D., M. Zhang, Yiyun Wang, B.W., J. Zheng, Yuying Wang, J. Xu, J.W., B.W., M.C., H.L., J. Xue, M.H., Y.G., J. Zhu, L. Zhou, Y. Zhang, M.Y., P.T., M.F. and Z.L. performed experiments and analyzed data. Z.X., Y. Zhao, H.Y., C.Z., Yuan Wang, J.H., S.Y., D.X., L.C., Q.Z., M. Zeng, S.W.L., Y. Lu, Y. Liu and Y. Wei provided resources and designed experiments. C.C. conceived the project, designed experiments, analyzed data and wrote the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Cancer thanks the anonymous reviewers for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Generating primary and orthotopic SCLC with metastases with genome edited lung organoids in mice.
(a) Representative bright-field and fluorescent images of lung organoids transduced with V2TC-sgRNAs and Myc. Three independent repeats. Scale bar, 200 μm. (b) T7 endonuclease 1 (T7E1) assays on Rb1 or Trp53 using infected lung organoid. Cleaved bands were pointed by arrowheads. Three independent repeats. (c) Representative IHC staining of KI67 of lung sections of the PRM mice (n = 4 mice). Scale bar, 20 µm. (d) Representative bright-field and fluorescent images showing metastatic lesions in the lymph nodes of the PRM mice (n = 4 mice). Scale bar, 2 mm. (e) Representative H&E staining of the lymph nodes (n = 4 mice). Scale bar, 20 µm. (f) Representative TTF1 staining of the lymph nodes (n = 4 mice). Scale bar, 20 µm. (g) Representative pictures showing staining of ASCL1, CHGA, SYP and NEUROD1 of liver sections of the PRM mice (n = 4 mice). Scale bar, 40 µm. (h) Representative pictures showing staining of ASCL1, CHGA, SYP and NEUROD1 of the PRM mice’s lymph node (n = 4 mice). Scale bar, 40 µm.
Extended Data Fig. 2 Single-cell transcriptome analyses of primary and metastatic SCLC cells.
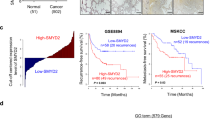
(a) The ATAC-Seq plot showing signals at the TSS of the PRM and PRM-Met SCLC cells. (b) The bar graph showing the numbers of differential chromatin accessible peaks in the PRM and PRM-Met tumor cells. (c) Genome-wide distribution of chromatin open peaks (left) and close peaks (right) in PRM-Met compared to PRM, measured by ATAC-seq analyses. (d) The dot plot showing the marker genes of each cell type. (e) The openTSNE maps showing the expression distributions of Chga, Ddc and Ncam1. (f) The Alluvial plot showing the composition variation of cell populations in PRM and PRM-Met. (g) The URD map showing the CDX metastasis score projected on the metastasis trajectory. (h) The Kaplan-Meier survival curves of SCLC patients with low and high mouse metastatic scores. p-value was calculated by log-rank test (n = 61, low; n = 16, high). (i) The dynamically expressed genes and enriched gene signatures on the metastasis trajectory. (j) The Kaplan-Meier survival curves of SCLC patients with low and high Module I gene signatures. p-value was calculated by log-rank test (n = 7, low; n = 70, high).
Extended Data Fig. 3 KMT2C deficiency in SCLC metastases and its function in lung organoids.
(a) The Venn plot showing the mutation frequency of epigenetic regulatory genes in Module I. (b) The Ridge plot showing gene ontology enrichment in the Ascl1 + primary SCLC cells, analyzed by GSEA. (c) The Kaplan-Meier survival curves of SCLC patients with low and high expressions of KMT2C. Calculated by log-rank test. (n = 42, low; n = 35, high) (d) Representative western blotting pictures of H3K4me1 and H3K4me2 in the PRM and PRM-Met SCLC cells. Three independent repeats. (e) Representative staining of KMT2C, H3K4me1and H3K4me2 of the PRM primary (n = 3) (left) and PRM-Met (n = 3) liver sections (right). Scale bar, 40 µm. (f) The levels of H3K4me1 bound at the enhancers in the PRM and PRM-Met tumor cells, measured by the CUT&Tag analyses. (g) Genome-wide distribution of the H3K4me1 up-regulated genes (top) and down-regulated genes (bottom) in PRM-Met compared to PRM, measured by CUT&Tag analyses. (h) T7 endonuclease 1 (T7E1) assays showing the mutations of Kmt2c in the premalignant PRM organoids. Three independent repeats. Cleaved bands were pointed by arrowheads. (i) Dynamics of relative expression levels of Cyp2f2, Notch1 and Mki67 on the normal development (black line) and malignant transformation (purple line) trajectories.
Extended Data Fig. 4 Pathological analysis of the metastases in the PRM and PRMK mice.
(a) Representative H&E (left) and TTF1 staining (right) of the lung sections of the PRMK mice (n = 4 mice). Scale bar, 200 µm. (b) Representative staining of ASCL1, CHGA, NEUROD1 and SYP of the lung (top) and liver (bottom) sections of the PRMK mice (n = 4 mice). Scale bar, 20 µm. (c) Representative images of the lymph nodes (left) and kidney (right) of the PRM (n = 4) (top) and PRMK (n = 4) (bottom) mice. Scale bar, 2 mm. (d) Representative H&E (top) and TTF1 staining (bottom) of the PRM (n = 4) and PRMK (n = 4) mice’s lymph nodes (left) and kidney (right) sections. Scale bar, 200 µm. (e) The -∆∆CT value of SCLC marker genes Ascl1, Ncam1, Chga and Syp in the CTC of PRM mice, measured by RT-qPCR (n = 3 technical replicates). (f) The -∆∆CT value of SCLC marker genes Ascl1, Ncam1, Chga and Syp in the CTC of PRMK mice, measured by RT-qPCR (n = 3 technical replicates).
Extended Data Fig. 5 The histone methylation in the PRM and PRMK SCLC.
(a) Representative staining of KMT2C, H3K4me1 and H3K4me2 of the lung sections of PRM (n = 3 mice) (top) and PRMK (n = 3 mice) (bottom). Scale bar, 40 µm. (b) Representative western blotting pictures showing the H3k4me1, H3k4me2, H3K4me3, H3K9me3, H3K27me3, H3K27ac and H3K36me3 levels in the PRM and PRMK SCLC cells. Three independent repeats. (c) The IGV plots showing the mutations and expression levels of Kmt2c in the PRM and PRMK SCLC.
Extended Data Fig. 6 The epigenetic reprogramming in SCLC with Kmt2c loss.
(a) The levels of H3K4me1 bound at the enhancer (left) and TSS (right) in the PRM and PRMK SCLC cells, measured by CUT&Tag analyses. (b) Genome-wide distribution of the H3K4me1 up-regulated genes (left) and down-regulated genes (right) in PRMK compared to PRM, measured by CUT&Tag analyses. (c) The levels of H3K4me2 bound at the TSS in the PRM and PRMK SCLC cells, measured by CUT&Tag analyses. (d) Genome-wide distribution of the H3K4me2 up-regulated genes (left) and down-regulated genes (right) in PRMK compared to PRM, measured by CUT&Tag analyses. (e) The levels of H3K4me3 bound at the TSS in the PRM and PRMK SCLC cells, measured by CUT&Tag analyses. (f) Genome-wide distribution of the H3K4me3 up-regulated genes (left) and down-regulated genes (right) in PRMK compared to PRM, measured by CUT&Tag analyses. (g) The levels of ATAC bound at the TSS in the PRM and PRMK SCLC cells, measured by CUT&Tag analyses. (h) Genome-wide distribution of the ATAC open genes (top) and close genes (bottom) in PRMK compared to PRM. (i) The levels of KMT2C bound at the peaks of gene body in the PRM, PRM-Met and PRMK tumor cells, measured by the CUT& Tag analyses. (j) Genome-wide distribution of the KMT2C binding peaks in PRM, measured by CUT&Tag analyses.
Extended Data Fig. 7 The effect of epigenetic reprogramming on gene expressions in SCLC with Kmt2c loss.
(a) The Venn diagram showing overlapping of the H3K4me2 down-regulated genes and the KMT2C down-regulated genes in PRMK compared to the PRM SCLC cells. p-value was calculated by a hypergeometric test. (b) Heatmap showing the differential expressed genes in the PRM and PRMK organoids. (c) The Venn diagram showing overlapping of the chromatin close genes and those downregulated in the PRMK cells compared to the PRM cells. p-value was calculated by a hypergeometric test. (d) The Venn diagram showing overlapping of the down-regulated genes and those with reduced H3K4me1 in the PRMK compared to the PRM cells. p-value was calculated by a hypergeometric test. (e) The Venn diagram showing overlapping of the H3K4me1 up-regulated genes in the PRM metastasis cells compared to the PRM primary cells and the H3K4me1 up-regulated genes in the PRMK cells compared to the PRM primary. p-value was calculated by a hypergeometric test. (f) The Venn diagram showing overlapping of the chromatin open genes in the PRM metastasis cells compared to the PRM primary cells and the chromatin open genes in the PRMK cells compared to the PRM primary. p-value was calculated by a hypergeometric test. (g) The Venn diagram showing overlapping of the chromatin open genes and those upregulated in the PRMK cells compared to the PRM cells. p-value was calculated by a hypergeometric test. (h) GSEA showing positive enrichment of the PRMK up-regulated gene set in the metastasis SCLC, compared to primary tumor cells in the CCLE cohort.
Extended Data Fig. 8 Identifying DNMT3A as a downstream target of KMT2C in SCLC.
(a) The Venn diagram showing overlapping of the down-regulated genes in RNA expression, chromatin accessibility, H3K4me1 in PRM-Met compared to PRM. p-value was calculated by a hypergeometric test. (b) The scatter plot showing the correlation between the relative expression levels of KMT2C and DNMT3A in multiple SCLC cohorts. (c) The Kaplan-Meier survival curves of SCLC patients with high or low expressions of DNMT3A. (n = 55, low; n = 22, high).
Extended Data Fig. 9 KMT2C loss gave rise to DNA hypomethylation in SCLC.
(a) The density plot showing all C sites’ methylation levels in the genome of the PRM and PRMK SCLC cells. (b) The 5mC levels of the CpG regions in the PRM and PRMK cells. (c) The density plot showing all C sites’ methylation levels in the genome of the PRM and PRM-Met SCLC cells. (d) The density plot showing the methylation levels of the CpG regions in the CCLE primary and metastasis SCLC cells. (e) The density plot showing the methylation levels of the CpG regions in the CCLE SCLC cells with or without KMT2C mutations. (f) The scatter plot showing the differentially methylated regions (DMRs) in the PRM and PRMK SCLC cells. (g) The scatter plot showing the differentially methylated sites (DMS) in the KMT2C-WT and KMT2C-Mut CCLE SCLC samples. (h) Pie charts showed the genomics region annotation (top) and CpGs subtypes (bottom) of hyper- and hypo- DMRs in PRMK compared to PRM. (i) The Venn diagram showed overlapping of the hypomethylated genes and open genes in PRMK compared to PRM (left); p-value was calculated by a hypergeometric test. The box plot displayed the normalized expression levels of 171 overlap genes of hypomethylated genes and open genes in PRM and PRMK (right), The box bounds the interquartile range divided by the median, with the whiskers extending to a maximum of 1.5 times the interquartile range beyond the box. p-value was calculated by Wilcoxon signed-rank test. (j) Dot blotting showed the expression of 5mC in PRMK organoids with vector or DNMT3A overexpression (left). The statistics of DNA 5mC levels in PRMK cells (right). (mean ± SEM, n = 3). Calculated by Student’s t-test, two-sided. All p-value, *, p < 0.05.
Extended Data Fig. 10 SAM treatment for KMT2C deficient SCLC.
(a) The dot blotting (left) and the relative levels (right) of 5mC in the PRMK organoids treated with vehicle or SAM. (mean ± SD, n = 3). *, p < 0.05, Calculated by Student’s t-test, two-sided. (b) The representative western blotting pictures showing the H3k4me1 and H3k4me2 levels in the PRMK organoids treated with vehicle or SAM. Three independent repeats. (c) The representative flow cytometry plots of CTCs in the peripheral blood of PRMK mice treated with vehicle or SAM. (d) Heatmap showing the differential pathways in SAM treated PRMK SCLC cells compared to those treated with vehicle, measured by RNA-seq analyses.
Supplementary information
Supplementary Information
Supplementary Fig. 1.
Supplementary Tables
Supplementary Tables 1–29.
Source data
Source Data Fig. 2
Statistical source data.
Source Data Fig. 3
Statistical source data.
Source Data Fig. 4
Statistical source data.
Source Data Fig. 6
Statistical source data.
Source Data Fig. 6
Unprocessed dot blots.
Source Data Fig. 7
Statistical source data.
Source Data Fig. 8
Statistical source data.
Source Data Extended Data Fig. 1
Unprocessed gels.
Source Data Extended Data Fig. 3
Unprocessed data.
Source Data Extended Data Fig. 4
Statistical source data.
Source Data Extended Data Fig. 5
Unprocessed western blots.
Source Data Extended Data Fig. 9
Statistical source data.
Source Data Extended Data Fig. 9
Unprocessed dot blots.
Source Data Extended Data Fig. 10
Statistical source data.
Source Data Extended Data Fig. 10
Unprocessed blots.
Rights and permissions
About this article
Cite this article
Na, F., Pan, X., Chen, J. et al. KMT2C deficiency promotes small cell lung cancer metastasis through DNMT3A-mediated epigenetic reprogramming. Nat Cancer 3, 753–767 (2022). https://doi.org/10.1038/s43018-022-00361-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s43018-022-00361-6
This article is cited by
-
Small cells – big issues: biological implications and preclinical advancements in small cell lung cancer
Molecular Cancer (2024)
-
Genetically-engineered mouse models of small cell lung cancer: the next generation
Oncogene (2024)
-
Establishment of a small-cell lung cancer (SCLC) mouse model using enhanced cancer stem-cell-functioning 3D SCLC spheroids
Molecular & Cellular Toxicology (2024)
-
Oncogenic enhancers prime quiescent metastatic cells to escape NK immune surveillance by eliciting transcriptional memory
Nature Communications (2024)
-
Applications of lung cancer organoids in precision medicine: from bench to bedside
Cell Communication and Signaling (2023)