Abstract
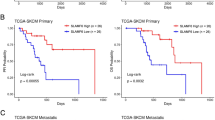
Primary melanomas >1 mm thickness are potentially curable by resection, but can recur metastatically. We assessed the prognostic value of the T-cell fraction (TCFr) and repertoire T-cell clonality, measured by high-throughput sequencing of the T-cell receptor β-chain in T2–T4 primary melanomas (n = 199). TCFr accurately predicted progression-free survival and was independent of thickness, ulceration, mitotic rate and age. TCFr was second only to tumor thickness in its predictive value, using a gradient-boosted model. For accurate progression-free survival prediction, adding TCFr to tumor thickness was superior to adding any other histopathological variable. Furthermore, a TCFr >20% was protective regardless of tumor ulceration status, mitotic rate or presence of nodal disease. TCFr is a quantitative molecular assessment that predicts metastatic recurrence in primary melanoma patients whose disease has been resected surgically. The present study suggests that a successful T-cell-mediated, antitumour response can be present in primary melanomas.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
Data availability
TCRB-sequencing data that support the findings of this study have been deposited at the publicly available immuneACCESS platform at https://clients.adaptivebiotech.com/pub/pruessmann-2019-nc and https://doi.org/10.21417/WP2019NC. Previously published data that were reanalyzed here can be found at https://clients.adaptivebiotech.com/pub/weber-2018-cir (https://doi.org/10.21417/EY2019CIR), and https://github.com/riazn/bms038_analysis. Imaging source data are available on request from the corresponding author. Numerical source data for Figs. 3c, 7a–d and 8 are presented with the paper. All other data supporting the findings of the present study are available from the corresponding author upon reasonable request.
Code availability
All code was performed using R v.3.5.1 and publicly available packages. Cox’s regressions were performed using the survival package v.2.43. Plots were generated using ggplot2 v.3.2.0. Heatmaps of V-family and J-gene usage were generated using the LymphoSeq package (https://doi.org/10.18129/B9.bioc.LymphoSeq) v.3.10. No custom packages were written for the analysis. Code underlying the analysis is available upon request from the corresponding author.
Change history
17 March 2020
A Correction to this paper has been published: https://doi.org/10.1038/s43018-020-0049-z
References
Matthews, N. H., Li, W. Q., Qureshi, A. A., Weinstock, M. A. & Cho, E. Epidemiology of melanoma. in Cutaneous Melanoma: Etiology and Therapy (eds., Ward, W. H. & Farma, J. M.) Chapter 1 (Codon Publications, 2017).
Shaikh, W. R. et al. Melanoma thickness and survival trends in the United States, 1989 to 2009. J. Natl Cancer Inst. 108, djv294 (2016).
Gershenwald, J. E. et al. Melanoma staging: evidence-based changes in the American Joint Committee on Cancer eighth edition cancer staging manual. CA Cancer J. Clin. 67, 472–492 (2017).
Elsaesser, O. et al. Prognosis of sentinel node staged patients with primary cutaneous melanoma. PLoS ONE 7, e29791 (2012).
Lawrence, M. S. et al. Mutational heterogeneity in cancer and the search for new cancer-associated genes. Nature 499, 214–218 (2013).
Hayward, N. K. et al. Whole-genome landscapes of major melanoma subtypes. Nature 545, 175–180 (2017).
Snyder, A. et al. Genetic basis for clinical response to CTLA-4 blockade in melanoma. N. Engl. J. Med. 371, 2189–2199 (2014).
Clemente, C. G. et al. Prognostic value of tumor infiltrating lymphocytes in the vertical growth phase of primary cutaneous melanoma. Cancer 77, 1303–1310 (1996).
Clark, W. H. Jr. et al. Model predicting survival in stage I melanoma based on tumor progression. J. Natl Cancer Inst. 81, 1893–1904 (1989).
Azimi, F. et al. Tumor-infiltrating lymphocyte grade is an independent predictor of sentinel lymph node status and survival in patients with cutaneous melanoma. J. Clin. Oncol. 30, 2678–2683 (2012).
Mansson-Brahme, E. et al. Prognostic factors in thin cutaneous malignant melanoma. Cancer 73, 2324–2332 (1994).
Tuthill, R. J., Unger, J. M., Liu, P. Y., Flaherty, L. E. & Sondak, V. K. Risk assessment in localized primary cutaneous melanoma: a Southwest Oncology Group study evaluating nine factors and a test of the Clark logistic regression prediction model. Am. J. Clin. Pathol. 118, 504–511 (2002).
van Houdt, I. S. et al. Favorable outcome in clinically stage II melanoma patients is associated with the presence of activated tumor infiltrating T-lymphocytes and preserved MHC class I antigen expression. Int. J. Cancer 123, 609–615 (2008).
Krynitz, B., Rozell, B. L., Lyth, J., Smedby, K. E. & Lindelof, B. Cutaneous malignant melanoma in the Swedish organ transplantation cohort: a study of clinicopathological characteristics and mortality. J. Am. Acad. Dermatol. 73, 106–113 e102 (2015).
Thomas, N. E. et al. Tumor-infiltrating lymphocyte grade in primary melanomas is independently associated with melanoma-specific survival in the population-based genes, environment and melanoma study. J. Clin. Oncol. 31, 4252–4259 (2013).
Burton, A. L. et al. Prognostic significance of tumor infiltrating lymphocytes in melanoma. Am. Surg. 77, 188–192 (2011).
Kruper, L. L. et al. Predicting sentinel node status in AJCC stage I/II primary cutaneous melanoma. Cancer 107, 2436–2445 (2006).
Taylor, R. C., Patel, A., Panageas, K. S., Busam, K. J. & Brady, M. S. Tumor-infiltrating lymphocytes predict sentinel lymph node positivity in patients with cutaneous melanoma. J. Clin. Oncol. 25, 869–875 (2007).
Mandala, M. et al. Clinical and histopathological risk factors to predict sentinel lymph node positivity, disease-free and overall survival in clinical stages I–II AJCC skin melanoma: outcome analysis from a single-institution prospectively collected database. Eur. J. Cancer 45, 2537–2545 (2009).
Donizy, P. et al. Paucity of tumor-infiltrating lymphocytes is an unfavorable prognosticator and predicts lymph node metastases in cutaneous melanoma patients. Anticancer Res. 35, 351–358 (2015).
Thorn, M., Ponten, F., Bergstrom, R., Sparen, P. & Adami, H. O. Clinical and histopathologic predictors of survival in patients with malignant melanoma: a population-based study in Sweden. J. Natl Cancer Inst. 86, 761–769 (1994).
Barnhill, R. L., Fine, J. A., Roush, G. C. & Berwick, M. Predicting five-year outcome for patients with cutaneous melanoma in a population-based study. Cancer 78, 427–432 (1996).
Saldanha, G., Flatman, K., Teo, K. W. & Bamford, M. A novel numerical scoring system for melanoma tumor-infiltrating lymphocytes has better prognostic value than standard scoring. Am. J. Surg. Pathol. 41, 906–914 (2017).
Larkin, J. et al. Combined nivolumab and ipilimumab or monotherapy in untreated melanoma. N. Engl. J. Med. 373, 23–34 (2015).
Prieto, P. A. et al. CTLA-4 blockade with ipilimumab: long-term follow-up of 177 patients with metastatic melanoma. Clin. Cancer Res. 18, 2039–2047 (2012).
Hogan, S. A., Levesque, M. P. & Cheng, P. F. Melanoma immunotherapy: next-generation biomarkers. Front. Oncol. 8, 178 (2018).
Robert, L. et al. Distinct immunological mechanisms of CTLA-4 and PD-1 blockade revealed by analyzing TCR usage in blood lymphocytes. Oncoimmunology 3, e29244 (2014).
Postow, M. A. et al. Peripheral T cell receptor diversity is associated with clinical outcomes following ipilimumab treatment in metastatic melanoma. J. Immunother. Cancer 3, 23 (2015).
Cha, E. et al. Improved survival with T cell clonotype stability after anti-CTLA-4 treatment in cancer patients. Sci. Transl. Med. 6, 238ra270 (2014).
Tumeh, P. C. et al. PD-1 blockade induces responses by inhibiting adaptive immune resistance. Nature 515, 568–571 (2014).
Roh, W. et al. Integrated molecular analysis of tumor biopsies on sequential CTLA-4 and PD-1 blockade reveals markers of response and resistance. Sci. Transl. Med. 9, eaah3560 (2017).
Riaz, N. et al. Tumor and microenvironment evolution during immunotherapy with nivolumab. Cell 171, 934–949 e915 (2017).
Inoue, H. et al. Intratumoral expression levels of PD-L1, GZMA, and HLA-A along with oligoclonal T cell expansion associate with response to nivolumab in metastatic melanoma. Oncoimmunology 5, e1204507 (2016).
Yusko, E. et al. Association of tumor microenvironment T-cell repertoire and mutational load with clinical outcome after sequential checkpoint blockade in melanoma. Cancer Immunol. Res. 7, 458–465 (2019).
Elith, J., Leathwick, J. R. & Hastie, T. A working guide to boosted regression trees. J. Animal Ecol. 77, 802–813 (2008).
Simoni, Y. et al. Bystander CD8+ T cells are abundant and phenotypically distinct in human tumour infiltrates. Nature 557, 575–579 (2018).
Duhen, T. et al. Co-expression of CD39 and CD103 identifies tumor-reactive CD8 T cells in human solid tumors. Nat. Commun. 9, 2724 (2018).
Vasaturo, A. et al. T-cell landscape in a primary melanoma predicts the survival of patients with metastatic disease after their treatment with dendritic cell vaccines. Cancer Res. 76, 3496–3506 (2016).
Nsengimana, J. et al. beta-Catenin-mediated immune evasion pathway frequently operates in primary cutaneous melanomas. J. Clin. Invest. 128, 2048–2063 (2018).
Scheper, W. et al. Low and variable tumor reactivity of the intratumoral TCR repertoire in human cancers. Nat. Med. 25, 89–94 (2019).
Rosato, P. C. et al. Virus-specific memory T cells populate tumors and can be repurposed for tumor immunotherapy. Nat. Commun. 10, 567 (2019).
Camisaschi, C., Vallacchi, V., Castelli, C., Rivoltini, L. & Rodolfo, M. Immune cells in the melanoma microenvironment hold information for prediction of the risk of recurrence and response to treatment. Expert Rev. Mol. Diagn. 14, 643–646 (2014).
Ladanyi, A. et al. T-cell activation marker expression on tumor-infiltrating lymphocytes as prognostic factor in cutaneous malignant melanoma. Clin. Cancer Res. 10, 521–530 (2004).
Park, C. K. & Kim, S. K. Clinicopathological significance of intratumoral and peritumoral lymphocytes and lymphocyte score based on the histologic subtypes of cutaneous melanoma. Oncotarget 8, 14759–14769 (2017).
Huang, A. C. et al. A single dose of neoadjuvant PD-1 blockade predicts clinical outcomes in resectable melanoma. Nat. Med. 25, 454–461 (2019).
Carlson, C. S. et al. Using synthetic templates to design an unbiased multiplex PCR assay. Nat. Commun. 4, 2680 (2013).
Robins, H. S. et al. Comprehensive assessment of T-cell receptor beta-chain diversity in alphabeta T cells. Blood 114, 4099–4107 (2009).
R Core Team. R: A Language and Environment for Statistical Computing Version 3.4.3 (R Foundation for Statistical Computing, 2017).
McShane, L. M. et al. Reporting recommendations for tumor marker prognostic studies (REMARK). J. Natl Cancer Inst. 97, 1180–1184 (2005).
Acknowledgements
This work was supported by National Institutes of Health grant nos. R01 AI127654 (to T.S.K.) and R01 CA203721 (to R.A.C. and T.S.K.). W.P. was supported by a grant of the German Research Foundation (grant no. PR 1621/1-1), B.D.-A. received grant support from the Novo Nordisk Foundation and the Lundbeck Foundation. Laboratory services were provided at no cost by Adaptive Biotechnologies. We thank Dana-Farber/Harvard Cancer Center in Boston, MA, for the use of the Pathology Specimen Locator Core, which is supported in part by a National Cancer Institute Cancer Center support grant (no. NIH 5 P30 CA06516). We thank J. Lock Andersen for help providing clinical data related to the collected archival melanoma samples. Support from colleagues of the MIA and the Australian National Health and Medical Research Council is also gratefully acknowledged. J.S.W. and R.A.S. are supported by Australian National Health and Medical Research Council Fellowships. J.F.T. is supported by the Medical Foundation of the University of Sydney. G.A. is supported by a scholarship from the University of Sydney. immunoSEQ, immuneACCESS and their associated designs are trademarks of Adaptive Biotechnologies. Other trademarks are the property of their respective owners. immunoSEQ Assays are for research use only and not for use in diagnostic procedures.
Author information
Authors and Affiliations
Contributions
W.P. and T.S.K. searched the literature and designed the study, and performed the data analysis and interpretation. J.R. performed the statistical analysis, data analysis and interpretation of high-throughput sequencing. W.P., P.F., E.Y. and H.R. contributed to the high-throughput sequencing. J.W., B.D-A., J.F.T., P.M.F., K.K., R.A.C. and R.A.S. acquired the clinical samples and patient data, and provided clinical interpretation. W.P. and B.D-A. processed the samples and performed laboratory experiments. M.C.M. histologically reassessed the TIL infiltration. Q.Z. helped with immunofluorescence staining. G.H.A. performed the mIHC and multispectral image analysis. A.J.C and J.W. reviewed the mIHC and multispectral image analysis. J.R. and W.P. prepared the figures. W.P., J.R. and T.S.K. wrote the manuscript. All the co-authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
J.R., P.F., E.Y. and H.R. are or were employed by and have financial interest in Adaptive Biotechnologies. H.R. owns intellectual property associated with Adaptive Biotechnologies. T.S.K. serves on the Scientific Advisory Board (Hematology) of Adaptive Biotechnologies but does not own stock or receive compensation.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Effect of FFPE age on TCR sequencing.
(a) Data quality of immunosequenced FFPE samples by sample age; bin-width = 1 year. Samples with < 500 nucleated cells (orange) were considered to have insufficient cellularity and/or DNA degradation and were excluded from analysis. All samples with ≥ 500 nucleated cells were analyzed for T cell fraction (green and yellow); only samples with ≥ 500 nucleated cells and ≥ 100 T cells (green) were analyzed for Simpson’s clonality. (b) Fitted LOESS curve showing the fraction of analyzable samples (green and yellow samples from figure (a) by FFPE sample age.
Extended Data Fig. 2 Deletions and insertions during somatic TCRB recombination.
Frequency distribution of (a) sum of deletions (Vdels, D5dels, D3dels and Jdels) and (b) insertions (N1ins, N2ins). Progressors and Non-Progressors do not differ. Non-Progressors, n = 107 primary melanoma samples; Progressors, n = 92. For all box plots, the bold line indicates the median; box illustrates lower and upper quartiles; whiskers show the lowest and highest data point still within 1.5x of interquartile range from lower or upper quartile, respectively; dots are outliers.
Extended Data Fig. 3 TCRB-V-family and TCRB-J-gene usage in progressors versus non-progressors.
Non-clustered heatmaps illustrating the usage of TCRB-V-family (a) or TCRB-J-gene (b) generated with the R package LymphoSeq. Gene usage does not differ between progressors and non-progressors. NA = patients with unknown recurrence status.
Extended Data Fig. 4 Simpson’s clonality and associations between clinicopathological variables.
(a) Simpson’s clonality is comparable between all T stages. Kruskal-Wallis Test; 1-2 mm, n = 42 independent samples; 2-4 mm, n = 59; > 4 mm, n = 57. Box plots: bold line indicates the median; box illustrates lower and upper quartiles; whiskers show the lowest and highest data point still within 1.5x of interquartile range from lower or upper quartile, respectively; all dots are data points. (b) Simpson’s clonality is not correlated with Breslow thickness. Spearman’s correlation test; n = 158 primary melanoma samples. (c) Spearman’s Rho calculated for correlations between continuous variables; Spearman’s correlation test; n = 158 primary melanoma samples.
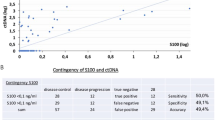
Extended Data Fig. 5 TCFr cut-off benchmarking and selection.
(a) Fraction below cut-off and (b) true negative rate (TNR: proportion of patients above the cut-off who remain disease-free) for seven different TCFr cut-off values as measured by bootstrapping the training group 100 times. Box plots (n = 100 bootstraps): the bold line indicates the median; box illustrates lower and upper quartiles; whiskers show the lowest and highest data point still within 1.5x of interquartile range from lower or upper quartile, respectively. Each dot represents one bootstrap per TCFr value. (c) Precision-Recall Curves of 100 training cohort bootstraps colorized by TCFr cut-off. (d) First order derivate of F-score versus TCFr cut-off colorized by the TPR; each dot represents one bootstrap per TCFr value, which were fitted with a LOESS curve.
Extended Data Fig. 6 Histological TIL grading.
TIL regrading of samples, using two histological grading systems (n = 153 primary melanoma samples). (a,b) Shown are T cell fraction per TIL grade for each thickness group. Dots for samples with low ( < 20%) TCFr are colorized orange, with high ( ≥ 20%) TCFr in green. Number of independent samples listed in plots. For all box plots: the bold line indicates the median; box illustrates lower and upper quartiles; whiskers show the lowest and highest data point still within 1.5x of interquartile range from lower or upper quartile, respectively; dots are data points. (c,d) Kaplan-Meier PFS curves according to (c) conventional TIL briskness assessment and (d) MIA TIL scores. Both grading systems are predictive of PFS; Cox regression with two-sided Z-test and Likelihood ratio test (LRT) (briskness: LRT p = 3E-5; MIA: LRT p = 0.001).
Extended Data Fig. 7 Composition of T cell infiltrate.
(a) Boxplot illustrating the higher median TCFr measured by TCRB sequencing in comparison to multiplex immunohistochemistry (mIHC), medianHTS = 0.21 vs medianmIHC = 0.05. Two-sided Wilcoxon Rank Sum Test; TCRseq, n = 199 primary melanoma patients; mIHC, n = 57. Box plots: the bold line indicates the median; box illustrates lower and upper quartiles; whiskers show the lowest and highest data point still within 1.5x of interquartile range from lower or upper quartile, respectively; dots are data points. (b) Overall, the TCFr determined by TCRB sequencing correlates with the fraction of CD3+/DAPI (all) cells by mIHC. Line = regression line, grey shading = 95% confidence interval, Spearman’s correlation test; n = 57 primary melanoma samples. (c) The percentage of CD3+ cells as well as of CD8+, CD4+, Tregs and tumor antigen specific CD8+ T cells (CD8+ CD39+ and CD8+ CD39+ CD103+) varies greatly if multiple (sequential) sections of one tumor are analyzed.
Extended Data Fig. 8 Power calculation.
Estimation of statistical power given 𝑥 number of subjects in a cohort and a range of effect sizes (i.e., hazard ratios), assuming a type I error rate of 5% and the typical variance observed for tumor T cell fractions.
Supplementary information
Supplementary Information
Supplementary Tables 1–5.
Source data
Source Data Fig. 3
Correlation statistics.
Source Data Fig. 7
Histological TIL grading data.
Source Data Fig. 8
Multiplex IHC data.
Rights and permissions
About this article
Cite this article
Pruessmann, W., Rytlewski, J., Wilmott, J. et al. Molecular analysis of primary melanoma T cells identifies patients at risk for metastatic recurrence. Nat Cancer 1, 197–209 (2020). https://doi.org/10.1038/s43018-019-0019-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s43018-019-0019-5
This article is cited by
-
Reversing immunosuppression in the tumor microenvironment of fibrolamellar carcinoma via PD-1 and IL-10 blockade
Scientific Reports (2024)
-
Evolution and modulation of antigen-specific T cell responses in melanoma patients
Nature Communications (2022)
-
Tumour gene expression signature in primary melanoma predicts long-term outcomes
Nature Communications (2021)