Abstract
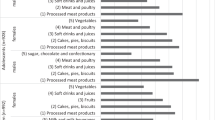
The world faces a global nutrition crisis, most clearly evidenced by the twin pandemics of obesity and type 2 diabetes (T2DM). Yet, substantial confusion and controversy exist about optimal dietary priorities and policy approaches to address these challenges. This paper reviews the evolution of nutritional evidence, emerging areas and corresponding policy lessons to address obesity and T2DM. This includes the complexity of diet–health pathways for long-term weight maintenance and metabolic health; a need to focus on both increasing protective foods (for example, minimally processed, phytochemical-rich foods) and reducing detrimental factors (for example, refined starches, added sugars and processed meats); and critical assessment of popular diets for weight-loss and metabolic health. Emerging evidence highlights areas for further research, including those related to food processing, non-nutritive sweeteners, emulsifiers, the microbiome, flavonoids and personalized nutrition. Evidence-based, multi-sectoral policy actions to address the global nutrition crisis are shown to span several domains, including health systems, economic incentives, school and workplace environments, quality and labelling standards, and innovation and entrepreneurship.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Bloom, D. et al. The Global Economic Burden of Noncommunicable Diseases (World Economic Forum, 2011).
GBD 2017 Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 392, 1923–1994 (2018).
Wang, D. D. et al. Global improvement in dietary quality could lead to substantial reduction in premature death. J. Nutrit. 149, 1065–1074 (2019).
Perez-Escamilla, R. et al. Nutrition disparities and the global burden of malnutrition. BMJ 361, k2252 (2018).
Bustamante, M. et al. Co-benefits, trade-offs, barriers and policies for greenhouse gas mitigation in the agriculture, forestry and other land use (AFOLU) sector. Glob. Chang. Biol. 20, 3270–3290 (2014).
Sims, R. E. H. et al. Energy-smart food for people and climate (FAO, 2011).
AQUASTAT (FAO, 2016); http://www.fao.org/nr/water/aquastat/water_use/index.stm
Kissinger, G., Herold, M. & De Sy, V. Drivers of Deforestation and Forest Degradation: A Synthesis Report for REDD+ Policymakers (Government of the UK & Government of Norway, 2012).
NCD-RisC. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet 390, 2627–2642 (2017).
NCD-RisC. Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet 387, 1513–1530 (2016).
NCD-RisC. Rising rural body-mass index is the main driver of the global obesity epidemic in adults. Nature 569, 260–264 (2019).
Mozaffarian, D. & Forouhi, N. G. Dietary guidelines and health-is nutrition science up to the task? BMJ 360, k822 (2018).
Mozaffarian, D., Rosenberg, I. & Uauy, R. History of modern nutrition science-implications for current research, dietary guidelines, and food policy. BMJ 361, k2392 (2018).
Pingali, P. L. Green revolution: impacts, limits, and the path ahead. Proc. Natl Acad. Sci. USA 109, 12302–12308 (2012).
Mozaffarian, D., Hao, T., Rimm, E. B., Willett, W. C. & Hu, F. B. Changes in diet and lifestyle and long-term weight gain in women and men. N. Engl. J. Med. 364, 2392–2404 (2011).
Pan, A. et al. Changes in water and beverage intake and long-term weight changes: results from three prospective cohort studies. Int. J. Obes. 37, 1378–1385 (2013).
Wang, H. et al. Longitudinal association between dairy consumption and changes of body weight and waist circumference: the Framingham Heart Study. Int. J. Obes. 38, 299–305 (2014).
Smith, J. D. et al. Changes in intake of protein foods, carbohydrate amount and quality, and long-term weight change: results from 3 prospective cohorts. Am. J. Clin. Nutr. 101, 1216–1224 (2015).
Bertoia, M. L. et al. Changes in intake of fruits and vegetables and weight change in United States men and women followed for up to 24 years: analysis from three prospective cohort studies. PLoS Med. 12, e1001878 (2015).
Hall, K. D. et al. Ultra-processed diets cause excess calorie intake and weight gain: an inpatient randomized controlled trial of ad libitum food intake. Cell Metab. 30, 226 (2019).
Ebbeling, C. B. et al. Effects of dietary composition on energy expenditure during weight-loss maintenance. JAMA 307, 2627–2634 (2012).
Ebbeling, C. B. et al. Effects of a low carbohydrate diet on energy expenditure during weight loss maintenance: randomized trial. BMJ 363, k4583 (2018).
Mozaffarian, D. & Wu, J. H. Omega-3 fatty acids and cardiovascular disease: effects on risk factors, molecular pathways, and clinical events. J. Am. Coll. Cardiol. 58, 2047–2067 (2011).
Mozaffarian, D. Dietary and policy priorities for cardiovascular disease, diabetes, and obesity: a comprehensive review. Circulation 133, 187–225 (2016).
Mozaffarian, D. & Wu, J. H. Y. Flavonoids, dairy foods, and cardiovascular and metabolic health: a review of emerging biologic pathways. Circ. Res. 122, 369–384 (2018).
Wu, J. H. Y., Micha, R. & Mozaffarian, D. Dietary fats and cardiometabolic disease: mechanisms and effects on risk factors and outcomes. Nat. Rev. Cardiol. 16, 581–601 (2019).
Astrup, A. et al. WHO draft guidelines on dietary saturated and trans fatty acids: time for a new approach? BMJ 366, l4137 (2019).
Micha, R. et al. Etiologic effects and optimal intakes of foods and nutrients for risk of cardiovascular diseases and diabetes: Systematic reviews and meta-analyses from the Nutrition and Chronic Diseases Expert Group (NutriCoDE). PLoS ONE 12, e0175149 (2017).
Shai, I. et al. Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet. N. Engl. J. Med. 359, 229–241 (2008).
Ajala, O., English, P. & Pinkney, J. Systematic review and meta-analysis of different dietary approaches to the management of type 2 diabetes. Am. J. Clin. Nutr. 97, 505–516 (2013).
Estruch, R. et al. Effect of a high-fat Mediterranean diet on bodyweight and waist circumference: a prespecified secondary outcomes analysis of the PREDIMED randomised controlled trial. Lancet Diabet. Endocrinol. 7, 6–17 (2019).
Cespedes, E. M. et al. Multiple healthful dietary patterns and type 2 diabetes in the women’s health initiative. Am. J. Epidemiol. 183, 622–633 (2016).
Howard, B. V. et al. Low-fat dietary pattern and risk of cardiovascular disease: the women’s health initiative randomized controlled dietary modification trial. JAMA 295, 655–666 (2006).
Dietary Guidelines Advisory Committee. Scientific Report of the 2015 Dietary Guidelines Advisory Committee (USDA, 2015).
Salas-Salvado, J. et al. Prevention of diabetes with Mediterranean diets: a subgroup analysis of a randomized trial. Ann. Intern. Med. 160, 1–10 (2014).
Estruch, R. et al. Primary prevention of cardiovascular disease with a Mediterranean diet supplemented with extra-virgin olive oil or nuts. N. Engl. J. Med. 378, e34 (2018).
Tindall, A. M., Johnston, E. A., Kris-Etherton, P. M. & Petersen, K. S. The effect of nuts on markers of glycemic control: a systematic review and meta-analysis of randomized controlled trials. Am. J. Clin. Nutr. 109, 297–314 (2019).
Huang, H., Chen, G., Liao, D., Zhu, Y. & Xue, X. Effects of berries consumption on cardiovascular risk factors: a meta-analysis with trial sequential analysis of randomized controlled trials. Sci. Rep. 6, 23625 (2016).
Schwingshackl, L. et al. Olive oil in the prevention and management of type 2 diabetes mellitus: a systematic review and meta-analysis of cohort studies and intervention trials. Nutr. Diabet. 7, e262 (2017).
Livesey, G. et al. Dietary glycemic index and load and the risk of type 2 diabetes: a systematic review and updated meta-analyses of prospective cohort studies. Nutrients 11, 1280 (2019).
Ludwig, D. S. Aways Hungry? (Grand Central Life and Style, 2016).
Hu, T. et al. Effects of low-carbohydrate diets versus low-fat diets on metabolic risk factors: a meta-analysis of randomized controlled clinical trials. Am. J. Epidemiol. 176, S44–54 (2012).
Tobias, D. K. et al. Effect of low-fat diet interventions versus other diet interventions on long-term weight change in adults: a systematic review and meta-analysis. Lancet Diabet. Endocrinol. 3, 968–979 (2015).
Huntriss, R., Campbell, M. & Bedwell, C. The interpretation and effect of a low-carbohydrate diet in the management of type 2 diabetes: a systematic review and meta-analysis of randomised controlled trials. Eur. J. Clin. Nutr. 72, 311–325 (2018).
Vasilaras, T. H., Raben, A. & Astrup, A. Twenty-four hour energy expenditure and substrate oxidation before and after 6 months’ ad libitum intake of a diet rich in simple or complex carbohydrates or a habitual diet. Int. J. Obes. Relat. Metab. Disord. 25, 954–965 (2001).
Weickert, M. O. & Pfeiffer, A. F. H. Impact of dietary fiber consumption on insulin resistance and the prevention of type 2 diabetes. J. Nutrition 148, 7–12 (2018).
Shukla, A. P., Iliescu, R. G., Thomas, C. E. & Aronne, L. J. Food order has a significant impact on postprandial glucose and insulin levels. Diabetes Care 38, 98–99 (2015).
Kim, Y., Keogh, J. B. & Clifton, P. M. Differential effects of red meat/refined grain diet and dairy/chicken/nuts/whole grain diet on glucose, insulin and triglyceride in a randomized crossover study. Nutrients 8, 687 (2016).
Kasubuchi, M., Hasegawa, S., Hiramatsu, T., Ichimura, A. & Kimura, I. Dietary gut microbial metabolites, short-chain fatty acids, and host metabolic regulation. Nutrients 7, 2839–2849 (2015).
Birt, D. F. et al. Resistant starch: promise for improving human health. Adv. Nutr. 4, 587–601 (2013).
Snelson, M. et al. Metabolic effects of resistant starch type 2: a systematic literature review and meta-analysis of randomized controlled trials. Nutrients 11, 1833 (2019).
Wang, Y. et al. Effects of the resistant starch on glucose, insulin, insulin resistance, and lipid parameters in overweight or obese adults: a systematic review and meta-analysis. Nutr. Diabetes 9, 19 (2019).
Mozaffarian, R. S. et al. Identifying whole grain foods: a comparison of different approaches for selecting more healthful whole grain products. Public Health Nutr. 16, 2255–2264 (2013).
Ghodsian, B. & Madden, A. M. Evaluating the ≤10:1 wholegrain criterion in identifying nutrient quality and health implications of UK breads and breakfast cereals. Public Health Nutr. 21, 1186–1193 (2018).
Michalski, M. C. et al. Multiscale structures of lipids in foods as parameters affecting fatty acid bioavailability and lipid metabolism. Prog. Lipid Res. 52, 354–373 (2013).
Alhazmi, A., Stojanovski, E., McEvoy, M. & Garg, M. L. Macronutrient intakes and development of type 2 diabetes: a systematic review and meta-analysis of cohort studies. J. Am. Coll. Nutr. 31, 243–258 (2012).
Imamura, F. et al. Effects of saturated fat, polyunsaturated fat, monounsaturated fat, and carbohydrate on glucose-insulin homeostasis: a systematic review and meta-analysis of randomised controlled feeding trials. PLoS Med. 13, e1002087 (2016).
Micha, R. & Mozaffarian, D. Saturated fat and cardiometabolic risk factors, coronary heart disease, stroke, and diabetes: a fresh look at the evidence. Lipids 45, 893–905 (2010).
Wu, J. H. Y. et al. Omega-6 fatty acid biomarkers and incident type 2 diabetes: pooled analysis of individual-level data for 39 740 adults from 20 prospective cohort studies. Lancet Diabet. Endocrinol. 5, 965–974 (2017).
Zong, G. et al. Associations between linoleic acid intake and incident type 2 diabetes among U.S. men and women. Diabetes Care 42, 1406–1413 (2019).
Zhao, J. V. & Schooling, C. M. Effect of linoleic acid on ischemic heart disease and its risk factors: a Mendelian randomization study. BMC Med. 17, 61 (2019).
Imamura, F. et al. Fatty acid biomarkers of dairy fat consumption and incidence of type 2 diabetes: a pooled analysis of prospective cohort studies. PLoS Med. 15, e1002670 (2018).
Abbott, K. A., Burrows, T. L., Thota, R. N., Acharya, S. & Garg, M. L. Do omega-3 PUFAs affect insulin resistance in a sex-specific manner? a systematic review and meta-analysis of randomized controlled trials. Am. J. Clin. Nutr. 104, 1470–1484 (2016).
Wu, J. H. et al. Omega-3 fatty acids and incident type 2 diabetes: a systematic review and meta-analysis. Br. J. Nutr. 107, S214–227 (2012).
Fretts, A. M. et al. Associations of circulating very-long-chain saturated fatty acids and incident type 2 diabetes: a pooled analysis of prospective cohort studies. Am. J. Clin. Nutr. 109, 1216–1223 (2019).
Lemaitre, R. N. et al. Plasma phospholipid very-long-chain saturated fatty acids and incident diabetes in older adults: the Cardiovascular Health Study. Am. J. Clin. Nutr. 101, 1047–1054 (2015).
Morton, R. W. et al. A systematic review, meta-analysis and meta-regression of the effect of protein supplementation on resistance training-induced gains in muscle mass and strength in healthy adults. Br. J. Sports Med. 52, 376–384 (2018).
Liao, C. D. et al. Effects of protein supplementation combined with resistance exercise on body composition and physical function in older adults: a systematic review and meta-analysis. Am. J. Clin. Nutr. 106, 1078–1091 (2017).
Schwingshackl, L. & Hoffmann, G. Long-term effects of low-fat diets either low or high in protein on cardiovascular and metabolic risk factors: a systematic review and meta-analysis. Nutr. J. 12, 48 (2013).
Ye, J. et al. Dietary protein intake and subsequent risk of type 2 diabetes: a dose-response meta-analysis of prospective cohort studies. Acta Diabetol. 56, 851–870 (2019).
Blachier, F. et al. High-protein diets for weight management: interactions with the intestinal microbiota and consequences for gut health. a position paper by the my new gut study group. Clin. Nutr. 38, 1012–1022 (2019).
Pan, A. et al. Red meat consumption and risk of type 2 diabetes: 3 cohorts of US adults and an updated meta-analysis. Am. J. Clin. Nutr. 94, 1088–1096 (2011).
Uribarri, J. et al. Advanced glycation end products in foods and a practical guide to their reduction in the diet. J. Am. Diet. Assoc. 110, 911–916 (2010).
Micha, R., Michas, G., Lajous, M. & Mozaffarian, D. Processing of meats and cardiovascular risk: time to focus on preservatives. BMC Med. 11, 136 (2013).
Rohrmann, S. & Linseisen, J. Processed meat: the real villain? Proc. Nutr. Soc. 75, 233–241 (2016).
Zhao, Z. et al. Body iron stores and heme-iron intake in relation to risk of type 2 diabetes: a systematic review and meta-analysis. PLoS ONE 7, e41641 (2012).
Fernandez-Real, J. M., McClain, D. & Manco, M. Mechanisms linking glucose homeostasis and iron metabolism toward the onset and progression of type 2 diabetes. Diabetes Care 38, 2169–2176 (2015).
Zeng, L. et al. Trends in processed meat, unprocessed red meat, poultry, and fish consumption in the United States, 1999–2016. J. Acad. Nutr. Diet. 119, 1085–1098 (2019).
Zhang, Q., Wu, Y. & Fei, X. Effect of probiotics on body weight and body-mass index: a systematic review and meta-analysis of randomized, controlled trials. Int. J. Food Sci. Nutr. 67, 571–580 (2015).
Sun, J. & Buys, N. J. Glucose- and glycaemic factor-lowering effects of probiotics on diabetes: a meta-analysis of randomised placebo-controlled trials. Br. J. Nutr. 115, 1167–1177 (2016).
Loman, B. R., Hernandez-Saavedra, D., An, R. & Rector, R. S. Prebiotic and probiotic treatment of nonalcoholic fatty liver disease: a systematic review and meta-analysis. Nutr. Rev. 76, 822–839 (2018).
Kanazawa, I. Osteocalcin as a hormone regulating glucose metabolism. World J. Diabetes 6, 1345–1354 (2015).
Rosqvist, F. et al. Potential role of milk fat globule membrane in modulating plasma lipoproteins, gene expression, and cholesterol metabolism in humans: a randomized study. Am. J. Clin. Nutr. 102, 20–30 (2015).
Hjerpsted, J., Leedo, E. & Tholstrup, T. Cheese intake in large amounts lowers LDL-cholesterol concentrations compared with butter intake of equal fat content. Am. J. Clin. Nutr. 94, 1479–1484 (2011).
Soerensen, K. V., Thorning, T. K., Astrup, A., Kristensen, M. & Lorenzen, J. K. Effect of dairy calcium from cheese and milk on fecal fat excretion, blood lipids, and appetite in young men. Am. J. Clin. Nutr. 99, 984–991 (2014).
Demmer, E. et al. Addition of a dairy fraction rich in milk fat globule membrane to a high-saturated fat meal reduces the postprandial insulinaemic and inflammatory response in overweight and obese adults. J. Nutr. Sci. 5, e14 (2016).
Beals, E. et al. Addition of milk fat globule membrane-enriched supplement to a high-fat meal attenuates insulin secretion and induction of soluble epoxide hydrolase gene expression in the postprandial state in overweight and obese subjects. J. Nutr. Sci. 8, e16 (2019).
Vors, C. et al. Milk polar lipids reduce lipid cardiovascular risk factors in overweight postmenopausal women: towards a gut sphingomyelin-cholesterol interplay. Gut https://doi.org/10.1136/gutjnl-2018-318155 (2019).
Geng, T., Qi, L. & Huang, T. Effects of dairy products consumption on body weight and body composition among adults: an updated meta-analysis of 37 randomized control trials. Mol. Nutr. Food Res. 62, 1700410 (2018).
Nupponen, M. et al. Metabolic syndrome from adolescence to early adulthood: effect of infancy-onset dietary counseling of low saturated fat: the Special Turku Coronary Risk Factor Intervention Project (STRIP). Circulation 131, 605–613 (2015).
Sluijs, I. et al. The amount and type of dairy product intake and incident type 2 diabetes: results from the EPIC-InterAct Study. Am. J. Clin. Nutr. 96, 382–390 (2012).
Chen, M. et al. Dairy consumption and risk of type 2 diabetes: 3 cohorts of US adults and an updated meta-analysis. BMC Med. 12, 215 (2014).
Ericson, U. et al. Food sources of fat may clarify the inconsistent role of dietary fat intake for incidence of type 2 diabetes. Am. J. Clin. Nutr. 101, 1065–1080 (2015).
Diaz-Lopez, A. et al. Dairy product consumption and risk of type 2 diabetes in an elderly Spanish Mediterranean population at high cardiovascular risk. Eur. J. Nutr. 55, 349–360 (2015).
Ding, M., Bhupathiraju, S. N., Chen, M., van Dam, R. M. & Hu, F. B. Caffeinated and decaffeinated coffee consumption and risk of type 2 diabetes: a systematic review and a dose-response meta-analysis. Diabet. Care 37, 569–586 (2014).
Yang, W. S., Wang, W. Y., Fan, W. Y., Deng, Q. & Wang, X. Tea consumption and risk of type 2 diabetes: a dose-response meta-analysis of cohort studies. Br. J. Nutr. 111, 1329–1339 (2014).
Zheng, X. X. et al. Effects of green tea catechins with or without caffeine on glycemic control in adults: a meta-analysis of randomized controlled trials. Am. J. Clin. Nutr. 97, 750–762 (2013).
Li, Y. et al. Effects of tea or tea extract on metabolic profiles in patients with type 2 diabetes mellitus: a meta-analysis of 10 randomized controlled trials. Diabet. Metab. Res. Rev. 32, 2–10 (2015).
Kondo, Y. et al. Effects of coffee and tea consumption on glucose metabolism: a systematic review and network meta-analysis. Nutrients 11, 48 (2018).
Liu, G. et al. Effects of tea intake on blood pressure: a meta-analysis of randomised controlled trials. Br. J. Nutr. 112, 1043–1054 (2014).
Onakpoya, I., Spencer, E., Heneghan, C. & Thompson, M. The effect of green tea on blood pressure and lipid profile: a systematic review and meta-analysis of randomized clinical trials. Nutr. Metab. Cardiovasc. Dis. 24, 823–836 (2014).
Wang, D., Chen, C., Wang, Y., Liu, J. & Lin, R. Effect of black tea consumption on blood cholesterol: a meta-analysis of 15 randomized controlled trials. PLoS ONE 9, e107711 (2014).
Nordestgaard, A. T., Thomsen, M. & Nordestgaard, B. G. Coffee intake and risk of obesity, metabolic syndrome and type 2 diabetes: a Mendelian randomization study. Int. J. Epidemiol. 44, 551–565 (2015).
Kwok, M. K., Leung, G. M. & Schooling, C. M. Habitual coffee consumption and risk of type 2 diabetes, ischemic heart disease, depression and Alzheimer’s disease: a Mendelian randomization study. Sci. Rep. 6, 36500 (2016).
Schwingshackl, L., Chaimani, A., Hoffmann, G., Schwedhelm, C. & Boeing, H. A network meta-analysis on the comparative efficacy of different dietary approaches on glycaemic control in patients with type 2 diabetes mellitus. Eur. J. Epidemiol. 33, 157–170 (2018).
Estruch, R. et al. Effect of a high-fat Mediterranean diet on bodyweight and waist circumference: a prespecified secondary outcomes analysis of the PREDIMED randomised controlled trial. Lancet Diabetes Endocrinol. 4, 666–676 (2016).
Salas-Salvado, J. et al. Reduction in the incidence of type 2 diabetes with the Mediterranean diet: results of the PREDIMED-Reus nutrition intervention randomized trial. Diabet. Care 34, 14–19 (2011).
Kodama, S. et al. Influence of fat and carbohydrate proportions on the metabolic profile in patients with type 2 diabetes: a meta-analysis. Diabet. Care 32, 959–965 (2009).
Schwingshackl, L. & Hoffmann, G. Comparison of the long-term effects of high-fat v. low-fat diet consumption on cardiometabolic risk factors in subjects with abnormal glucose metabolism: a systematic review and meta-analysis. Br. J. Nutr. 111, 2047–2058 (2014).
Bazzano, L. A. et al. Effects of low-carbohydrate and low-fat diets: a randomized trial. Ann. Intern. Med. 161, 309–318 (2014).
Gardner, C. D. et al. Effect of low-fat vs low-carbohydrate diet on 12-month weight loss in overweight adults and the association with genotype pattern or insulin secretion: the DIETFITS randomized clinical trial. JAMA 319, 667–679 (2018).
Hallberg, S. J. et al. Effectiveness and safety of a novel care model for the management of type 2 diabetes at 1 year: an open-label, non-randomized, controlled study. Diabetes Ther. 9, 583–612 (2018).
Ghaedi, E. et al. Effects of a Paleolithic diet on cardiovascular disease risk factors: a systematic review and meta-analysis of randomized controlled trials. Adv. Nutr. 10, 634–646 (2019).
Hoffman, R. & Gerber, M. Food processing and the Mediterranean diet. Nutrients 7, 7925–7964 (2015).
Louzada, M. L. et al. Consumption of ultra-processed foods and obesity in Brazilian adolescents and adults. Prev. Med. 81, 9–15 (2015).
Dobarganes, C. & Marquez-Ruiz, G. Possible adverse effects of frying with vegetable oils. Br. J. Nutr. 113, S49–57 (2015).
Zinocker, M. K. & Lindseth, I. A. The Western diet-microbiome-host interaction and its role in metabolic disease. Nutrients 10, 365 (2018).
Monteiro, C. A., Moubarac, J. C., Cannon, G., Ng, S. W. & Popkin, B. Ultra-processed products are becoming dominant in the global food system. Obes. Rev. 14, 21–28 (2013).
da Silva Oliveira, M. S. & Silva-Amparo, L. Food-based dietary guidelines: a comparative analysis between the dietary guidelines for the Brazilian population 2006 and 2014. Public Health Nutr. 21, 210–217 (2018).
Luevano-Contreras, C., Gomez-Ojeda, A., Macias-Cervantes, M. H. & Garay-Sevilla, M. E. Dietary advanced glycation end products and cardiometabolic risk. Curr. Diabet. Rep. 17, 63 (2017).
Vlassara, H. et al. Oral AGE restriction ameliorates insulin resistance in obese individuals with the metabolic syndrome: a randomised controlled trial. Diabetologia 59, 2181–2192 (2016).
Arranz, E. & Corredig, M. Invited review: Milk phospholipid vesicles, their colloidal properties, and potential as delivery vehicles for bioactive molecules. J. Dairy Sci. 100, 4213–4222 (2017).
Bourlieu, C. et al. Polar lipid composition of bioactive dairy co-products buttermilk and butterserum: emphasis on sphingolipid and ceramide isoforms. Food Chem. 240, 67–74 (2018).
Brunkwall, L. & Orho-Melander, M. The gut microbiome as a target for prevention and treatment of hyperglycaemia in type 2 diabetes: from current human evidence to future possibilities. Diabetologia 60, 943–951 (2017).
Canfora, E. E., Meex, R. C. R., Venema, K. & Blaak, E. E. Gut microbial metabolites in obesity, NAFLD and T2DM. Nat. Rev. Endocrinol. 15, 261–273 (2019).
Davani-Davari, D. et al. Prebiotics: definition, types, sources, mechanisms, and clinical applications. Foods 8, 92 (2019).
Yoo, J. Y. & Kim, S. S. Probiotics and prebiotics: present status and future perspectives on metabolic disorders. Nutrients 8, 173 (2016).
Reese, A. T. & Carmody, R. N. Thinking outside the cereal box: noncarbohydrate routes for dietary manipulation of the gut microbiota. Appl. Environ. Microbiol. 85, e02246-18 (2019).
Suez, J., Korem, T., Zilberman-Schapira, G., Segal, E. & Elinav, E. Non-caloric artificial sweeteners and the microbiome: findings and challenges. Gut Microbes 6, 149–155 (2015).
Pearlman, M., Obert, J. & Casey, L. The association between artificial sweeteners and obesity. Curr. Gastroenterol. Rep. 19, 64 (2017).
Pepino, M. Y. Metabolic effects of non-nutritive sweeteners. Physiol. Behav. 152, 450–455 (2015).
Nichol, A. D., Holle, M. J. & An, R. Glycemic impact of non-nutritive sweeteners: a systematic review and meta-analysis of randomized controlled trials. Eur. J. Clin. Nutr. 72, 796–804 (2018).
Tey, S. L., Salleh, N. B., Henry, J. & Forde, C. G. Effects of aspartame-, monk fruit-, stevia- and sucrose-sweetened beverages on postprandial glucose, insulin and energy intake. Int. J. Obes. 41, 450–457 (2017).
Ludwig, D. S. Artificially sweetened beverages: cause for concern. JAMA 302, 2477–2478 (2009).
Halmos, E. P., Mack, A. & Gibson, P. R. Review article: emulsifiers in the food supply and implications for gastrointestinal disease. Aliment Pharmacol. Ther. 49, 41–50 (2019).
Chassaing, B. et al. Dietary emulsifiers impact the mouse gut microbiota promoting colitis and metabolic syndrome. Nature 519, 92–96 (2015).
Chassaing, B., Van de Wiele, T., De Bodt, J., Marzorati, M. & Gewirtz, A. T. Dietary emulsifiers directly alter human microbiota composition and gene expression ex vivo potentiating intestinal inflammation. Gut 66, 1414–1427 (2017).
Beauchamp, G. K. et al. Phytochemistry: ibuprofen-like activity in extra-virgin olive oil. Nature 437, 45–46 (2005).
Scotece, M. et al. New drugs from ancient natural foods. Oleocanthal, the natural occurring spicy compound of olive oil: a brief history. Drug Discov. Today 20, 406–410 (2015).
Guo, X., Yang, B., Tan, J., Jiang, J. & Li, D. Associations of dietary intakes of anthocyanins and berry fruits with risk of type 2 diabetes mellitus: a systematic review and meta-analysis of prospective cohort studies. Eur. J. Clin. Nutr. 70, 1360–1367 (2016).
Xu, H., Luo, J., Huang, J. & Wen, Q. Flavonoids intake and risk of type 2 diabetes mellitus: a meta-analysis of prospective cohort studies. Medicine 97, e0686 (2018).
Mulvihill, E. E. et al. Naringenin prevents dyslipidemia, apolipoprotein B overproduction, and hyperinsulinemia in LDL receptor-null mice with diet-induced insulin resistance. Diabetes 58, 2198–2210 (2009).
Hoek-van den Hil, E. F. et al. Quercetin decreases high-fat diet induced body weight gain and accumulation of hepatic and circulating lipids in mice. Genes Nutr. 9, 418 (2014).
Tsutsumi, R. et al. Sudachitin, a polymethoxylated flavone, improves glucose and lipid metabolism by increasing mitochondrial biogenesis in skeletal muscle. Nutr. Metab. 11, 32 (2014).
Zhang, X. et al. Dietary luteolin activates browning and thermogenesis in mice through an AMPK/PGC1alpha pathway-mediated mechanism. Int. J. Obes. 40, 1841–1849 (2016).
Kawser Hossain, M. et al. Molecular mechanisms of the anti-obesity and anti-diabetic properties of flavonoids. Int. J. Mol. Sci. 17, 569 (2016).
Warner, E. F. et al. Common phenolic metabolites of flavonoids, but not their unmetabolized precursors, reduce the secretion of vascular cellular adhesion molecules by human endothelial cells. J. Nutr. 146, 465–473 (2016).
Heianza, Y. & Qi, L. Gene-diet interaction and precision nutrition in obesity. Int. J. Mol. Sci. 18, 787 (2017).
Ortega, A., Berna, G., Rojas, A., Martin, F. & Soria, B. Gene-diet interactions in type 2 diabetes: the chicken and egg debate. Int. J. Mol. Sci. 18, 1188 (2017).
Ordovas, J. M., Ferguson, L. R., Tai, E. S. & Mathers, J. C. Personalised nutrition and health. BMJ 361, bmj.k2173 (2018).
de Toro-Martin, J., Arsenault, B. J., Despres, J. P. & Vohl, M. C. Precision nutrition: a review of personalized nutritional approaches for the prevention and management of metabolic syndrome. Nutrients 9, 913 (2017).
Christensen, L., Roager, H. M., Astrup, A. & Hjorth, M. F. Microbial enterotypes in personalized nutrition and obesity management. Am. J. Clin. Nutr. 108, 645–651 (2018).
Kabisch, S. et al. Fasting glucose state determines metabolic response to supplementation with insoluble cereal fibre: a secondary analysis of the optimal fibre trial (OptiFiT). Nutrients 11, 2385 (2019).
Hjorth, M. F. et al. Pretreatment fasting glucose and insulin as determinants of weight loss on diets varying in macronutrients and dietary fibers-the POUNDS LOST study. Nutrients 11, 586 (2019).
Mirrahimi, A. et al. Associations of glycemic index and load with coronary heart disease events: a systematic review and meta-analysis of prospective cohorts. J. Am. Heart Assoc. 1, e000752 (2012).
Dong, J. Y., Zhang, Z. L., Wang, P. Y. & Qin, L. Q. Effects of high-protein diets on body weight, glycaemic control, blood lipids and blood pressure in type 2 diabetes: meta-analysis of randomised controlled trials. Br. J. Nutr. 110, 781–789 (2013).
Viana, L. V., Gross, J. L. & Azevedo, M. J. Dietary intervention in patients with gestational diabetes mellitus: a systematic review and meta-analysis of randomized clinical trials on maternal and newborn outcomes. Diabet. Care 37, 3345–3355 (2014).
Zeevi, D. et al. Personalized nutrition by prediction of glycemic responses. Cell 163, 1079–1094 (2015).
Korem, T. et al. Bread affects clinical parameters and induces gut microbiome-associated personal glycemic responses. Cell Metab. 25, 1243–1253 (2017).
Rothschild, D. et al. Environment dominates over host genetics in shaping human gut microbiota. Nature 555, 210–215 (2018).
Hjorth, M. F. et al. Prevotella-to-Bacteroides ratio predicts body weight and fat loss success on 24-week diets varying in macronutrient composition and dietary fiber: results from a post-hoc analysis. Int. J. Obes. 43, 149–157 (2019).
Artinian, N. T. et al. Interventions to promote physical activity and dietary lifestyle changes for cardiovascular risk factor reduction in adults: a scientific statement from the American Heart Association. Circulation 122, 406–441 (2010).
Spring, B. et al. Better population health through behavior change in adults: a call to action. Circulation 128, 2169–2176 (2013).
Celis-Morales, C. et al. Effect of personalized nutrition on health-related behaviour change: evidence from the Food4Me European randomized controlled trial. Int. J. Epidemiol. 46, 578–588 (2017).
Capewell, S. & O’Flaherty, M. Rapid mortality falls after risk-factor changes in populations. Lancet 378, 752–753 (2011).
McGill, R. et al. Are interventions to promote healthy eating equally effective for all? Systematic review of socioeconomic inequalities in impact. BMC Public Health 15, 457 (2015).
Guzman-Castillo, M. et al. The contribution of primary prevention medication and dietary change in coronary mortality reduction in England between 2000 and 2007: a modelling study. BMJ Open 5, e006070 (2015).
Mozaffarian, D. in Rising Health Care Costs: Drivers, Challenges and Solutions 8–25 (NAIC & CIPR, 2018).
Huang, Y. et al. Adoption and design of emerging dietary policies to improve cardiometabolic health in the US. Curr. Atheroscler. Rep. 20, 25 (2018).
Swinburn, B. A. et al. The global syndemic of obesity, undernutrition, and climate change: the Lancet commission report. Lancet 393, 791–846 (2019).
Mozaffarian, D. et al. Population approaches to improve diet, physical activity, and smoking habits: a scientific statement from the American Heart Association. Circulation 126, 1514–1563 (2012).
Li, F. et al. Built environment and 1-year change in weight and waist circumference in middle-aged and older adults: Portland Neighborhood Environment and Health Study. Am. J. Epidemiol. 169, 401–408 (2009).
Powell, L. M. & Bao, Y. Food prices, access to food outlets and child weight. Econ. Hum. Biol. 7, 64–72 (2009).
Boone-Heinonen, J. et al. Fast food restaurants and food stores: longitudinal associations with diet in young to middle-aged adults: the CARDIA study. Arch. Intern. Med. 171, 1162–1170 (2011).
Block, J. P., Christakis, N. A., O’Malley, A. J. & Subramanian, S. V. Proximity to food establishments and body mass index in the Framingham Heart Study offspring cohort over 30 years. Am. J. Epidemiol. 174, 1108–1114 (2011).
Gibson, D. M. The neighborhood food environment and adult weight status: estimates from longitudinal data. Am. J. Public Health 101, 71–78 (2011).
Shier, V., An, R. & Sturm, R. Is there a robust relationship between neighbourhood food environment and childhood obesity in the USA? Public Health 126, 723–730 (2012).
Wang, R. & Shi, L. Access to food outlets and children’s nutritional intake in urban China: a difference-in-difference analysis. It. J. Pediatrics 38, 30 (2012).
Boone-Heinonen, J. et al. The neighborhood energy balance equation: does neighborhood food retail environment + physical activity environment = obesity? The CARDIA study. PLoS ONE 8, e85141 (2013).
Smith, D., Cummins, S., Clark, C. & Stansfeld, S. Does the local food environment around schools affect diet? Longitudinal associations in adolescents attending secondary schools in East London. BMC Public Health 13, 700 (2013).
Cummins, S., Flint, E. & Matthews, S. A. New neighborhood grocery store increased awareness of food access but did not alter dietary habits or obesity. Health Affairs (Project Hope) 33, 283–291 (2014).
Elbel, B. et al. Assessment of a government-subsidized supermarket in a high-need area on household food availability and children’s dietary intakes. Public Health Nutr. 18, 2881–2890 (2015).
Dubowitz, T. et al. Diet and perceptions change with supermarket introduction in a food desert, but not because of supermarket use. Health Affairs (Project Hope) 34, 1858–1868 (2015).
Ghosh-Dastidar, M. et al. Does opening a supermarket in a food desert change the food environment? Health Place 46, 249–256 (2017).
Haspel, T. Food deserts don’t cause obesity. But that doesn’t mean they don’t matter. Washington Post (August 2018).
Sustainable Development Goals: 17 Goals to Transform our World (UN, 2015).
WHO Framework Convention on Tobacco Control (WHO, 2019).
Silver, L. Sugary drink taxes – the new normal. World Cancer Research Fund International (June 2018).
Mozaffarian, D., Rogoff, K. S. & Ludwig, D. S. The real cost of food: can taxes and subsidies improve public health? JAMA 312, 889–890 (2014).
Pomeranz, J., Mozaffarian, D. & Micha, R. Mandating front-of-package food labels in the U. S. – What are the First Amendment obstacles? Food Policy 86, https://doi.org/10.1016/j.foodpol.2019.05.005 (2019).
Jacobs, A. In sweeping war on obesity, Chile slays Tony the tiger. New York Times (February 2018).
Food Directions LLC. Restrictions of Food Marketing and Advertisements Aimed at Children https://fooddirectionsllc.com/2017/02/06/restrictions-of-food-marketing-and-advertisements-aimed-at-children/ (2017).
Association of National Advertisers. Three New International Food Advertising Restrictions https://www.ana.net/content/show/id/42549 (2019).
USFDA. Trans Fat https://www.fda.gov/food/food-additives-petitions/trans-fat (2018).
Hyseni, L. et al. Systematic review of dietary salt reduction policies: Evidence for an effectiveness hierarchy? PLoS ONE 12, e0177535 (2017).
Flor, R. Focusing on “Protective Foods” to Reduce the Global Burden of Disease. Rockefeller Foundation (April 2019).
Acknowledgements
D.M. acknowledges support from the National Health, Lung, and Blood Institute (grant no. R01 HL115189), National Institutes of Health. D.M. also acknowledges research funding from the National Institutes of Health and the Gates Foundation; personal fees from GOED, Nutrition Impact, Pollock Communications, Bunge, Indigo Agriculture, Amarin, Acasti Pharma, Cleveland Clinic Foundation, America’s Test Kitchen, and Danone; scientific advisory board, Brightseed, DayTwo, Elysium Health and Filtricine; and chapter royalties from UpToDate—all outside the submitted work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Tufts University holds patents US8889739 and US9987243 (unlicensed), listing D.M. as a co-inventor, for use of trans-palmitoleic acid to prevent and treat insulin resistance, type 2 diabetes and related conditions, as well as reduce metabolic risk factors.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mozaffarian, D. Dietary and policy priorities to reduce the global crises of obesity and diabetes. Nat Food 1, 38–50 (2020). https://doi.org/10.1038/s43016-019-0013-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s43016-019-0013-1
This article is cited by
-
Nutrition and movement to improve quality of life in patients with knee osteoarthritis: the NUMOQUA study protocol for a randomised controlled trial
Trials (2024)
-
Effect of mobile food environments on fast food visits
Nature Communications (2024)
-
How does the updated Nutri-Score discriminate and classify the nutritional quality of foods in a Norwegian setting?
International Journal of Behavioral Nutrition and Physical Activity (2023)
-
The diet rapidly and differentially affects the gut microbiota and host lipid mediators in a healthy population
Microbiome (2023)
-
Climate change exacerbates nutrient disparities from seafood
Nature Climate Change (2023)