Despite substantial advances in understanding of the molecular features of gliomas, the therapeutic options for these aggressive tumors remain scarce. Rich, Mitchell and colleagues provide their views about a phase 1 clinical trial testing the safety and efficacy of vaccines against cancer expressing mutant metabolic enzyme IDH1 in patients with high-grade glioma.
From the bench: Sameer Agnihotri and Jeremy N. Rich
Gliomas are the most prevalent primary brain tumors and remain incurable despite extensive molecular characterization and research aimed at identifying viable therapeutic vulnerabilities. Among the various glioma subtypes, diffuse gliomas and secondary glioblastomas are driven mostly by gain-of-function oncogenic mutations in genes encoding the metabolic enzymes IDH1 and, less frequently, IDH2, and thus are genetically distinct from primary glioblastomas1,2. Mutations in IDH1 are commonly found in heterozygosis and often result in the single-amino-acid substitution of arginine (R) with histidine (H) in the catalytic site of IDH1 at codon 132 (called ‘IDH1(R132H)’ here)1,2,3. Mutations in IDH1 and IDH2 result in neomorphic enzymatic activities that lead to production of the oncometabolite 2-HG4,5,6. 2-HG inhibits the enzymatic functions of many α-ketoglutarate-dependent enzymes, including histone and DNA demethlyases, and thus causes the aberrant epigenetic reprogramming seen in the CpG island methylator phenotypes7,8,9,10,11. The presence of mutations in IDH1 and/or IDH2 have led to intensive preclinical and clinical research aimed at developing clinical-grade inhibitors of mutant IDH1, some of which have achieved approval from the US Food and Drug Administration for certain indications, including acute myeloid leukemia or cholangiocarcinoma expressing mutant IDH1; however, despite promising preclinical evidence in support of the efficacy of these compounds, clinical studies of these mutant IDH1–targeted compounds for glioma have not yet progressed beyond early-phase clinical trials, mostly due to concerns about their ability to overcome the blood–brain barrier. This leaves few targeted therapeutic opportunities for patients with glioblastoma, and thus there is an urgent unmet need for the development of alternative strategies that could provide a suitable path for the treatment of these aggressive tumors.
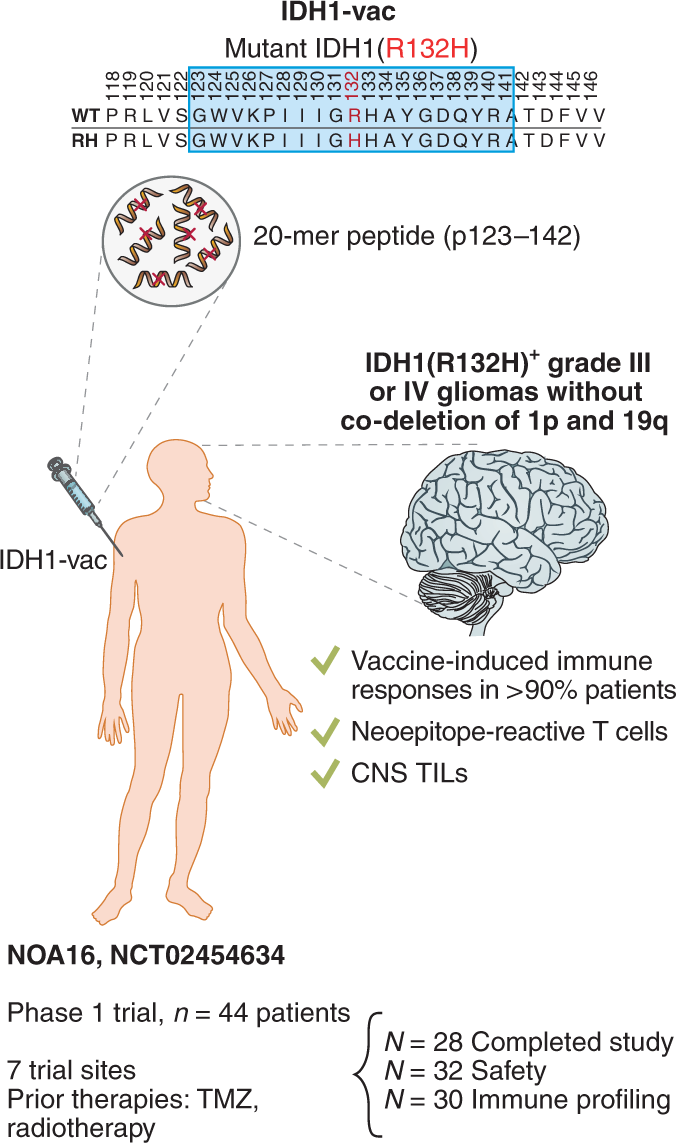
Writing in Nature, Platten and colleagues now report the results of a phase 1 trial testing an anti-cancer vaccine designed to target neoantigens commonly found in patients with glioma bearing IDH1 mutations12 (Fig. 1). Their results provide proof-of-concept evidence of the feasibility and efficacy of this immunotherapy modality and open the path for the development of similar therapeutic approaches for the treatment of these lethal tumors.
A 20-amino-acid (20-mer) peptide that spans codons 123–142 of mutant IDH1 (p123–142)—and thus contains the neoepitope generated by the R132H mutation present in this subset of patients with grade III or IV glioma—was selected for the development of an IDH1-vac anti-cancer vaccine. The cohort included 44 patients from seven different trial sites, who were selected for assessment of safety and efficacy after exposure to IDH1-vac. 1p and 19q, chromosomal arms; CNS, central nervous system; TILs, tumor-infiltrating lymphocytes; TMZ, temozolomide.
Anti-cancer vaccination typically consists of the administration of tumor-specific antigens that elicit adaptive anti-tumor immune responses. These antigens usually comprise ‘self’ peptides or ‘non-self’ peptides (such as cancer testis antigens or human papillomavirus proteins, respectively), although the best responses to anti-cancer vaccines are usually achieved when these are directed against antigens expressed exclusively by tumor cells. This has led to greater interest in the use of specific antigens that arise from endogenous tumor mutational processes and are generally known as ‘neoantigens’ or ‘neoepitopes’. Even though anti-cancer vaccines have been extensively explored in various settings with relative success, they have achieved uneven activity in neuro-oncology. More than 70% of diffuse gliomas harbor the IDH1 R132H mutation, an early genetic lesion expressed nearly uniformly by tumor cells, which renders this a potentially powerful therapeutic candidate. Additionally, this neoepitope is presented via the class II major histocompatibility complex (MHC)13 and thus represents an attractive potential target for immunotherapy.
Previous preclinical studies demonstrated that versions of an IDH1(R132H)-specific peptide vaccine (IDH1-vac) were capable of inducing sustained anti-tumor–specific therapeutic helper T cell responses in syngeneic MHC-humanized mice13. Platten and colleagues developed an array of peptides encompassing the R132H substitution within IDH1 and identified the peptide p123–142, which spans the codons 123–142 and includes the R132H substitution, as a potent inducer of specific anti-tumor immune responses to cells expressing mutant IDH1 (Fig. 1). On the basis of this promising preclinical evidence, Platten and colleagues designed a multi-center, phase 1 clinical trial (NOA-16; ClinicalTrials.gov identifier NCT02454634) to test the safety, feasibility and efficacy of a vaccine targeting mutant IDH1 in newly diagnosed patients with World Health Organization (WHO) grade III or grade IV glioma12 (Fig. 1).
In this proof-of-concept trial, Platten and colleagues demonstrated that the IDH1-targeting vaccine was safe and immunogenic and was capable of inducing both T cell and B cell immune responses across patients bearing a variety of human leukocyte antigen–encoding alleles. The authors established a mutation-specificity score to incorporate the duration and level of IDH1-vac-induced T cell immune responses and observed that patients with high scores showed predominant production of the cytokines TNF, IFN-γ and IL-17 by helper T cells, indicative of involvement of the TH1 and TH17 subtypes of helper T cells. The authors also followed up with the patients and assessed the 3-year progression-free and death-free rates, which were 0.63 and 0.84, respectively. Interestingly, treated patients displayed higher rates of pseudoprogression (PsPD), a condition in which patients develop mass lesions that resemble tumor growth by neuroimaging, than those of a molecularly matched cohort that had not been treated with the IDH1-targeting vaccine. PsPD indicates intratumoral inflammatory infiltration and reactions, with prior studies suggesting that patients who develop PsPD after conventional therapy may survive longer. PsPD after vaccination did not correlate with patient age, extent of resection, standard-of-care treatment, or tumor grade. Furthermore, PsPD did not correlate with specific copy-number variations, tumor-methylation class (e.g., the CpG island methylator phenotype), or deletion status for CDKN2A (which encodes a cyclin-dependent kinase inhibitor).
Overall, these results provide evidence that supports the proposal of the induction of specific anti-tumor immune responses after vaccination with a cancer-specific neoepitope.
From the clinic: Kailin Yang and Duane A. Mitchell
Of the 44 patients initially enrolled in the clinical trial, 32 met the inclusion criteria and received the vaccine; the authors were able to perform analysis on the safety and feasibility of this therapy on all the treated patients, including mid-term follow-up, and were also able to perform immunological profiling in a subset of 30 of these treated patients (Fig. 1).
In order to generate a comprehensive map of the complex immunological interactions taking place in the tumor microenvironment following administration of the neoantigen vaccine, the authors performed single-cell RNA sequencing of tumor samples from patients; this allowed them to delineate the heterogeneity of the immune-cell landscape, which eventually resulted in the identification of three distinct clusters of CD4+ T cells within PsPD masses, such as CXCL13+CD4+ T cells, which are key to sustaining anti-tumor immunity responses. Moreover, sequencing of T cell antigen receptors in patients with PsPD revealed that tumor-infiltrating helper T cell clusters displayed a predominance of a single T cell antigen receptor clone, which suggested that IDH1-vac induced the clonal expansion of mutant IDH1–specific helper T cells.
There are notable observations that arise at the interface of the clinical findings and immunological findings of this study that have substantial implications in support of further vaccine development for IDH1-mutant gliomas specifically and for glioma immunotherapy more generally. For example, the observation of vaccine-induced immune responses in more than 90% of the vaccinated participants spanning a broad repertoire of MHC-encoding alleles provides compelling proof-of-concept evidence of the induction of T cell immunity to a highly conserved and ubiquitously expressed glioma-specific mutant protein. Notably, the higher than expected frequency of PsPD in vaccinated participants (and, in a single case, tumor tissue after vaccination) demonstrates an increased frequency of mutant IDH1–specific T cells among tumor-infiltrating lymphocytes.
Despite the promising data in support of the proposal of mutant IDH1 neoepitope–reactive T cells that localize to the central nervous system, further confirmatory studies linking vaccine responses to radiographic and immunological changes are needed. Future prospective studies that incorporate specific imaging endpoints as well as systematic analyses of tumor tissues and/or cerebral spinal fluid will help answer important questions about the potential for imaging modalities to detect changes within gliomas after vaccination; the possibility of monitoring the activity of mutant IDH1–stimulated T cells through liquid biopsy of cerebrospinal fluid; and whether CD4+ T cells that recognize mutant IDH1 effectively elicit anti-tumor activity that translates into improved patient outcomes, or if other populations are involved and required in establishment of the long-term anti-tumor immune responses.
Among the limitations of the study, the trial was not sufficiently powered to determine the relationship between vaccination and patient outcomes, as expected from a phase 1 study; moreover, the overall survival and progression-free survival times for patients with IDH1-mutant gliomas would be expected to be prolonged within this subgroup of patients with glioma. The investigators observed a trend of higher mutation-specificity scores in patients with PsPD than in patients with progressive disease or stable disease, as well as indications of better vaccine-induced responses in patients with stable disease than in those with progressive disease. However, randomized and appropriately powered clinical trials will be needed to determine the long-term impact of this approach, and to discern whether specific immunological correlates can serve as biomarkers of clinical responses. The authors had previously demonstrated that patients have spontaneous T cell and antibody responses to mutant IDH1, and thus it would be very interesting to know whether baseline responses to the mutant protein influence vaccine responses, PsPD and clinical outcomes.
Although the results of this study are encouraging and provide a foundation for further development, some additional outstanding questions remain. For example, during follow-up, four of ten patients with methylation-class high-grade glioma experienced progressive disease. Moreover, PsPD was not detected in patients who did not respond to treatment. Although no molecular correlates were found in this study, it would be interesting to see if future studies can identify patients who will not respond or patients at greater risk of developing progressive disease. Future and larger clinical trials may additionally provide more-granular insights into the various subtypes and stages of this disease by looking at grade III gliomas and grade IV gliomas as distinct entities. As gliomas are highly heterogeneous and develop subclonal alterations during the course of the disease, this vaccine may also provide superior therapeutic indices in combination with other immunotherapy approaches, such as immune-checkpoint inhibition14. As 2-HG has been shown to impair T cell function, small-molecule inhibitors of mutant IDH1 may augment the anti-tumor efficacy of vaccines against mutant IDH115.
As mutant IDH1 is a clonal event, and its expression is detected almost universally in all tumor cells, the vaccine against IDH1 provides the basis of a potentially impactful therapeutic strategy. From a wider point of view, this study—along with the recent scientific advancements in vaccine technology—may provide the foundation for the exploration of vaccine-based therapies for other incurable cancers following a similar rationale, and the work by Platten and colleagues provides the proof-of-concept clinical evidence that will undoubtedly stimulate the development of similarly impactful therapeutic strategies.
References
The Cancer Genome Atlas Research Network. N. Engl. J. Med. 372, 2481–2498 (2015).
Parsons, D. W. et al. Science 321, 1807–1812 (2008).
Yan, H. et al. N. Engl. J. Med. 360, 765–773 (2009).
Andronesi, O. C. et al. J. Clin. Invest. 123, 3659–3663 (2013).
Dang, L. et al. Nature 465, 966 (2010).
Pusch, S. et al. Acta Neuropathol. Commun. 2, 19 (2014).
Lu, C. et al. Nature 483, 474–478 (2012).
Noushmehr, H. et al. Cancer Cell 17, 510–522 (2010).
Rohle, D. et al. Science 340, 626–630 (2013).
Sasaki, M. et al. Nature 488, 656–659 (2012).
Xu, W. et al. Cancer Cell 19, 17–30 (2011).
Platten, M. et al. Nature 592, 463–468 (2021).
Schumacher, T. et al. Nature 512, 324–327 (2014).
Touat, M. et al. Nature 580, 517–523 (2020).
Bunse, L. et al. Nat. Med. 24, 1192–1203 (2018).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Rights and permissions
About this article
Cite this article
Agnihotri, S., Yang, K., Mitchell, D.A. et al. A vaccine for glioma. Nat Cancer 2, 584–586 (2021). https://doi.org/10.1038/s43018-021-00228-2
Published:
Issue Date:
DOI: https://doi.org/10.1038/s43018-021-00228-2