Abstract
Evidence on what people eat globally is limited in scope and rigour, especially as it relates to children and adolescents. This impairs target setting and investment in evidence-based actions to support healthy sustainable diets. Here we quantified global, regional and national dietary patterns among children and adults, by age group, sex, education and urbanicity, across 185 countries between 1990 and 2018, on the basis of data from the Global Dietary Database project. Our primary measure was the Alternative Healthy Eating Index, a validated score of diet quality; Dietary Approaches to Stop Hypertension and Mediterranean Diet Score patterns were secondarily assessed. Dietary quality is generally modest worldwide. In 2018, the mean global Alternative Healthy Eating Index score was 40.3, ranging from 0 (least healthy) to 100 (most healthy), with regional means ranging from 30.3 in Latin America and the Caribbean to 45.7 in South Asia. Scores among children versus adults were generally similar across regions, except in Central/Eastern Europe and Central Asia, high-income countries, and the Middle East and Northern Africa, where children had lower diet quality. Globally, diet quality scores were higher among women versus men, and more versus less educated individuals. Diet quality increased modestly between 1990 and 2018 globally and in all world regions except in South Asia and Sub-Saharan Africa, where it did not improve.
Similar content being viewed by others
Main
Poor diet is a leading cause of disease worldwide, responsible for an estimated 26% of global preventable mortality1,2,3,4. While individual foods and nutrients are important, overall dietary patterns are more strongly associated with health5. Evidence supports interactive and synergistic relationships between foods and nutrients when consumed together6, resulting in complementary effects5. While the various components of an optimal dietary pattern are well established and validated7, the distributions of such patterns globally are not well characterized. This is particularly true for children and adolescents, among whom global dietary patterns have not previously been reported.
Previous dietary studies have been limited to small subsets of countries8,9, used national per capita food availability or sales data as direct data inputs10,11,12,13,14, which substantially misestimate intake compared with individual-level data15 and did not include children, adolescents or young adults (<25 years old)8,9,10,11,12,16. Additionally, there is a paucity of evidence on global disparities in dietary patterns, for example by age, sex, education and urbanicity. Also, no previous global studies have jointly assessed several validated metrics of diet quality17, such as the Alternative Healthy Eating Index (AHEI), the Dietary Approaches to Stop Hypertension (DASH) and the Mediterranean Diet Score (MED).
In this Article, to address these gaps in knowledge, we characterized global, regional and national dietary patterns and trends on the basis of individual-level intake data among both adults and children from 185 countries in 1990 and 2018. Findings were further assessed by age, sex, education and urbanicity within each country. This analysis utilized the latest Global Dietary Database (GDD) 2018 data, based on individual-level dietary surveys around the world18.
Results
The GDD is a collaborative effort to systematically identify, compile and standardize individual-level dietary data on 53 foods, beverages and nutrients (Methods). The GDD uses Bayesian modelling methods to estimate dietary intakes jointly stratified by age, sex, education, level and urbanicity for 185 countries between 1990 and 2018.
Global and regional diet quality in 2018
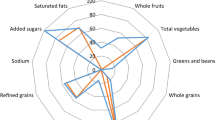
In 2018, the global mean of the AHEI score was 40.3 (95% uncertainty interval (UI) 39.4, 41.3), with regional means ranging from 30.3 (28.7, 32.2) in Latin America and the Caribbean to 45.7 (43.8, 49.3) in South Asia (Fig. 1). Among components of the score, highest global scores for healthier items were for legumes/nuts (5.0; 4.8, 5.3), followed by whole grains (4.7; 4.5, 5.0), seafood omega-3 fat (4.2; 3.8, 5.1) and non-starchy vegetables (3.9; 3.8, 4.0); among unhealthier items, highest scores (lowest or most favourable intakes) were for sugar-sweetened beverages (SSBs) (5.8; 5.7, 5.9) and red/processed meat (4.8; 4.5, 5.1). However, these score components varied substantially by world region. For example, top scores in South Asia were for higher whole grains and lower red/processed meat and SSBs, while top scores in Latin American and the Caribbean were for higher legumes/nuts and lower sodium.
National diet quality in 2018
Only ten countries, representing <1% of the world’s population, had AHEI scores ≥50. Among the world’s 25 most populous countries, the mean AHEI score was highest in Vietnam, Iran, Indonesia and India (54.5 to 48.2) and lowest in Brazil, Mexico, the United States and Egypt (27.1–33.5) (Fig. 2). Most component scores varied substantially across these populous countries. For example, a 100-fold difference was seen in the sodium score, a 90-fold difference in the red/processed meat score and a 23-fold difference in the SSB score. Among the components, the polyunsaturated fatty acid (PUFA) and non-starchy vegetable scores varied the least (two-fold and three-fold, respectively) across populous countries.
Global and regional differences across demographic subgroups
Globally, the mean AHEI score in 2018 was similar among children (39.2; 38.2, 40.3) versus adults (40.8; 39.8, 42.0) (Fig. 1). However, the mean AHEI score was substantially higher among adults compared with children in Central/Eastern Europe and Central Asia, high-income countries, and the Middle East and Northern Africa region. By age, most regions had J- or U-shaped relationships, with the highest scores observed among the youngest (≤5 years) and/or oldest age groups (≥75 years) (Fig. 3).
The AHEI score ranged from 0 to 100. The circles represent the global or regional mean for the age group, and the error bars represent the corresponding 95% UI. The mean and its UI are plotted for the midpoint of each age group (<1, 1–2, 3–4, 5–9, 10–14, 15–19, 20–24, 25–29, 30–34, 35–39, 40–44, 45–49, 50–54, 55–59, 60–64, 65–69, 70–74, 75–79, 80–84, 85–89, 90–94 and ≥95 years).
Among the AHEI components globally, four component scores were lower among children versus adults: fruit (2.2 (2.1, 2.3) versus 2.5 (2.4, 2.5), respectively), non-starchy vegetables (3.1 (3.0, 4.5) versus 4.3 (4.2, 3.2)), SSBs (5.3 (5.1, 5.5) versus 6.1 (6.0, 6.2)) and seafood omega-3 (3.3 (2.9, 4.0) versus 4.7 (4.2, 5.7)), while two others were higher among children versus adults: PUFAs (2.1 (2.0, 2.2) versus 1.4 (1.3, 1.5)) and sodium (4.6 (4.1, 5.1) versus 3.2 (2.9, 3.5)) (Fig. 1).
By sex, the mean AHEI score was generally higher in women versus men globally and regionally, with the greatest differences seen in high-income countries (difference +4.4; 3.8, 5.0), and Central/Eastern Europe and Central Asia (+3.6; 2.1, 5.3) (Extended Data Fig. 1). Evaluating different AHEI components globally, women had modestly higher scores for fruit (+0.2; 0.2, 0.3), non-starchy vegetables (+0.3; 0.1, 0.4) and whole grains (+0.4; 0.2, 0.5).
Evaluating differences according to educational attainment, AHEI scores were greater among individuals with a higher education level globally and in most regions, except in the Middle East and Northern Africa and Sub-Saharan Africa, where no differences were evident (Fig. 4). Among world regions, differences by education were largest in Central/Eastern Europe and Central Asia (+3.6; 2.4, 4.9), Latin America and the Caribbean (+3.5; 0.9, 6.0) and South Asia (+2.9; 1.1, 4.9). Globally, more educated individuals had higher scores for fruit (+0.8; 0.7, 0.9), sodium (+0.7; 0.3, 1.1), whole grains (+0.6; 0.4, 0.8) and non-starchy vegetables (+0.5; 0.4, 0.6). However, in contrast, more educated individuals also had lower scores (less favourable consumption levels) for red/processed meat (−0.6; −0.7, −0.5), SSBs (−0.6; −0.8, −0.4) and nuts and legumes (−0.1; −0.2, −0.1) globally.
AHEI score: nine components scored from 0 to 10 each and scaled to ten components (correction not shown). The absolute difference by education was computed as the difference at the stratum level and aggregated to the global and regional mean differences using weighted population proportions for low (<6 years) and high education levels (≥12 years) only (excludes education level ≥6 and <12 years).
Globally, AHEI scores did not significantly vary by urban versus rural residence (Fig. 5). However, higher scores were evident among urban versus rural individuals in Central/Eastern Europe and Central Asia (difference +2.2; 0.9, 3.5), and Southeast and East Asia (+1.4; 0.6, 2.4), and lower scores among urban versus rural individuals in the Middle East and Northern Africa (−3.8; −5.5, −2.2). Globally, individuals residing in urban areas had higher scores for fruit (+0.2; 0.2, 0.3) and whole grains (+0.2; 0.1, 0.4), but lower scores for SSBs (−0.5; −0.7, −0.4), red/processed meat (−0.4, −0.5, −0.1) and legumes/nuts (−0.1; −0.2, −0.1).
Changes in dietary pattern scores between 1990 and 2018
Between 1990 and 2018, the mean global AHEI score (standardized to 2018 population distributions) increased by +1.5 (1.0, 2.0). Increasing trends occurred in five of seven regions: Central/Eastern Europe and Central Asia (+4.6; 4.0, 5.3); high-income countries (+3.2; 2.9, 3.5); Southeast and East Asia (+2.7; 1.7, 3.8); the Middle East and Northern Africa (+2.2; 1.4, 3.0); and Latin America and the Caribbean (+1.3; 0.6, 2.0). No significant change was seen in South Asia (0; −0.9, 1.1), and a decreasing trend was seen in Sub-Saharan Africa (−1.1; −1.8, −0.4) (Fig. 6).
Among AHEI components globally, scores increased over time for non-starchy vegetables (+1.1; 1.0, 1.2), legumes/nuts (+1.1; 1.0, 1.3) and fruit (+0.1; 0.1, 0.2); decreased for red/processed meat (−1.4; −1.5, −1.2), SSBs (−0.6; −0.7, −0.6) and sodium (−0.4; −0.6, −0.2); and remained stable for whole grains (+0.1; 0, 0.2), PUFAs (0; 0, 0.1) and seafood omega-3 (0; 0, 0.1).
Among the most populous countries, the largest absolute improvement in the AHEI score between 1990 and 2018 occurred in Iran (+12.0; 9.9, 13.9), the United States (+4.6; 4.1, 5.1), Vietnam (+4.5; 2.4, 7.2) and China (+4.3; 2.8, 5.9), while the largest declines were found in Tanzania (−3.7; −5.8, −1.5), Nigeria (−3.0; −5.3, −0.7), Japan (−2.7; −3.1, −2.3) and the Philippines (−1.8; −2.7, −0.9) (Fig. 7).
Results for DASH and MED
Detailed findings for the DASH and MED scores are presented in Supplementary Information. Briefly, global mean DASH and MED scores in 2018 were 22.9 (22.6, 23.2) and 4.1 (3.9, 4.2), respectively (Extended Data Figs. 2 and 3). Regionally, means for these scores were consistently higher in South Asia, and lower in Latin America and the Caribbean (Extended Data Figs. 4 and 5). Among population subgroups, global DASH and MED scores were higher among adults compared with children (DASH: 23.2 (22.9, 23.4) versus 22.3 (21.9, 22.7); MED: 4.3 (4.1, 4.4) versus 3.7 (3.5, 3.8)), but did not appreciably differ by sex (Extended Data Figs. 2 and 3). Global mean scores were higher among more versus less educated individuals (difference +2.6 (2.3, 2.8) and +0.3 (0.2, 0.4), respectively) (Extended Data Fig. 7), and, for DASH only, among urban versus rural individuals (+0.4; 0.2, 0.7) (Extended Data Fig. 8). Worldwide, the mean DASH and MED scores increased modestly between 1990 and 2018, by +1.0 (0.8, 1.1) for DASH and +0.3 (0.2, 0.4) for MED (Extended Data Figs. 6 and 9). Across strata in 2018, the inter-correlations of the dietary pattern scores were 0.8 for AHEI and DASH, 0.5 for AHEI and MED, and 0.6 for DASH and MED.
Discussion
In this global assessment of different dietary patterns across 185 countries in 1990 and 2018, we found modest overall dietary quality, but with important variation by age, sex, education, urbanicity, time and world region, as well as by dietary component. These results, based on the systematic collection and standardization of more than 1,100 individual-level dietary surveys worldwide, provide the most current and comprehensive estimates of global, regional and national dietary quality among adults and children, in subgroups according to educational attainment and urban versus rural residence, and comparing three validated dietary patterns including the AHEI, DASH and MED17. These results have important implications for public health and inform priorities in each nation and subnational subgroup to improve nutrition security and health equity.
As one example, our findings highlight the regional differences between insufficient intakes of healthful foods versus excess intakes of unhealthful foods. For instance, the highest dietary pattern scores in 2018 were identified in low-income countries in South Asia and Sub-Saharan Africa, where relatively low consumption of SSBs and red/processed meats is consistent with national data on food or beverage volume sales19. However, consumption of healthy components, such as fruit, non-starchy vegetables, legumes/nuts, seafood omega-3 fat and PUFAs, were also far from optimal in these nations. This suggests that a major focus on policies and innovations to increase intakes of produce, seafood and plant oils will have the largest impact on dietary quality in these countries.
By contrast, in high-income countries, Central/Eastern Europe and Central Asia, and the Middle East and Northern Africa, increasing intakes of fruit, non-starchy vegetables, legumes/nuts and whole grains have improved dietary quality over time, but have been offset by stable trends or only minor reductions in red/processed meats, SSBs and sodium. We found that red/processed meat and sodium have each significantly increased over time in Asia and Latin America and the Caribbean, consistent with previous nation-specific reports from China, Japan and Mexico20,21,22. These findings suggest that a dual focus on increasing healthful foods and lowering of harmful factors is essential in these regions, especially for nations in Asia and Latin America and the Caribbean.
Several studies have documented that the AHEI is associated with the risk of non-communicable diseases23. For example, pooled findings from two US cohorts found a 24%, 33% and 6% reduction in the incidence of cardiovascular disease, diabetes mellitus and cancer, respectively, for the highest AHEI quintile (median 64.5) compared with the lowest quintile (median 36.9; comparable to the global mean in our study, 40.3 (95% UI 39.4, 41.3)) (ref. 24). Cohorts have also found that a moderate increase (20-percentile increase) in the AHEI score during follow-up was associated with significantly lower risk of cardiovascular disease mortality and cancer mortality25. Similar relationships have been observed in France26, the United Kingdom27 and Singapore28,29. Such associations suggest that the current quality of global diets identified in this study is leading to preventable chronic disease and mortality, and that modest improvements in dietary quality can contribute to reductions in fatal and non-fatal diet-related diseases over time.
Our findings on global diet patterns among infants, children and adolescents have important implications for child nutrition and health. We found that diet quality was generally highest among infants and young children and worsened into adolescence, emphasizing the need for initiatives to aim to improve dietary quality in older children, as well as promote healthy eating habits in early childhood to translate into improved dietary quality in adolescence and adulthood. Although, diet quality was highest among children in Sub-Saharan Africa and South Asia, we found that diet quality worsened or remained stable over time in these regions. Children with more educated parents had higher dietary quality in all regions except South Asia and the Middle East and Northern Africa, while better diet quality was found among children residing in urban areas in Central/Eastern Europe and Central Asia and Southeast and East Asia, and rural areas in the Middle East and Northern Africa. Worse dietary quality in children is associated with stunting, cardiometabolic risk factors (for example, blood pressure, blood lipid levels, glucose control and obesity) and lower health-related quality of life30,31,32,33,34,35, and dietary habits and food preferences established during early life influence later habits throughout childhood and into adulthood36,37,38.
Dietary disparities by education or income level have been reported in specific, mostly high-income nations or selected groups of nations8,39,40,41, but not globally. Our findings demonstrate that more educated individuals had higher overall dietary quality in most, but not all, world regions, with largest impacts of education among nations in Central/Eastern Europe and Central Asia, Latin America and the Caribbean, and South Asia. We also identified key exceptions in the Middle East and Northern Africa, and Sub-Saharan Africa, where dietary quality did not vary by education level. Notably, higher education was generally linked to greater consumption of fruits, non-starchy vegetables, whole grains and plant oils, but not always to lower consumption of SSBs and red/processed meat. Interestingly, urbanicity differentially influenced dietary quality in different world regions, with better dietary quality among urban versus rural residents in Central/Eastern Europe and Central Asia and Southeast and East Asia, but the opposite in the Middle East and Northern Africa, related to specific differences in the consumption of the underlying healthful versus unhealthful components among urban versus rural residents in these regions.
In agreement with our earlier analysis of healthy and unhealthy dietary scores16, we found that, compared with lower-income countries, higher-income countries had better scores for healthy components (for example, fruit and whole grains) but worse scores for unhealthy components (for example, red/processed meats and sodium).
This investigation has several strengths. Our data and findings build upon and expand the previous literature by including the largest number of individual-level dietary surveys, providing a more contemporary estimate of trends in global dietary quality and estimating global dietary quality in children and adolescents, which has not been previously reported. We included 1,139 dietary surveys, most of which were nationally representative and collected at the individual-level using 24 h recalls or food-frequency questionnaires (FFQs). We standardized all data inputs including dietary factor definitions, units and age-specific energy adjustment, and incorporated Bayesian modelling with survey and country covariates to address heterogeneity and sampling and modelling uncertainty42. We assessed subnational differences by age, sex, education and urbanicity, including the first global estimates of dietary patterns by educational attainment and urban versus rural residence. We characterized three established metrics for diet quality, each validated against major health outcomes17, including the similarities and differences in global, regional and national dietary quality depending on the dietary metric.
Potential limitations should be considered. While we made extensive efforts to minimize bias and incorporate heterogeneity and uncertainty, individual-level dietary data are subject to measurement errors, and survey availability was limited or incomplete for some nations, dietary factors, demographic groups and years16,42. For example, less than a quarter of surveys included data on children aged 3–9 years and adults ≥85 years. The Bayesian hierarchical models incorporated additional uncertainty to account for these limitations, but sampling and/or information bias cannot be ruled out16. To allow for comparability between population subgroups, we standardized dietary intakes to 2,000 kcal per day before computing the dietary patterns, but the unadjusted dietary intakes may be lower among populations with lower energy requirements (for example, infants and young children, and seniors) or higher among populations consuming >2,000 kcal per day. We did not have information on trans fat (AHEI) or alcohol use (AHEI and MED), and our findings should be interpreted as dietary quality based on the other components of these scores. The dietary patterns selected (AHEI, MED and DASH) were originally developed and validated for adult populations in high-income countries but have been used to characterize dietary quality among children and seniors33,43,44. It is important to note that a single or suite of dietary metrics has not been developed or validated to assess micronutrient quality of the diet in all age groups17, and the AHEI, MED and DASH may be inadequately correlated with nutrients of concern, particularly among children and in low- and middle-income countries. Caution is warranted when interpreting the findings in relation to nutrient adequacy. However, in the absence of validated metrics for the double burden of malnutrition, the AHEI, MED and DASH are appropriate metrics for assessing dietary quality across populations17. We did not consider other, less validated dietary indices and scores16,17,45,46, which can be assessed once these have been better validated for use in diverse global populations.
In conclusion, we found global dietary quality to be only modest today, and with only some improvement, although inconsistent by world region, over the past three decades.
These results provide comprehensive global information about individual-level dietary patterns among children and adults, by age, sex, education and urbanicity. Our findings highlight the substantial variation in dietary quality and inform the need for specific national and subnational policies to improve nutrition security and nutrition equity.
Methods
Data sources and retrieval
Our methods and findings for identifying dietary surveys, data extraction, standardization and harmonization, and modelling have been reported18,42,47,48. In brief, we systematically searched, identified and collated data from nationally and subnationally representative surveys (or local representative community surveys when national and subnational were not available) on individual-level dietary intakes, and for sodium intake, as well as additional biomarker surveys18,42. Household budget surveys were used rarely when individual-level dietary surveys were not identified for a populous country18,42. In total, we compiled data from 1,248 dietary surveys from 188 countries. Of these, 1,139 surveys from 175 countries (representing 7.46 billion of the world population in 2018) reported data on the nine foods, three beverages and six nutrients measured in the dietary pattern scores in the present analysis. Most surveys were nationally or subnationally representative (89.1%); used an FFQ (42.1%) or 24 h recall (22.7%); included data on children (0–19 years) (73.9%) and adults (≥20 years) (64.5%); and included data on urban and/or rural residence (60.8%) (Supplementary Information Table 4).
Data extraction and standardization
For each survey in the GDD, we obtained and assessed the credibility of information obtaining relating to survey characteristics, including survey name, country, years performed, sampling methods, response rate, national representativeness, level of data collection (individual or household), dietary assessment method and validation, sample size, population demographics (age, sex, education, urban/rural residence and pregnancy/lactation status) and definitions and units of dietary factors18. We also extracted or obtained directly from the survey owners data on individual-level dietary intakes of up to 53 foods, beverages and nutrients, jointly stratified by age, sex, education and urban/rural residence. We evaluated dietary intakes adjusted to age-standardized energy intakes to assess dietary composition independently of quantity, account for estimated age-specific average requirements and reduce measurement error within and across surveys (Supplementary Information)42. Data were assessed for extraction errors and for plausibility using standardized protocols, and survey quality by evaluating evidence for selection bias, sample representativeness, response rate and validity of diet assessment method42.
Modelling and uncertainty
To account for differences in survey methods, representativeness, time trends, input data and uncertainty, a Bayesian model estimated the log-means of dietary intake (mean and standard deviation) within a nested hierarchical structure42. The model included random effects by country and region as well as globally; sex, education, urban/rural residence and non-linear age effects; survey-level indicator data for dietary assessment method (24 h recall, FFQ, Demographic Health Survey questionnaire and household budget survey) and type of dietary metric (optimal or suboptimal definition); and national year-specific covariate data relevant to each dietary factor42. The model included overdispersion of study-level variance for surveys that were not nationally representative or not stratified by sex, education, urbanicity or small age groups (≤10 years)42.
The final model included estimates of consumption of each food or nutrient for 264 subgroups jointly stratified by sex (male or female), age group (<1, 1–2, 3–4, 5–9, 10–14, 15–19, 20–24, 25–29, 30–34, 35–39, 40–44, 45–49, 50–54, 55–59, 60–64, 65–69, 70–74, 75–79, 80–84, 85–89, 90–94 and ≥95 years), education (<6 years, ≥6 to <12 years, or ≥12 years) and urban versus rural residence; within 185 countries covering 99.0% of the world’s population in 201842. Uncertainty of each stratum-specific dietary factor estimate was quantified using 4,000 iterations to determine posterior distributions jointly by country, year, age, sex, education and urbanicity42. We computed the median intake and the 95% UI for each stratum from the 50th, 2.5th and 97.5th percentiles of the 4,000 draws, respectively42. Validity checks included: five-fold cross-validation (randomly omitting 20% of the raw survey data, run five times), comparing predicted versus observed intakes; assessment of implausible estimates; and visual assessment of national mean intakes using global heat maps42. A second time-component-based Bayesian model was used to strengthen time trend estimates for dietary factors with corresponding food or nutrient availability data (FAO Food Balance Sheets49 and Global Expanded Nutrient Supply50)42. The model, commonly referred to as a varying slopes model, incorporated country-level intercepts, and slopes, along with their correlation that is estimated across countries42,51,52. The final GDD results were based on these two Bayesian models42, as detailed in Supplementary Information.
Characterization of dietary patterns
For our primary analysis, we focused on the AHEI. For each stratum, we scored nine components: fruit, non-starchy vegetables, whole grains, SSBs, legumes/nuts, unprocessed red/processed meats, seafood omega-3 fat, PUFAs and sodium (alcohol and trans fat were not estimated in GDD) (Supplementary Table 6). Each component was scored from 0 to 10, and the final score ranging from 0 to 90 was scaled to range from 0 to 100. DASH was calculated on the basis of eight components, scored from 1 to 5 using sex-specific quintiles, with the final score ranging from 8 to 40 (Supplementary Table 7). MED was calculated on the basis of eight components (alcohol was not estimated), with each component scored as 0 or 1 using sex-specific medians and the final score ranging from 0 to 8 (Supplementary Table 8). As scoring cutpoints for DASH and MED are based on observed population distributions, distributions were calculated for 2018 and used consistently in other years. As each of these scores is based on usual adult intakes, consumption levels of dietary factors in each stratum were standardized to 2,000 kcal per day for deriving the dietary pattern scores. For each dietary pattern, higher scores are given for higher intakes of healthier foods or nutrients and lower intakes of unhealthier foods or nutrients, and thus higher scores represent healthier diets.
Statistical analysis
Population-weighted average dietary pattern scores for each population subgroup stratum in each country–year were calculated using all 4,000 posterior predictions for each of the components in that stratum to derive global, regional and national scores42. Annual population weights were derived from the United Nations Population Division53, supplemented with data on educational and urban/rural distributions from Barro Lee54 and the United Nations55, respectively42. Spearman correlations assessed inter-relationships between each dietary pattern score. Changes in scores between 1990 and 2018 were calculated using all 4,000 posterior predictions for each stratum to account for the full spectrum of uncertainty and standardized to the proportion of individuals within each stratum in 2018 to account for changes in demographics over time42. Given the Bayesian nature of the analysis, formal statistical significance was not appropriate, and the 95% UIs should be used as a guide42.
Data availability
The modelled estimates of individual food and nutrient intakes by population subgroup, country, region and globe in 1990 and 2018 are available for download from the GDD (https://www.globaldietarydatabase.org/). Survey-level information and original data download weblinks are also provided for all public surveys; survey-level microdata or stratum-level aggregate data are provided for direct download for all non-public surveys granted consent for public sharing by the data owner. The modelled dietary quality scores are available for download from (https://github.com/victoriaemiller/GDD-Diet-Quality).
Code Availability
The statistical coding is available from the corresponding author on reasonable request.
Change history
24 January 2023
A Correction to this paper has been published: https://doi.org/10.1038/s43016-023-00705-0
References
2021 Global Nutrition Report: The State of Global Nutrition (Development Initiatives, 2021).
GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet https://doi.org/10.1016/s0140-6736(18)32203-7 (2018).
GBD 2017 Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet https://doi.org/10.1016/s0140-6736(18)32225-6 (2018).
GBD 2017 Diet Collaborators. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet https://doi.org/10.1016/s0140-6736(19)30041-8 (2019).
Sacks, F. M. et al. Rationale and design of the Dietary Approaches to Stop Hypertension trial (DASH). A multicenter controlled-feeding study of dietary patterns to lower blood pressure. Ann. Epidemiol. 5, 108–118 (1995).
Hu, F. B. Dietary pattern analysis: a new direction in nutritional epidemiology. Curr. Opin. Lipidol. 13, 3–9 (2002).
Micha, R. et al. Etiologic effects and optimal intakes of foods and nutrients for risk of cardiovascular diseases and diabetes: systematic reviews and meta-analyses from the Nutrition and Chronic Diseases Expert Group (NutriCoDE). PLoS ONE 12, e0175149 (2017).
Teo, K. et al. Prevalence of a healthy lifestyle among individuals with cardiovascular disease in high-, middle- and low-income countries: the Prospective Urban Rural Epidemiology (PURE) study. JAMA 309, 1613–1621 (2013).
Yusuf, S. et al. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet 395, 795–808 (2020).
Ezzati, M. & Riboli, E. Behavioral and dietary risk factors for noncommunicable diseases. N. Engl. J. Med. 369, 954–964 (2013).
Kennedy, G., Nantel, G. & Shetty, P. Globalization of food systems in developing countries: impact on food security and nutrition. FAO Food Nutr. Pap. 83, 1–300 (2004).
Wang, D. D. et al. Global improvement in dietary quality could lead to substantial reduction in premature death. J. Nutr. 149, 1065–1074 (2019).
Vandevijvere, S. et al. Monitoring and benchmarking population diet quality globally: a step-wise approach. Obes. Rev. 14, 135–149 (2013).
Green, R., Sutherland, J., Dangour, A. D., Shankar, B. & Webb, P. Global dietary quality, undernutrition and non-communicable disease: a longitudinal modelling study. BMJ Open 6, e009331 (2016).
Del Gobbo, L. C. et al. Assessing global dietary habits: a comparison of national estimates from the FAO and the Global Dietary Database. Am. J. Clin. Nutr. 101, 1038–1046 (2015).
Imamura, F. et al. Dietary quality among men and women in 187 countries in 1990 and 2010: a systematic assessment. Lancet Glob. Health 3, e132–e142 (2015).
Miller, V., Webb, P., Micha, R. & Mozaffarian, D. Defining diet quality: a synthesis of dietary quality metrics and their validity for the double burden of malnutrition. Lancet Planet Health 4, e352–e370 (2020).
Miller, V. et al. Global Dietary Database 2017: data availability and gaps on 54 major foods, beverages and nutrients among 5.6 million children and adults from 1220 surveys worldwide. BMJ Global Health 6, e003585 (2021).
Vandevijvere, S. et al. Global trends in ultraprocessed food and drink product sales and their association with adult body mass index trajectories. Obes. Rev. 20, 10–19 (2019).
Li, Y. et al. Time trends of dietary and lifestyle factors and their potential impact on diabetes burden in China. Diabetes Care 40, 1685–1694 (2017).
Murakami, K., Livingstone, M. B. E. & Sasaki, S. Thirteen-year trends in dietary patterns among Japanese adults in the National Health and Nutrition Survey 2003–2015: continuous Westernization of the Japanese diet. Nutrients 10, 994 (2018).
Marrón-Ponce, J. A., Tolentino-Mayo, L., Hernández-F, M. & Batis, C. Trends in ultra-processed food purchases from 1984 to 2016 in Mexican Households. Nutrients 11, 45 (2018).
Schwingshackl, L., Bogensberger, B. & Hoffmann, G. Diet quality as assessed by the healthy eating index, alternate healthy eating index, dietary approaches to stop hypertension score, and health outcomes: an updated systematic review and meta-analysis of cohort studies. J. Acad. Nutr. Diet 118, 74–100.e111 (2018).
Chiuve, S. E. et al. Alternative dietary indices both strongly predict risk of chronic disease. J. Nutr. 142, 1009–1018 (2012).
Sotos-Prieto, M. et al. Association of changes in diet quality with total and cause-specific mortality. N. Engl. J. Med. 377, 143–153 (2017).
Trébuchet, A. et al. Prospective association between several dietary scores and risk of cardiovascular diseases: is the Mediterranean diet equally associated to cardiovascular diseases compared to National Nutritional Scores? Am. Heart J. 217, 1–12 (2019).
Shivappa, N., Hebert, J. R., Kivimaki, M. & Akbaraly, T. Alternative Healthy Eating Index 2010, Dietary Inflammatory Index and risk of mortality: results from the Whitehall II cohort study and meta-analysis of previous Dietary Inflammatory Index and mortality studies. Br. J. Nutr. 118, 210–221 (2017).
Neelakantan, N., Koh, W.-P., Yuan, J.-M. & van Dam, R. M. Diet-quality indexes are associated with a lower risk of cardiovascular, respiratory, and all-cause mortality among Chinese adults. J. Nutr. 148, 1323–1332 (2018).
Chen, G.-C. et al. Diet quality indices and risk of type 2 diabetes mellitus: The Singapore Chinese Health Study. Am. J. Epidemiol. 187, 2651–2661 (2018).
Wu, X. Y. et al. The influence of diet quality and dietary behavior on health-related quality of life in the general population of children and adolescents: a systematic review and meta-analysis. Qual. Life Res. 28, 1989–2015 (2019).
Dalwood, P., Marshall, S., Burrows, T. L., McIntosh, A. & Collins, C. E. Diet quality indices and their associations with health-related outcomes in children and adolescents: an updated systematic review. Nutr. J. 19, 118 (2020).
Jennings, A., Welch, A., van Sluijs, E. M., Griffin, S. J. & Cassidy, A. Diet quality is independently associated with weight status in children aged 9-10 years. J. Nutr. 141, 453–459 (2011).
Marshall, S., Burrows, T. & Collins, C. E. Systematic review of diet quality indices and their associations with health-related outcomes in children and adolescents. J. Hum. Nutr. Diet 27, 577–598 (2014).
Krasevec, J., An, X., Kumapley, R., Bégin, F. & Frongillo, E. A. Diet quality and risk of stunting among infants and young children in low- and middle-income countries. Matern. Child Nutr. https://doi.org/10.1111/mcn.12430 (2017).
Martin-Calvo, N., Chavarro, J. E., Falbe, J., Hu, F. B. & Field, A. E. Adherence to the Mediterranean dietary pattern and BMI change among US adolescents. Int. J. Obes. 40, 1103–1108 (2016).
Switkowski, K. M., Gingras, V., Rifas-Shiman, S. L. & Oken, E. Patterns of complementary feeding behaviors predict diet quality in early childhood. Nutrients 12, 810 (2020).
Mikkilä, V., Räsänen, L., Raitakari, O. T., Pietinen, P. & Viikari, J. Longitudinal changes in diet from childhood into adulthood with respect to risk of cardiovascular diseases: The Cardiovascular Risk in Young Finns Study. Eur. J. Clin. Nutr. 58, 1038–1045 (2004).
Lake, A. A., Mathers, J. C., Rugg-Gunn, A. J. & Adamson, A. J. Longitudinal change in food habits between adolescence (11–12 years) and adulthood (32–33 years): the ASH30 Study. J. Public Health 28, 10–16 (2006).
Wang, D. D. et al. Trends in dietary quality among adults in the United States, 1999 through 2010. JAMA Intern. Med. 174, 1587–1595 (2014).
Fang Zhang, F. et al. Trends and disparities in diet quality among US adults by supplemental nutrition assistance program participation status. JAMA Netw. Open 1, e180237 (2018).
Dehghan, M. et al. Relationship between healthy diet and risk of cardiovascular disease among patients on drug therapies for secondary prevention. Circulation 126, 2705–2712 (2012).
Miller, V. et al. Global, regional, and national consumption of animal-source foods between 1990 and 2018: findings from the Global Dietary Database. Lancet Planet. Health 6, e243–e256 (2022).
Chen, X., Maguire, B., Brodaty, H. & O’Leary, F. Dietary patterns and cognitive health in older adults: a systematic review. J. Alzheimers Dis. 67, 583–619 (2019).
Roman, B., Carta, L., Martínez-González, M. A. & Serra-Majem, L. Effectiveness of the Mediterranean diet in the elderly. Clin. Interv. Aging 3, 97–109 (2008).
Bromage, S. et al. Development and validation of a novel food-based global diet quality score (GDQS). J. Nutr. 151, 75s–92s (2021).
Herforth, A. W., Wiesmann, D., Martínez-Steele, E., Andrade, G. & Monteiro, C. A. Introducing a suite of low-burden diet quality indicators that reflect healthy diet patterns at population level. Curr. Dev. Nutr. 4, nzaa168–nzaa168 (2020).
Micha, R. et al. Estimating the global and regional burden of suboptimal nutrition on chronic disease: methods and inputs to the analysis. Eur. J. Clin. Nutr. 66, 119–129 (2012).
Khatibzadeh, S. et al. A global database of food and nutrient consumption. Bull. World Health Organ. 94, 931–934 (2016).
Food and Agriculture Organization of the United Nations. Food balances. 2021. https://www.fao.org/faostat/en/#data2021 (accessed March 3, 2021).
Smith, M. R., Micha, R., Golden, C. D., Mozaffarian, D. & Myers, S. S. Global Expanded Nutrient Supply (GENuS) Model: a new method for estimating the global dietary supply of nutrients. PLoS ONE 11, e0146976 (2016).
Gelman, A. & Pardoe, I. Bayesian measures of explained variance and pooling in multilevel (hierarchical) models. Technometrics 48, 241–251 (2006).
Wagner, T., Diefenbach, D. R., Christensen, S. & Norton, A. S. Using multilevel models to quantify heterogeneity in resource selection. J. Wildl. Manag. 75, 1788–1796 (2011).
United Nations Population Division. Total population by sex (thousands). 2019. https://population.un.org/wpp/DataQuery/2019 (accessed June 12, 2020).
Barro, R. & Lee, J. A new data set of educational attainment in the world, 1950–2010. J. Dev. Econ 104, 184–198 (2013).
United Nations Population Division. Urban population (% of total population). 2018. https://data.worldbank.org/indicator/SP.URB. TOTL.IN.ZS2018 (accessed June 12, 2020).
Acknowledgements
We thank R. Micha for her work harmonizing the individual dietary surveys included in the GDD. We thank the GDD corresponding members for sharing and harmonizing their dietary surveys in accordance with the GDD methods. This study was supported by grants from the Bill and Melinda Gates Foundation (OPP1176681; D.M.) and from the American Heart Association (20POST35200069; V.M.). The Bill and Melinda Gates Foundation contributed to study design during the grant application process; the funders otherwise had no role in data collection, data analysis, data interpretation or writing of the report.
Author information
Authors and Affiliations
Consortia
Contributions
V.M., P.W. and D.M. conceptualized and designed the study. V.M., R.M., J.R. and J.C. were involved in the data collection. V.M., F.C., J.Z., P.S. and J.E.-M. conducted the analyses for the study. V.M., P.W. and D.M. drafted the manuscript. All the authors interpreted the data, read the final manuscript, reviewed it for important intellectual content and approved its submission. V.M. and D.M. are the guarantors of this work.
Corresponding author
Ethics declarations
Competing interests
V.M. reports research funding from the Canadian Institutes of Health Research, outside the submitted work. P.W. reports research grants and contracts from the United States Agency for International Development and personal fees from the Global Panel on Agriculture and Food Systems for Nutrition, outside the submitted work. J.R., J.Z. and P.S. report research funding from Nestlé, outside the submitted work. J.C. reports research funding from the Bill and Melinda Gates Foundation and the United States Agency for International Development, and personal fees from UNICEF/WHO, outside the submitted work. D.M. reports research funding from the National Institutes of Health and the Bill and Melinda Gates Foundation; personal fees from GOED, Bunge, Indigo Agriculture, Motif FoodWorks, Amarin, Acasti Pharma, Cleveland Clinic Foundation, America’s Test Kitchen and Danone; scientific advisory board member for Brightseed, DayTwo, Elysium Health, Filtricine, HumanCo and Tiny Organics; and chapter royalties from UpToDate, all outside the submitted work. The other authors have no disclosures to declare.
Peer review
Peer review information
Nature Food thanks Inge Tetens and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Global and regional AHEI score by (A) sex, (B) education, and (C) urban/rural residence in 2018.
Data are the mean score (95% uncertainty interval). The AHEI score ranged from 0 to 100. <6 years: <6 years of education; ≥6 to <12 years: ≥6 to <12 years of education; ≥12 years: ≥12 years of education. Rural: rural residence; urban: urban residence.
Extended Data Fig. 2 Global and regional DASH score by (A) age, (B) sex, (C) education, and (D) urban/rural residence in 2018.
Data are the mean score (95% uncertainty interval). The DASH score ranged from 5 to 40. <6 years: <6 years of education; ≥6 to <12 years: ≥6 to <12 years of education; ≥12 years: ≥12 years of education. Rural: rural residence; urban: urban residence.
Extended Data Fig. 3 Global and regional MED score by (A) age, (B) sex, (C) education, and (D) urban/rural residence in 2018.
Data are the mean score (95% uncertainty interval). The MED score ranged from 0 to 8. <6 years: <6 years of education; ≥6 to <12 years: ≥6 to <12 years of education; ≥12 years: ≥12 years of education. Rural: rural residence; urban: urban residence.
Extended Data Fig. 4 Global and region mean DASH scores (top panel), and MED scores (bottom panel) among all ages (children and adults) in 2018.
The DASH score ranged from 5 to 40, and the MED score ranged from 0 to 8.
Extended Data Fig. 5 National mean DASH scores (top panel), and MED scores (bottom panel) among all ages (children and adults) in 2018.
The DASH score ranged from 5 to 40, and the MED score ranged from 0 to 8.
Extended Data Fig. 6 National mean absolute change in DASH scores (top panel), and MED scores (bottom panel) among all ages (children and adults) in 2018.
The DASH score ranged from 5 to 40, and the MED score ranged from 0 to 8. The absolute difference between 2018 and 1990 was computed as the difference at the stratum-level and aggregated to the global and regional mean differences using weighted population proportions for 2018.
Extended Data Fig. 7 Global and regional mean absolute difference in DASH component scores (top panel) and MED component scores (bottom panel) in all ages (children and adults) in 2018, by high versus low education level.
The absolute difference by education was computed as the difference at the stratum-level and aggregated to the global and regional mean differences using weighted population proportions for low (<6 years) and high education levels (≥12 years) only (excludes education level = ≥6 to <12 years).
Extended Data Fig. 8 Global and regional mean absolute difference in DASH component scores (top panel) and MED component scores (bottom panel) in all ages (children and adults) in 2018, by urban versus rural residence.
The absolute difference by urbanicity was computed as the difference at the stratum-level and aggregated to the global and regional mean differences using weighted population proportions.
Extended Data Fig. 9 Global and regional mean absolute difference in DASH component scores (top panel) and MED component scores (bottom panel) in all ages (children and adults) between 2018 and 1990.
The absolute difference by time was computed as the difference at the stratum-level and aggregated to the global and regional mean differences using weighted population proportions for 2018.
Supplementary information
Supplementary Information
Supplementary methods, Tables 1–8 and discussion.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Miller, V., Webb, P., Cudhea, F. et al. Global dietary quality in 185 countries from 1990 to 2018 show wide differences by nation, age, education, and urbanicity. Nat Food 3, 694–702 (2022). https://doi.org/10.1038/s43016-022-00594-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s43016-022-00594-9
This article is cited by
-
Cross-country health inequalities of four common nutritional deficiencies among children, 1990 to 2019: data from the Global Burden of Disease Study 2019
BMC Public Health (2024)
-
Gender differences in the association between healthy eating index-2015 and hypertension in the US population: evidence from NHANES 1999–2018
BMC Public Health (2024)
-
Nutritional status in patients with chronic pancreatitis and liver cirrhosis is related to disease conditions and not dietary habits
Scientific Reports (2024)
-
Metabolic risks remain a serious threat to cardiovascular disease: findings from the Global Burden of Disease Study 2019
Internal and Emergency Medicine (2024)
-
Accounting for nutrition-related health impacts in food life cycle assessment: insights from an expert workshop
The International Journal of Life Cycle Assessment (2024)